Abstract
Background: The introduction of SLNB has allowed accurate staging in early-stage breast carcinomas and has minimized the number of unnecessary ALNDs. Intraoperative frozen-section analysis is a fundamental component of the sentinel lymph node biopsy (SLNB) procedure. Some patients have positive nodes on frozen-section analysis and thus undergo a conventional axillary lymph node dissection (ALND) at the time of the SLNB. A few patients have negative nodes on frozen-section analysis but have subsequent evidence of metastases on final pathologic examination. The purpose of our study was 2-fold: to compare the hospital-related charges of patients undergoing staging by SLNB with those of patients undergoing conventional ALND and to assess whether the different outcomes associated with SLNB adversely affect the charges incurred with this procedure.
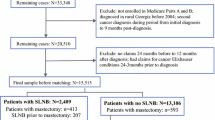
Methods: Our study group consisted of 100 patients with T1 breast cancer and breast conservation therapy who underwent either SLNB or ALND from July 1, 1997, to June 30, 1998. We identified the first 50 consecutive patients to undergo SLNB during this period. We chose a similar cohort of 50 patients for ALND. Mean hospital-related charges for the SLNB patients were categorized and compared with those for the ALND patients.
Results: Results for the two groups were analyzed using a two-sample Wilcoxon rank-sum test. Charges for the OR and hospital stay were less for the SLNB group (P<.05). Frozen-section analysis in the SLNB group contributed to the significant difference in charges for pathologic evaluation. Overall, the two groups showed no significant difference in total hospital-related charges.
Conclusions: When SLNB is used for T1 tumors, a small percentage of patients (10% in our study) will return to the operating room for an ALND. This small percentage does not increase the charges related to SLNB, however, as the reduced stay for most patients offsets this subgroup’s contribution to the total hospital-related charges. Thus, in patients with clinical stage I breast cancer, SLNB does not cause significantly higher hospital-related charges compared with conventional ALND.
Similar content being viewed by others
References
Rosen PP, Groshen S, Saigo P, Kinne DW, Hellman S. Pathological prognostic factors in stage I (T1N0M0) and stage II (T1N1M0) breast carcinoma: a study of 644 patients with median follow-up of 18 years.J Clin Oncol 1989;7:1239–51.
Kissin MW, Querci della Rovere G, Easton D, Westbury G. Risk of lymphoedema following the treatment of breast cancer.Br J Surg 1986;73:580–4.
Ivens D, Hoe AL, Podd TJ, Hamilton CR, Taylor I, Royle GT. Assessment of morbidity from complete axillary dissection.Br J Cancer 1992;66:136–8.
Rosen PP, Lesse ML, Kinne DW, Beattie EJ. Discontinuous or “skip” metastases in breast carcinoma. Analysis of 1228 axillary dissections.Ann Surg 1983;197:276–83.
Giuliano AE, Kirgan DM, Guenther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer.Ann Surg 1994;220:391–401.
Giuliano AE, Jones RC, Brennan M, Statman R. Sentinel lymphadenectomy in breast cancer.J Clin Oncol 1997;15:2345–50.
Veronesi U, Paganelli G, Galimberti V, et al. Sentinel-node biopsy to avoid axillary dissection in breast cancer with clinically negative lymph-nodes.Lancet 1997;349:1864–7.
Giuliano AE, Barth AM, Spivack B, Beitsch PD, Evans SW. Incidence and predictors of axillary metastases in T1 carcinoma of the breast.J Am Coll Surg 1996;183:185–9.
Albertini JJ, Lyman GH, Cox C, et al. Lymphatic mapping and SLNB in the patient with breast cancer.JAMA 1996;276:1818–22.
Krag D, Weaver D, Ashikaga T, et al. Sentinel node in breast cancer.N Engl J Med 1998;339:941–6.
Krag DN, Weaver DL, Alex JC, et al. Surgical resection and radiolocalization of the sentinel lymph node in breast cancer using gamma probe.Surg Oncol 1993;2:335–59.
O’Hea BJ, Hill ADK, El-Shirbiny AM, et al. Sentinel lymph node biopsy in breast cancer: the initial experience at Memorial Sloan-Kettering Cancer Center.J Am Coll Surg 1998;186:423–7.
Hill ADK, Tran KN, Akhurst T, et al. Lessons learned from 500 cases of lymphatic mapping for breast cancer.Ann Surg 1999;229:528–35.
Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma.Arch Surg 1992;127:392–9.
Reintgen D, Albertini J, Milliotes G, et al. Investment in new technology research can save future health care dollars.J Fla Med Assoc 1997;84:175–81.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gemignani, M.L., Cody, H.S., Fey, J.V. et al. Impact of sentinel lymph node mapping on relative charges in patients with early-stage breast cancer. Ann Surg Oncol 7, 575–580 (2000). https://doi.org/10.1007/BF02725336
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02725336