Abstract
Background
Laryngeal mask airway (LMA) CTrach has an integrated fiber optic bundle and battery-powered monitor that enable viewing the larynx. The LMA CTrach is a step in the evolution of LMA Fastrach. This study assessed the feasibility of the two types of LMA in anesthetized non-paralyzed patients.
Patients and methods
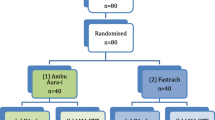
This is a randomized controlled study where patients were allocated into two equal groups (n = 40 each), LMA CTrach group and LMA Fastrach group. All patients were scheduled for elective surgeries requiring intubation. General anesthesia with sevoflurane was used without the use of a neuromuscular blocking agent. The success of intubation from the first attempt and overall success rate were recorded. Also, the time to achieve ventilation, the time for complete tracheal intubation, and the time of the whole procedure were recorded, and any side effects were noticed.
Results
Tracheal intubation was successful on the first attempt in 92.5% in the LMA CTrach group and in 67.5% in the LMA Fastrach group. The success rate within three attempts was 100% in the LMA CTrach group and 95% in the LMA Fastrach group. The time for tracheal intubation and the time of the whole procedure are significantly longer with the LMA CTrach group than the LMA Fastrach group (P < 0.002).
Conclusion
LMA CTrach produced a high first-attempt success rate of tracheal intubation; meanwhile, the time for intubation and the whole procedure times were longer. Complications of both groups were minimal.
Similar content being viewed by others
Introduction
Most cases of unexpected difficult intubation are managed satisfactorily by direct laryngoscope. Associated problems with tracheal intubation are soft tissue damage and marked sympathoadrenal response. Although hemodynamic alterations are short lived, they can be specifically important in patients with myocardial or cerebral insufficiency. Alternative guiding devices for intubation were inaugurated such as fiber optic scope, light wand, and intubating laryngeal mask airways (LMA) (Mohammed et al. 2014).
The laryngeal mask airway (LMA) Fastrach allows ventilation and provides simple maneuver for blind tracheal intubation. However, intubation could fail despite multiple attempts (Baskett et al. 1998).
The LMA CTrach is functionally identical to the LMA Fastrach but has an integrated fiber optic bundle that enables viewing of the larynx through a battery-powered monitor that lies at the top of the CTrach LMA and is attached to it via a magnetic latch connector (Arslan et al. 2009). Intubating LMA has been used for tracheal intubation with many methods: after administration of neuromuscular blocking drugs, awake insertion of the mask followed by intubation using high concentration of sevoflurane, or awake intubation using topical anesthesia (Liu et al. 2006; Lopez et al. 2009). All these methods have their own limitations. The administration of a neuromuscular blocking drug may not be preferable in patients with an anticipated difficult airway. High concentration of inhalational anesthetic may lead to cardiovascular and cerebrovascular compromise in susceptible patients. Awake insertion of LMA cannot be performed without patient cooperation (Chlkoti et al. 2012).
In the anesthetic practice with cancer patients, it is not uncommon to face situations where patients complain heavy tumor burden in the head and neck area or patients with significant psychological morbidity. These patients are expected to be uncooperative and airway difficulty is anticipated. The hypothesis of this study was that if intubation can be performed through LMA using moderate concentration of an anesthetic agent but without the use of muscle relaxant in normal patients without anticipated difficulty, it would be a useful alternative in intubating the abovementioned uncooperative patients with anticipated difficult intubation.
The aim of this study was to assess the feasibility of two different types of intubating LMA in anesthetized unparalysed patients. Moreover, their comparison regarding the success rate of intubation, corrective maneuvers needed, and the procedure-related complications were to be assessed.
Patients and methods
After approval from the local ethics committee and informed written consent, 80 patients of American Society of Anesthesiologists (ASA) grade I/II scheduled for elective surgeries in Mansoura University Hospitals, Egypt, requiring orotracheal intubation were studied. Patients who had body mass indices greater than 35 kg/m2 and patients having limited mouth opening < 25 mm, oropharyngeal pathology, or risk of regurgitation or pulmonary aspiration of gastric contents were excluded from the study. Mallampatti grading (MPG), thyromental distance (TMD), and neck circumference (NC) were used to assess the airway of all patients. Patients were kept fasting overnight and were given tab diazepam 10 mg in the night before surgery and 5 mg just 2 h before induction of anesthesia. Patients were randomly assigned using a closed envelope method into two groups: LMA Fastrach group and LMA CTrach group. The observer who collected that data was blinded to patients’ group.
Standard intraoperative monitoring included continuous ECG (electrocardiography), non-invasive blood pressure, and pulse oximetry. Difficult airway set was kept ready to manage any difficult airway situation. The LMA Fastrach and the LMA CTrach laryngeal mask airway size was chosen according to the patients’ body weight in accordance with the manufacturer recommendation (LMA Fastrach Instruction Manual Henkey on Thames 2001; LMA CTrach Instruction Manual 2004): LMA size 3 and a 7.0-mm ID endotracheal tube for patients with body weight below 50 kg, a size 4 airway and 7.5 mm endotracheal tube for patients with body weight 50–70 kg, and a size 5 airway and 8.0 mm endotracheal tube for patients with body weight over 70 kg. Anesthesia was induced with intravenous fentanyl 1μg/kg and sevoflurane. A neuromuscular blocking agent was not used. Anesthesia was considered adequate for LMA insertion when the patient was unresponsive, and steady-state end-tidal concentration of 2% sevoflurane was achieved. Nondisposable, flexible, cuffed, wire-reinforced LMA Fastrach tracheal tubes were used for all patients. The viewer was focused before using the LMA CTrach and was not adjusted any further during the procedure. The patients’ heads were supported on donut and kept in a neutral posture. The LMA Fastrach or LMA CTrach was inserted and adjusted, and tracheal intubation was performed with minimal neck movement. All patients were monitored carefully to ensure that oxygen saturation did not decrease below 95% at any time.
In the LMA Fastrach group, LMA Fastrach was inserted, its cuff was inflated, and the ability to ventilate the lungs was checked. If ventilation was difficult, the “up-down maneuver” was applied by withdrawing the mask by 6 cm and reinserting it, with the cuff still inflated. If this failed, partial withdrawal of the mask was tried, and if this also failed, the LMA was completely removed and reinserted. After optimizing ventilation, the metal handle was used to slightly lift the LMA Fastrach away from the posterior pharyngeal wall. If there was resistance to the passage of the endotracheal tube, corrective measures were applied based on the depth of endotracheal tube insertion at which resistance was encountered (Ferson et al. 2001). If resistance was felt after advancing the endotracheal tube 2–2.5 cm beyond the distal opening of the LMA Fastrach, the up and down maneuver was applied. If resistance was felt within 1 cm when trying to advance the endotracheal tube, a smaller LMA Fastrach was used. If resistance was felt after advancing the endotracheal tube 3 cm beyond the distal opening, a larger LMA Fastrach was used. Lungs were ventilated in between attempts. Correct position of the endotracheal tube was confirmed with end-tidal capnography, and then the LMA Fastrach was removed over the endotracheal tube with the aid of the stabilizer rod. Up to three attempts were allowed; after which, tracheal intubation was performed using a Macintosh laryngoscope.
In LMA CTrach group, lung ventilation was optimized after insertion of the LMA CTrach using the same sequence of maneuvers as with the LMA Fastrach starting with the up and down maneuver. Then, the viewer was connected and the view of the laryngeal structures was noted. After the vocal cords were visualized, a small-sized suction catheter was passed through the CTrach which could be easily seen on the viewer and 2 ml of 2% lignocaine was instilled over the vocal cords through the catheter. After waiting for 2 min, a lubricated endotracheal tube was passed through the rigid anatomically curved airway tube of the CTrach. During these 2 min, ventilation was assisted in all patients. The correct tube placement was confirmed by direct visualization, chest auscultation, and capnography. After confirmation of the tracheal intubation, the CTrach was removed according to the manufacturer’s instructions. Whenever the laryngeal view was partial, various adjusting maneuvers were used to improve the view depending on the likely cause of failure. Three types of corrective manoeuvers were used: Down-Up-Down (DUD), medial-lateral-medial (MLM), and Chandy’s manoeuvers. The purpose of Chandy’s maneuver is to optimize the success of “blind” tracheal intubation when using LMA Fastrach. It is noteworthy that if visualization of the glottis failed with LMA CTrach, it was used as LMA Fastrach for “blind” tracheal intubation. The two steps of the Chandy’s maneuver are performed sequentially. After insertion of the LMA-Fastrach or LMA CTrach, optimal ventilation is established by slightly rotating the device in the sagittal plane, using the metal handle, until the least resistance to bag ventilation is achieved. This helps to align the internal aperture of the device with the glottic opening. Just before intubation, the LMA-CTrach is slightly lifted (but not tilted) away from the posterior pharyngeal wall using the metal handle. This prevents the endotracheal tube (ETT) from colliding with the arytenoids and facilitates the smooth passage of the ETT into the trachea. The tracheal intubation was considered failed if trachea could not be intubated in three attempts. In this situation, intubation was performed using a Macintosh laryngoscope.
Monitoring included the following items:
-
The number of LMA trials was recorded; the success rate of intubation from the first attempt, overall success rate of intubation, and failure after the third attempt were all recorded. The procedure-related durations were also assessed; the time required to achieve ventilation (from the time of holding LMA until the capnographic confirmation of adequate lung ventilation), the time required for intubation, and the time taken for the whole procedure (included the whole steps till the removal of the LMA) were recorded. The ease of technique was assessed on a 4-point scale as easy, adjusting manoeuvers required, reinsertion required, or failure at third attempt (Healy et al. 2012).
-
Heart rate (HR) and blood pressure were recorded after induction, after insertion of LMA, 1-min after induction, and 3-min after induction. Any complications occurring following the LMA insertion or tracheal intubation, e.g., coughing, bucking, or bronchospasm, and those in the post-operative period, e.g., dysphagia, hoarseness of voice, sore throat, nausea, or vomiting were recorded.
Statistical analysis
Data was analyzed using SPSS (Statistical Package for the Social Science) version 15 (SPSS Inc. Chicago, IL). It was estimated that a sample size of more than 36 patients per group would achieve a power of 90% with type 1 error 0.05. Qualitative data were presented as number and percent. Comparison between groups was done by chi-Square test. Quantitative data were tested for normality by Kolmogorov–Smirnov test. Normally distributed data were presented as mean (SD). Student t test was used to compare between two groups. P value (calculated probability) < 0.05 was considered statistically significant.
Results
The study included 80 patients requiring orotracheal intubation and scheduled for elective surgery. Patients were randomly assigned into two groups: LMA Fastrach group and LMA CTrach group (Fig. 1).
There was no significant difference in the demographic data for the two studied groups (Table 1). The success rate of intubation on the first attempt was significantly higher in the CTrach group (92.5%) compared to the Fastrach group (67.5%). The overall success rates of tracheal intubation were 100% in the LMA CTrach and 95% in the LMA Fastrach group. Intubation failed in two patients in the LMA Fastrach group, and tracheal intubation was done with the Macintosh laryngoscope. As regards the ease of the technique, it was easy in 16 patients of the LMA Fastrach group and 12 patients of the LMA CTrach group while corrective maneuvers required to optimize ventilation were needed in 24 (60%) patients in the LMA Fastrach group and 28 (70%) patients in the LMA CTrach group (Table 2).
The time for complete tracheal intubation and the total time for the whole procedure of LMA insertion, tracheal intubation, and removal of the mask were significantly longer in the LMA CTrach group in comparison to the LMA Fastrach group; meanwhile, the time to achieve ventilation was comparable in the two studied groups (Table 3).
Heart rate increased significantly following insertion of CTrach compared to the induction value (P < 0.05); otherwise, there was no statistically significant difference in hemodynamic parameters among patients of the two groups (Table 4). Postoperative complications were not significantly different in the two studied groups; mucosal laceration as evidenced by staining of the mask or the endotracheal tube was observed in four patients of the LMA Fastrach group and three patients in the LMA CTrach group; five patients in Fastrach group complained hoarseness of voice and two patients suffered from sore throat and dysphagia (Table 5).
Discussion
In the current study, there was a higher success rate of intubation on the first attempt with the LMA CTrach compared to the LMA Fastrach which was in agreement with the result of Lieu et al. (Liu et al. 2008), despite the routine use of muscle relaxants in all patients in this study.
Both the LMA Fastrach and LMA CTrach have an evidenced role in difficult airway management, enabling ventilation and providing a conduit for tracheal intubation in a situation where both mask ventilation and conventional tracheal intubation are difficult (Ferson et al. 2001). Moreover, both of them provide a patent airway conduit to the glottis avoiding potential obstruction and permit the spontaneous or manual ventilation with 100% O2 decreasing the risk of rapid desaturation (Dimitriou et al. 2002). In this study, the success rate of intubation within three attempts was 100% in the CTrach group and 95% in the Fastrach group which is coincident with the study of Liu et al. (Liu et al. 2006) that reported high success rates of CTrach and endotracheal intubation through it with minimal neck movement.
The fiber optic bronchoscope has been used in combination with LMA Fastrach to improve the success rate of tracheal intubation (Dimitriou et al. 2002). It can improve the first attempt success and reduce the risk of esophageal intubation and laryngeal trauma but will add to the complexity of airway management. In comparison, the LMA CTrach system is completely portable, can easily be handled by a single operator, and requires less preparation time than fiberoptic bronchoscope (Liu et al. 2008).
Corrective maneuvers were needed in both groups to achieve a full or partial view of the vocal cords that consumed more time in few cases. Timmermann et al. (Timmermann et al. 2006) stated that there are both anatomical and technical reasons that limit the image quality obtained using the LMA CTrach. As observed in the anesthetized patient, the most common anatomical factor was downfolding of the epiglottis, or contact with the lenses that can be successfully corrected (Liu et al. 2006). Concerning the technical reasons, the small lenses are easily obstructed by secretions or fogging during insertion or manipulation, requiring removal, cleaning, and reinsertion of the mask. This can be avoided by appropriate protection of the fiberoptic before insertion or, alternatively, cleaning the lenses with a swab inserted through the channel (Maurtua et al. 2007). The time for intubation and successful ventilation was prolonged to some extent with the LMA CTrach than LMA Fastrach. This was reported in an earlier study (Arslan et al. 2009) that found that CTrach was associated with the prolonged view and intubation time. Liu et al. (Liu et al. 2008) confirmed these results as they reported that CTrach increased the time to achieve intubation and adequate ventilation. Also, Lopez et al. (Lopez et al. 2009) compared LMA CTrach with the fiber optic laryngoscope and concluded that the time required for intubation with CTrach may be longer than that with the fiberoptic laryngoscope. However, LMA CTrach is easy to use and well tolerated (Dhonneur et al, 2006).
In the present study, there was no significant difference between the two groups regarding MABP and HR. Elnaghy and Yuste (Elnaghy and Yuste 2015) concluded that the use of CTrach failed to get any advantage in attenuating the hemodynamic response during tracheal intubation. Similarly, Sharma e al. (Sharma et al. 2013) reported no significant hemodynamic changes in patients intubated with LMA Fastrach.
The complaint from the airway was a little bit more in the Fastrach group than in the CTrach group. This may be due to the more attempts needed to achieve intubation with the LMA Fastrach; also, the blind attempts with the Fastrach may traumatize the airway.
Conclusion
In conclusion, both LMA CTrach and LMA Fastrach achieved an overall satisfactory success rate of intubation in anesthetized non-paralyzed patients. The LMA CTrach achieved higher overall success rate and high rates of success on the first attempt though it was associated with longer duration. Theoretically, both techniques could be useful tools in anesthetizing uncooperative patients with an anticipated difficult airway.
Abbreviations
- ASA:
-
American society of Anesthesiology
- DUD:
-
Down-Up-Down
- ECG:
-
Electrocardiography
- ETT:
-
Endotracheal tube
- HR:
-
Heart rate
- LMA:
-
Laryngeal mask airway
- MABP:
-
Mean arterial blood pressure
- MLM:
-
Medial-lateral-medial
- MPG:
-
Mallampati grading
- NCL:
-
Neck circumference
- SD:
-
Standard deviation
- SPSS:
-
Statistical Package for Social Science
- TMD:
-
Thyromental distance
References
Arslan ZI, Yildiz T, Baykara ZN et al (2009) Tracheal intubation in patients with rigid collar immobilization of the cervical spine: a comparison of Airtraq and LMA CTrach devices. Anesthesia 64:1332–1336
Baskett PJ, Parr MJ, Nolan JP (1998) The intubating laryngeal mask: results of a multicentre trial with experience of 500 cases. Anaesthesia 53:1174–1179
Chlkoti G, Mohta M, Kochhar A (2012) Intubation using LMA CTrach in anaesthetized but unparalysed patients – a pilot study. J Evol Med Dental Siences 1(4):422–429
Dhonneur G, Ndoko SK, Yavchitz A et al (2006) Tracheal intubation of morbidly obese patients: LMA CTrach vs direct laryngoscopy. Br J Anaesth 97:742–745
Dimitriou V, Voyagis GS, Brimacombe JR (2002) Flexible lightwand- guided tracheal intubation with the intubating laryngeal mask Fastrach in adults after unpredicted failed laryngoscope-guided tracheal intubation. Anesthesiology 96:296–299
Elnaghy KM, Yuste J (2015) Comparative study of airway management and hemodynamic response during intubation with two different video laryngoscopes (Glidescope versus intubating laryngeal mask CTrach). EC Anaesthesia 2(2):90–98
Ferson DZ, Rosenblatt WH, Johansen MJ et al (2001) Use of the intubating LMA-Fastrach in 254 patients with difficult to manage airways. Anesthesiology 95:1175–1181
Healy DW, Maties O, Hovord D et al (2012) A systemic review of the role of video- laryngoscopy in successful orotracheal intubation. BMC Anesthesiol:12–32
Liu EH, Goy R, Chen F (2006) The LMA CTrach, a new laryngeal mask airway for endotracheal intubation under vision: evaluation in 100 patients. Br J Anaesth 96:396–400
Liu EH, Goy RW, Lim Y et al (2008) Success of tracheal intubation with intubating laryngeal mask airways: a randomized trial of the LMA Fastrach and LMA CTrach. Anesthesiology 108:621–626
LMA CTrach Instruction Manual, Singapore, Laryngeal Mask Company, 2004, p9
LMA Fastrach Instruction Manual Henkey on Thames (2001) LMA International Services, p 7 15–7
Lopez AM, Valero R, Pons M et al (2009) Awake intubation using the LMA CTrach in patients with difficult airways. Anaesthesia 64:387–391
Maurtua MA, Maurtua DB, Zura A et al (2007) Improving intubation success using the CTrach laryngeal mask airway (letter). Anesthesiology 106:640–641
Mohammed S, Yadav D, Sharma UD et al (2014) Comparison of intubation by LMA CTrach vs intubation by direct laryngoscopy in patient with normal airway. Indian J Clin Anesth 1(1):1–10
Sharma MU, Gombar S, Gombar K et al (2013) Endotracheal intubation through the intubating laryngeal mask airway (LMA- Fastrach): a randomized study of LMA-Fastrach wire- reinforced silicon endotracheal tube versus conventional polyvinyl chloride tracheal tube. Indian J Anaesth 57:19–24
Timmermann A, Russo S, Natge U et al (2006) LMA CTrach: initial experiences in patients with difficult- to –manage airways. Anaesthesist 55:528–534
Funding
No funding. Costs were the responsibility of the authors and medications used in the study belong to Mansoura University Hospitals, Mansoura, Egypt, which is a public governmental organization.
Availability of data and materials
All data and materials are available on the main manuscript and additional information will be provided upon request.
Author information
Authors and Affiliations
Contributions
OTA is responsible for the data collection, data analysis, and writing of the manuscript. TMF is responsible for the data collection and helped in writing the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
After approval of the institutional ethical committee of the Faculty of Medicine, Mansoura University, informed consent was obtained from the patients.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Abdel Dayem, O.T., Farahat, T.M. Intubation using laryngeal mask airway CTrach and laryngeal mask airway Fastrach in anesthetized non-paralyzed patients: a randomized controlled study. Ain-Shams J Anesthesiol 11, 13 (2019). https://doi.org/10.1186/s42077-019-0029-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-019-0029-7