Summary
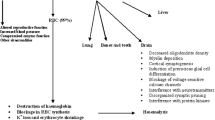
In a group of ten male adults admitted to hospital with clinical symptoms of lead exposure, phenazone elimination rates, blood δ-amino-laevulinic acid dehydratase (ALA.D) activity, blood lead levels and haemoglobin were measured. Investigations were carried out before, immediately after and again at least 12 weeks after cessation of CaEDTA (sodium calcium edetate) chelation therapy. Following chelation, phenazone elimination rates were increased as assessed by a decrease in half life and increase in clearance. This was significant, both immediately after and 12 weeks after cessation of chelation therapy. The change in rate of phenazone metabolism was associated with improved clinical status, with lowered blood lead levels and raised haemoglobin and ALA.D activity. The results of the study suggest that the depression in phenazone elimination in lead intoxication is possibly due to depressed hepatic cytochrome P450 levels.
Similar content being viewed by others
References
Goldberg, A.: Lead poisoning and haem biosynthesis. Brit. J. Haematol.23, 521–524 (1972)
Campbell, B.C., Meredith, P.A., Moore, M.R., Brodie, M.J., Thompson, G.G., Goldberg, A.: Haem biosynthesis and hydroxylation of phenazone during lead intoxication. Biochem. Soc. Trans.4, 1090–1091 (1976)
Scoppa, P., Roumengous, M., Penning, W.: Hepatic drug metabolising activity in lead-poisoned rats. Experientia (Basel),29, 970–972 (1973)
Alvares, A.P., Leigh, S., Cohn, J., Kappas, A.: Lead and methyl mercury: Effects of acute exposure on cytochrome P-450 and the mixed function oxidase system in the liver. J. Exp. Medicine135, 1406–1409 (1972)
Alvares, A.P., Kapelner, S., Sassa, S., Kappas, A.: Drug metabolism in normal children, lead-poisoned children and normal adults. Clin. Pharmacol. Ther.17, 179–183 (1973)
Alvares, A.P., Fishbein, A., Sassa, S., Anderson, K.E., Kappas, A.: Lead intoxication: Effects on cytochrome P-450 mediated hepatic oxidations. Clin. Pharmacol. Ther.19, 183–190 (1976)
Andreassen, P.B., Vessel, E.S.: Comparison of plasma levels of antipyrine, tolbutamide and warfarin after oral and intravenous administration. Clin. Pharmacol. Ther.16, 1059–1065 (1974)
Brodie, B.B., Axelrod, J.: The fate of antipyrine in man. J. Pharmacol. Exp. Ther.98, 97–104 (1950)
Welch, R.M., de Angelis, R.L., Wingfield, M., Farmer, T.W.: Elimination of antipyrine from saliva as a measure of metabolism in man. Clin. Pharmacol. Ther.18, 249–258 (1975)
Vessel, E.S., Passanti, G.T., Glenwright, P.A., Dvorchik, B.M.: Studies on the disposition of antipyrine, aminopyrine and phenacetin using plasma, saliva and urine. Clin. Pharmacol. Ther.18, 259–272 (1975)
Berlin, A., Schaller, K.: European standardised method for the determination of δ-aminolaevulinic acid dehydratase activities in blood. Z. Klin. Chem. Klin. Biochem.12, 389–390 (1974)
Brodie, B.B., Axelrod, J., Soberman, R., Levy, B.B.: The estimation of antipyrine in biological materials. J. biol. Chem.179, 25–29 (1949)
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Meredith, P.A., Campbell, B.C., Moore, M.R. et al. The effects of industrial lead poisoning on cytochrome P450 mediated phenazone (antipyrine) hydroxylation. Eur J Clin Pharmacol 12, 235–239 (1977). https://doi.org/10.1007/BF00609867
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00609867