Abstract
PURPOSE: Although many studies reported the association between high anal sphincter pressures and anal fissures, one question is open to date: is manometry really necessary for surgical management/does manometry influence the outcome? METHODS: Between October 1, 1990 and December 31, 1991, lateral sphincterotomy was performed in 177 patients with chronic anal fissure. In all patients the operation was performed as an outpatient procedure under local anesthetic. Electromanometry of the anal canal was carried out preoperatively to demonstrate the raised resting pressure profile within the anal canal. At the same time the maximum squeezing pressure was determined by electromanometry, and electromyography was performed to detect dysfunction of the external sphincter or the levators. The control group consisted of 14 proctologically healthy patients with a resting pressure of 74.4±8.9 and a maximum squeezing pressure of 130.2±15 (cm H2O). On the basis of resting pressures determined in healthy patients, an upper limit of 90 was defined as normal, taking into account the standard deviation and standard error rate. For statistical comparison patients were divided into two groups, retrospectively. All patients in Group A had a resting pressure of ≤90, and all patients in Group B had a resting pressure of >90. Six weeks after operation electromanometry was again performed to determine the resting pressure profile and maximum squeezing pressure of the sphincter system, and patients were examined to determine whether the fissure had healed. RESULTS: As a result of the lateral sphincterotomy, the resting pressure was lowered in all patients from 106.6±21.5 to 80.9±10.4 and maximum squeezing pressure from 149.3±27.6 to 135.3±27.2. Both results were highly significant (P<0.001, chisquared). Regarding either reduction in postoperative resting pressure or continence, Groups A and B did not differ statistically. In Group A soiling occurred in 3.2 percent and Grade 1 incontinence in 3.2 percent (1 patient each), and in Group B only one patient (0.7 percent) complained of soiling. Recurrences occurred in 9.7 percent of patients in Group A and in 2.1 percent of patients in Group B (3 patients in each case). CONCLUSION: Electromanometric examinations showed that internal sphincterotomy significantly reduces pressure within the anal canal, thus permitting the anal fissure to heal. No significant continence problems were observed. Although manometric selection of patients leads to different results regarding both postoperative continence and recurrence, these differences are not statistically significant. Therefore, it follows that, in experienced hands and using a standardized technique, manometry before surgical management of anal fissure by lateral sphincterotomy is probably superfluous.
Similar content being viewed by others
References
Notaras J. The treatment of anal fissure by lateral internal sphincterotomy: a technique and results. Br J Surg 1971;58:96–100.
Bennet RC, Duthie HI. The functional importance of the internal anal sphincter. Br J Surg 1964;51:355–7.
Gibbons CP, Read NW. Anal hypertonia in fissures: cause or effect? Br J Surg 1986;73:443–5.
Nicholls J. Fissure in ano and anorectal sepsis. Verh Dtsch Ges Inn Med 1988;9:425–30.
Jensen SL. Treatment of first episodes of acute anal fissure: prospective randomised study of lignocaine ointment versus hydrocortisone ointment or warm sitz baths plus bran. BMJ 1986;292:1167–9.
Jensen SL. Maintenance therapy with unprocessed bran in the prevention of acute anal fissure recurrence. J R Soc Med 1987;80:296–8.
Kortbeek JB, Langevin JM, Khoo RE, Heine JA. Chronic fissure-in-ano: a randomized study comparing open and subcutaneous lateral internal sphincterotomy. Dis Colon Rectum 1992;35:835–7.
Matteucci P, Pittamiglio H, Lopez-Susviela J. Anal cancer masked by benign lesions. Int Surg 1983;68:183–4.
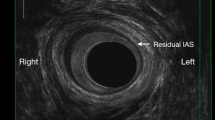
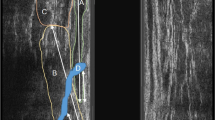
Speakman CT, Burnett SJ, Kamm MA, Bartram CI. Sphincter injury after anal dilatation demonstrated by anal endosonography. Br J Surg 1991;78:1429–30.
Bachmann-Nielsen MB, Rasmussen OO, Pedersen JF, Christiansen J. Risk of sphincter damage and anal incontinence after anal dilatation for fissure-in-ano: an endosonographic study. Dis Colon Rectum 1993;36:677–80.
MacDonald A, Smith A, McNeill AD, Finlay IG. Manual dilatation of the anus. Br J Surg 1992;79:1381–2.
Goldman G, Zilberman M, Werbin N. Bacteremia in anal dilatation. Dis Colon Rectum 1986;29:304–5.
Boulos PB, Araujo JG. Adequate internal sphincterotomy for chronic anal fissure: subcutaneous or open technique? Br J Surg 1984;71:360–2.
Nothmann BJ, Schuster MM. Internal anal sphincter derangement with anal fissures. Gastroenterology 1974;67:216–20.
McNamara MJ, Percy JP, Fielding IR. A manometric study of anal fissure treated by subcutaneous lateral internal sphincterotomy. Ann Surg 1990;211:235–8.
Blessing H. Spaetresultate nach individualisierter lateraler interner sphinkterotomie. Helv Chir Acta 1993;59:603–7.
Olsen J, Mortensen PE, Krogh PI, Christiansen J. Anal sphincter function after treatment of fissure-in-ano by lateral subcutaneous sphincterotomy versus anal dilatation: a randomized study. Int J Colorectal Dis 1987;2:155–7.
Weaver RM, Ambrose NS, Alexander Williams J, Keighley MR. Manual dilatation of the anus vs. lateral subcutaneous sphincterotomy in the treatment of chronic fissure-in-ano: results of a prospective, randomized, clinical trial. Dis Colon Rectum 1987;30:420–3.
Khubchandani IT, Reed JF. Sequelae of internal sphincterotomy for chronic fissure in ano. Br J Surg 1989;76:431–4.
Lewis TH, Corman ML, Prager ED, Robertson WG. Long-term results of open and closed sphincterotomy for anal fissure. Dis Colon Rectum 1988;31:368–71.
Prohm P. Analyse der prä- und postoperativen kontinenz-funktion nach lateraler sphinkterotomie am beispiel der chronischen analfissur. Kontinenz 1992;2:120–4.
Author information
Authors and Affiliations
About this article
Cite this article
Prohm, P., Bönner, C. Is manometry essential for surgery of chronic fissure-in-ano?. Dis Colon Rectum 38, 735–738 (1995). https://doi.org/10.1007/BF02048032
Issue Date:
DOI: https://doi.org/10.1007/BF02048032