Abstract
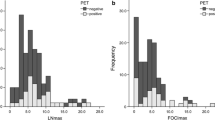
In 1989–90, all 37 lung cancer patients scheduled for surgery underwent transesophageal endoscopic ultrasonography (EUS) for pre-operative detection of hilar and mediastinal lymph node metastases. An electronic ultrasonic fiberscope with a linear array (EPB-503-FS, Machida-Toshiba) was used. Of 380 nodes surgically removed and that could have been detected by EUS, the detection rates for histologically metastatic and non-metastatic nodes were 65% (33 of 51) and 44% (144 of 329), respectively (p<0.01). Metastatic nodes were detected readily in every lymph node site, especially subaortic and subcarinal. Non-metastatic nodes were detected at low rates, especially in the superior mediastinum, paratracheal, and tracheobronchial locations. For greater long or short axes of the detected nodes, or for rounder nodes, the metastasis rate was higher. Detected nodes were classified into six types by their internal echo patterns; three were rarely metastatic (called “negative”) and the other three were often metastatic (called “positive”). Of the “negative” nodes histologically proved to be metastatic, metastasis was often diffuse. The “positive” nodes found to be metastatic tended to have one of two patterns of internal echoes when invasion was diffuse and a third pattern when it was localized. In an examination of the diagnostic usefulness of EUS, we made more correct diagnoses from the internal echo pattern than by reference to either the long or short axis alone. The short axes, node shape, and internal echoes were examined by Hayashi's second method of quantification. The sensitivity, specificity, and accuracy of the diagnoses were 85%, 84%, and 84%, respectively, superior to those by computed tomography done of the same patients.
Résumé
Pendant la période 1989/90, afin de déterminer l'existence de métastases ganglionnaires hilaires et/ou médiastinales, un examen échographique par voie endoscopique transesophagienne (EE) a été réalisé chez 37 patients consécutifs prévus pour une exérèse chirurgicale d'un cancer du poumon. On a utilisé un fibroscope électronique à ultrasons avec une sonde linéaire (EPB-503-FS). Des 380 ganglions lymphatiques vus en échographie et retirés chirurgicalement, une métastase a été diagnostiquée échographiquement dan 33 et confirmée histologiquement dans 51 cas (33/51=44%), alors que 144 des 329 ganglions indemnes de métastase étaient considérés comme tels par l'échographie (144/329=66%). L'échographie a pu détecter les métastases dans tous les groupes lymphatiques possibles, surtout dans les sites 5 et 7. L'échographie a pu innocenter très peu de ganglions, surtout dans les groupes 1, 2 et 4. Les métastases étaient plus fréquentes lorsque les ganglions étaient ronds et lorsque leurs axes principaux (vertical et horizontal) étaient allongés. On a classé les ganglions en six types selon leur échogénécité: trois étaient rarement métastatiques (appelés “négatifs”) et trois étaient souvent métastatiques (appelés “positifs”). Parmi les ganglions dits “negatifs” qui se sont avérés histologiquement métastaiques, la métastase était souvent diffuse. Lorsqu'un ganglion dit “positif” était réellement métastatique, l'invasion était diffuse dans deux types sur trois alors que c'était le troisème type d'échogénécité qui avait été observé lorsque l'invasion était localisée. En analyse finale, on a trouvé que la détermination du type d'échogénécité interne a été plus performante pour faire le diagnostic correct que l'augmentation de la taille des ganglions. Le plus petit axe des ganglions, la forme du ganglion et l'échogénécité interne ont été analysés selon la deuxième méthode de qunatification de Hayashi. La sensibilité, la spécificité, et la précision diagnostiques étaient respectivement de 85%, 84% et 84%, c'est à dire des chiffres supérieurs aux résultats obtenus pour la tomodensitométrie.
Resumen
En el período 1989–90 se realizó ultrasonografía endoscópica transesofágica (UET) en la totalidad de los pacientes programados para cirugía por cáncer pulmonar con el propósito de indentificar metástasis ganglíonares biliares y mediastinales, mediante un fibroscopio ultrasónico Machida — Toshiba EPB-503-FS. La tasa de detección para ganglios histológicamente metastásicos en los 380 ganglios resecados y que hybieran podido ser identificados mediante UET fue de 65% (33/51) y 44% (144/329), respectivamente (p<0.01). Los ganglios afectados pudieron ser fácilmente detectados en cada región ganglionar, especialmente en las ubicaciones 1, 2 y 4. La tasa de metástasis apareción incrementada en los ganglios de más largo eje longitudinal o transverso, o aquellos de estructura más redonda. Los ganglios así detectados fueron clasificados en seis tipos según sus patrones ecogénicos internos; tres tipos son raramente metastásicos (denominados “negativos”) y los otros tres con frecuencia son metastásicos (denominados “positivos”). En los ganglios “negativos” que histologicamente resultaron metastásicos, la metastásis generalmente fue del tipo difuso. Los ganglios “positivos” que demostraron ser matastásicos exhibieron tendencia hacía uno de dos patrones de ecogenicidad interna cuando la invasión era difusa y un tercer patrón cuando la invasión era localizada. Al analizar la utilidad diagnóstica de la UET, encontramos que el diagóstico correcto se derivó más a partir del patrón ecogénico interno que en relación a los ejes longitudinal y tranverso. Los ejes transversos, la forma del ganglio y los ecos internos fueron sujetos al segundo método de Hayashi de cuantificación. La sensibilidad, especificidad y certeza de los diagnósticos fue 85%, 84% y 84% respectivamente, lo cual es superior a lo que se logra mediante la tomografía computadorizada.
Similar content being viewed by others
References
Hermaneck, P., Sobin, L.H.: TNM Classification of Malignant Tumors, 4th edition, Geneva, International Union Against Cancer, 1987
Naruke, T., Suemasu, K., Ishikawa, S.: Lymph node mapping and curability at various levels of metastasis in resected lung cancer. J. Thorac. Cardiovasc. Surg.76:832, 1978
Hayashi, C.: On the quantification of qualitative data from the mathematico-statistical point of view. Ann. Inst. Statist. Math.2:35, 1950
Hayashi, C.: On the prediction of phenomena from qualitative data and the quantification of qualitative data from the mathematicostatistical point of view. Ann. Inst. Statist. Math.3:69, 1952
Watanabe, Y., Satoh, H., Iida S., Yamada, T., Magara T., Kobayashi, H., Tsunamura Y., Ichihashi, T., Iwa, T., Suzuki, M., Takashima T., Tonami, N., Matsubara, F., Kitagawa, M.: Accuracy of preoperative evaluation of T and N factors: Analysis of 330 thoracotomized cases (in Japanese). Haigan24:165, 1984
Yamashita, T., Tsubota, N., Aogaito, R., Yoshikawa, K., Nakamura K.: Evaluation of CT scan in diagnosis of mediastinal lymph node metastasis in lung cancer (in Japanese). Haigan27:149, 1987
Daly, B.D.T., Jr., Faling, L.J., Pugatch, R.D., Jung-Legg, Y., Gale, M.E., Bite, G., Snider, G.L.: Computed tomography. J. Thorac. Cardiovasc. Surg.88:486, 1984
Frazin L., Talano, J.V., Stephanides, L., Loeb, H.S., Kopel, L., Gunnar, R.M.: Esophageal echocardiography. Circulation54:102, 1976
Kobayashi, H., Danbara, T., Sugama, T., Saito, T., Kitamura, S., Kira, S.: Observation of lymph nodes and great vessels in the mediastinum by endoscopic ultrasonography. Jpn. J. Med.26:353, 1987
Kondo, D., Naruke, T., Kondo, H., Goya, T., Tsuchiya, R., Suemasu, K.: Endoscopic ultrasound examination for mediastinal lymph node metastases of lung cancer (in Japanese). Nippon Kokyuki Geka Gakkai Zasshi2:125, 1988
Sakio, H., Yamaguchi, Y.: Transesophageal endoscopic ultrasonography for preoperative assessment of the N-factor in lung cancer (in Japanese). Nippon Kokyuki Geka Gakkai Zasshi2:103, 1988
Murata, Y., Muroi, M., Yoshida, M., Okushima, N., Sugiyama, A., Ide, H., Yamada, A: Endoscopic ultrasonography in the diagnosis of esophageal carcinoma (in Japanese). Nippon Kikanshokudoka Gakkai Kaiho37:378, 1986
Koizumi, H.: Usefulness of endoscopic ultrasnonography for evaluating the depth of cancer invasion and the metastasis to the lymph nodes in patients with esophageal cancer (in Japanese). Osakashi Igakukai Zasshi37:151, 1988
Genereux, G.P., Howie, J.L.: Normal mediastinal lymph node size and number: CT and anatomical study. Am. J. Roentogenol.142:1095, 1984
Glazer, G.M., Gross, B.H., Quint, L.E., Francis, I.R., Bookstein, F.L., Orringer, M.B.: Normal mediastinal lymph nodes: Number and size according to American Thoracic Society Mapping. Am. J. Roentogenol.144:261, 1985
Quint, L.E., Glazer, G.M., Orringer, M.B., Francis, I.R., Bookstein, F.L.: Mediastinal lymph node detection and sizing at CT and autopsy. Am. J. Roentogenol.147:469, 1986
Libshitz, H.I., McKenna, R.J., Jr.: Mediastinal lymph node size in lung cancer. Am. J. Roentogenol.143:715, 1984
Patterson, G.A., Ginsberg, R.J., Poon, P.Y., Cooper, J.D., Goldberg M., Jones, D., Pearson, F.G., Todd, T.R., Waters, P., Bull, S.: A prospective evaluation of magnetic resonance imaging, computed tomography, and mediastinoscopy in the preoperative assessment of mediastinal node status in bronchogenic carcinoma. J. Thorac. Cardiovasc. Surg.94:679, 1987
Naruke, T., Goya, T., Tsuchiya, T., Suemasu, K.: Prognosis and survival in resected lung carcinoma based on the new international staging system. J. Thorac. Cardiovasc. Surg.96:440, 1988
Riquet, M., Hidden, G., Debesse, B.: Direct lymphatic drainage of lung segments to the mediastinal nodes. J. Thorac. Cardiovasc. Surg.97:623, 1989
Hata, E., Hayakawa, K., Miyamoto, H., Hayashida, R., Take, A., Fukushima, K., Hasegawa, T.: The incidence and the prognosis of contralateral mediastinal node involvement of the left lung cancer patients who underwent bilateral mediastinal dissection and pulmonary resection through the median sternotomy (in Japanese). Nippon Kyobu Rinsho48:275, 1989
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lee, N., Inoue, K., Yamamoto, R. et al. Patterns of internal echoes in lymph nodes in the diagnosis of lung cancer metastasis. World J. Surg. 16, 986–993 (1992). https://doi.org/10.1007/BF02067013
Issue Date:
DOI: https://doi.org/10.1007/BF02067013