Abstract
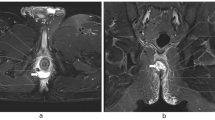
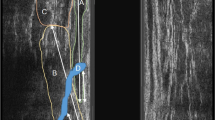
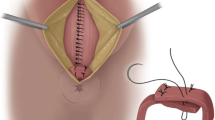
The aim of this study is to describe the technical details and clinical and functional results of anatomical sphincteroplasty as a global reconstructive surgery for the treatment of faecal incontinence caused by anal sphincter lesions. This was a prospective, longitudinal study that included patients who underwent the anatomical sphincteroplasty procedure described here to treat complete sphincter damage. We have described the different technical steps in detail. We evaluated the intraoperative and postoperative complications rate, Cleveland Clinic Score (CCS), a modification of the CCS that included soiling (mCCS), the Faecal Incontinence Quality of Life Scale (FIQLS), and patient satisfaction. An endoanal ultrasound and anorectal manometric study were performed in all the patients. Forty-four patients were included with a mean of 40.5 months follow-up. The CCS reduced from 15 to 3.3 points and the mCCS from 18.5 to 4.5 points over the study period; p < 0.001. Excellent or good results were achieved in 93% of cases. Endoanal ultrasounds showed a good sphincter repair in 66% of the cases. Anorectal manometry showed an increase in the mean maximal resting pressure from 27.6 mmHg to 41.7 mmHg and of the maximal squeeze pressure from 57.9 to 93 mmHg (p < 0.001) with respect to the preoperative values. Anatomical sphincteroplasty is a surgical proposal for the global anatomical reconstruction of anal sphincter lesions, even in cases of very severe damage. The procedure is safe and produced excellent clinical and functional results after a medium-term follow-up.
Graphical abstract






Similar content being viewed by others
Data availability
All data, analytic methods, and study materials used to conduct the research will be made available to any researcher by the corresponding author (J.G.A.), upon reasonable request.
References
Parks AG, McPartlin JF (1971) Late repair of injuries of the anal sphincter. Proc R Soc Med 64:1187–1189
Fang DT, Nivatvongs S, Vermeulen FD et al (1984) Overlapping sphincteroplasty for acquired anal incontinence. Dis Colon Rectum 27:720–722. https://doi.org/10.1007/bf02554596
Cook TA, Mortensen NJ (1998) Management of faecal incontinence following obstetric injury. Br J Surg 85:293–299. https://doi.org/10.1046/j.1365-2168.1998.00693.x
del Rio C, Biondo S, Marti-Rague J (2005) Fecal incontinence. Patient assessment and classical treatments. Cir Esp 78(Suppl 3):34–40. https://doi.org/10.1016/s0009-739x(05)74642-x
Lamblin G, Bouvier P, Damon H et al (2014) Long-term outcome after overlapping anterior anal sphincter repair for fecal incontinence. Int J Colorectal Dis 29:1377–1383. https://doi.org/10.1007/s00384-014-2005-9
Malouf AJ, Norton CS, Engel AF et al (2000) Long-term results of overlapping anterior anal-sphincter repair for obstetric trauma. Lancet (London, England) 355:260–265. https://doi.org/10.1016/S0140-6736(99)05218-6
Wexner SD, Marchetti F, Jagelman DG (1991) The role of sphincteroplasty for fecal incontinence reevaluated: a prospective physiologic and functional review. Dis Colon Rectum 34:22–30. https://doi.org/10.1007/bf02050202
Kreydin EI, Chaudhry ZQ, Kazanjian KK et al (2019) Anal sphincteroplasty in the minimally invasive era: assessment of national trends and complications. Am Surg 85:46–51. https://doi.org/10.1177/000313481908500123
Jordán J, Roig JV, García-Armengol J et al (2010) Risk factors for recurrence and incontinence after anal fistula surgery. Colorectal Dis 12:254–260. https://doi.org/10.1111/j.1463-1318.2009.01806.x
Briel JW, de Boer LM, Hop WC, Schouten WR (1998) Clinical outcome of anterior overlapping external anal sphincter repair with internal anal sphincter imbrication. Dis Colon Rectum 41:209–214. https://doi.org/10.1007/bf02238250
Maslekar S, Gardiner AB, Duthie GS (2007) Anterior anal sphincter repair for fecal incontinence: good longterm results are possible. J Am Coll Surg 204:40–46. https://doi.org/10.1016/j.jamcollsurg.2006.10.008
Berg MR, Gregussen H, Sahlin Y (2019) Long-term outcome of sphincteroplasty with separate suturing of the internal and the external anal sphincter. Tech Coloproctol 23:1163–1172. https://doi.org/10.1007/s10151-019-02122-7
Lestar B, Penninckx F, Kerremans R (1989) The composition of anal basal pressure. An in vivo and in vitro study in man. Int J Colorectal Dis 4:118–122. https://doi.org/10.1007/bf01646870
Wallner Ch, Van Wissen J, Mass CP, Dabhoiwala NF, DeRuiter MC, Lamers WH (2008) The contribution of the levator ani nerve and the pudendal nerve to the innervation of the levator ani muscles; a study in human fetuses. Eur Uro 54:1136–1142. https://doi.org/10.1016/j.eururo.2007.11.015
Londono-Schimmer EE, Garcia-Duperly R, Nicholls RJ et al (1994) Overlapping anal sphincter repair for faecal incontinence due to sphincter trauma: five year follow-up functional results. Int J Colorectal Dis 9:110–113. https://doi.org/10.1007/BF00699424
Oom DMJ, Gosselink MP, Schouten WR (2009) Anterior sphincteroplasty for fecal incontinence: a single center experience in the era of sacral neuromodulation. Dis Colon Rectum 52:1681–1687. https://doi.org/10.1007/DCR.0b013e3181b13862
Pla-Martí V, Moro-Valdezate D, Alos-Company R et al (2007) The effect of surgery on quality of life in patients with faecal incontinence of obstetric origin. Colorectal Dis 9:90–95. https://doi.org/10.1111/j.1463-1318.2006.01128.x
Glasgow SC, Lowry AC (2012) Long-term outcomes of anal sphincter repair for fecal incontinence: a systematic review. Dis Colon Rectum 55:482–490. https://doi.org/10.1097/DCR.0b013e3182468c22
Engel AF, Lunniss PJ, Kamm MA, Phillips RK (1997) Sphincteroplasty for incontinence after surgery for idiopathic fistula in ano. Int J Colorectal Dis 12:323–325. https://doi.org/10.1007/s003840050116
Karoui S, Leroi AM, Koning E et al (2000) Results of sphincteroplasty in 86 patients with anal incontinence. Dis Colon Rectum 43:813–820. https://doi.org/10.1007/bf02238020
Slade MS, Goldberg SM, Schottler JL et al (1977) Sphincteroplasty for acquired anal incontinence. Dis Colon Rectum 20:33–35. https://doi.org/10.1007/bf02587449
Chase S, Mittal R, Jesudason MR et al (2010) Anal sphincter repair for fecal incontinence: experience from a tertiary care centre. Indian J Gastroenterol 29:162–165. https://doi.org/10.1007/s12664-010-0037-9
Felt-Bersma RJ, Cuesta MA, Koorevaar M (1996) Anal sphincter repair improves anorectal function and endosonographic image. A prospective clinical study. Dis Colon Rectum 39:878–885. https://doi.org/10.1007/bf02053986
Ternent CA, Shashidharan M, Blatchford GJ et al (1997) Transanal ultrasound and anorectal physiology findings affecting continence after sphincteroplasty. Dis Colon Rectum 40:462–467. https://doi.org/10.1007/bf02258393
Gearhart S, Hull T, Floruta C et al (2005) Anal manometric parameters: predictors of outcome following anal sphincter repair? J Gastrointest Surg 9:115–120. https://doi.org/10.1016/j.gassur.2004.04.001
Sitzler PJ, Thomson JPS (1996) Overlap repair of damaged anal sphincter. Dis Colon Rectum 39:1356–1360. https://doi.org/10.1007/BF02054524
Oberwalder M, Dinnewitzer A, Baig MK et al (2006) Do internal anal sphincter defects decrease the success rate of anal sphincter repair? Tech Coloproctol. 10:94–97. https://doi.org/10.1007/s10151-006-0259-0. (discussion 97)
Abramov Y, Feiner B, Rosen T et al (2008) Primary repair of advanced obstetric anal sphincter tears: should it be performed by the overlapping sphincteroplasty technique? Int Urogynecol J Pelvic Floor Dysfunct 19:1071–1074. https://doi.org/10.1007/s00192-008-0592-0
Farrell SA, Flowerdew G, Gilmour D et al (2012) Overlapping compared with end-to-end repair of complete third-degree or fourth-degree obstetric tears: three-year follow-up of a randomized controlled trial. Obstet Gynecol 120:803–808. https://doi.org/10.1097/AOG.0b013e31826ac4bb
Gilliland R, Altomare DF, Moreira HJ, Oliveira L, Gilliland JE, Wexner SD (1998) Pudendal neuropathy is predictive of failure following anterior overlapping sphincteroplasty. Dis Colon Rectum 41:1516–1522. https://doi.org/10.1007/bf02237299
Cerdán C, Cerdán DM, Milla L, Ruiz de León A, Cerdán J (2022) Multimodal management of fecal incontinence focused on sphincteroplasty: long-term outcomes from a single center case series. J Clin Med 11:3755. https://doi.org/10.3390/jcm11133755
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Research involving human and ethical approval
The study protocol was approved by the local ethics committee (Consorcio hospital general universitario valencia).
Informed consent
Written informed consent was obtained from all individual participants in the study, including for ongoing use of medical records in future related research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
García-Armengol, J., Martínez-Pérez, C., Roig-Vila, J.V. et al. Anatomical sphincteroplasty as a surgical treatment for faecal incontinence: proposal for a global anatomical reconstructive surgical procedure and results from a case series. Updates Surg (2024). https://doi.org/10.1007/s13304-023-01749-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-023-01749-4