Summary
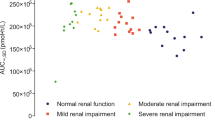
The disposition of clofibrate over 96 hours was observed following single oral dose in six patients with acute viral hepatitis, six patients with liver cirrhosis, seven patients with renal insufficiency, and six control subjects. No parameter of the disposition of CPIB (active form of clofibrate) was significantly altered in acute hepatitis. In liver cirrhosis, the mean plasma half-life was unchanged compared to controls (20.9 vs. 17.5 h), but plasma clearance of the non-protein bound drug was reduced (115 vs. 243 ml×min−1), plasma protein binding was reduced (92.8 vs. 97.2 percent), and the apparent volume of distribution was increased (0.20 vs. 0.141×kg−1). In renal insufficiency plasma half-life was prolonged 2 to 6-fold, depending on the degree of renal impairment. Total plasma clearance (3.4 vs. 7.1 ml×min−1) and plasma clearance of the unbound drug (81 vs. 243 ml×min−1 were reduced in patients with renal failure, the clearance of the unbound drug being inversely correlated with the serum creatinine concentration. Renal failure was also associated with decreased protein binding and an increased volume of distribution of CPIB, and with reduced urinary excretion of CPIB and its glucuronide metabolite. The dose of clofibrate should be halved in patients with cirrhosis. In renal insufficiency, the dose should be adjusted according to the individual serum creatinine level: only 10 to 15% of the usual weekly dose should be given in complete renal failure.
Similar content being viewed by others
References
Bierman, E.L., Brunzell, J.D., Bagdade, J.D., Lerner, R.L., Hazard, W.R., Porte, D. Jr.: On the mechanism of action of Atromid-S on triglyceride transport in man. Trans. Assoc. Am. Physicians83, 211–224 (1970)
Mitchell, W.D., Murchison, L.E.: The effect of clofibrate on serum and fecal lipids. Clin. Chim. Acta36, 153–161 (1972)
Nestel, P.J., Hirsch, Z., Couzens, E.: The effects of chlorophenoxyisobutyric acid and ethinyl estradiol on cholesterol turnover. J. Clin. Invest.44, 891–896 (1965)
Grundy, S.M., Ahrens, E.H., Jr., Salen, G., Schreibman, P.H., Nestel, P.J.: Mechanism of action of clofibrate on cholesterol metabolism in patients with hyperlipidemia. J. Lipid. Res.13, 531–551 (1972)
Clofibrate for the prevention of myocardial infarction. Med. Lett.15, 37–38 (1973
Hunninghake, D.B., Tucker, D.R., Azarnoff, D.L.: Long-term effects of clofibrate (Atromid S) on serum lipids in man. Circulation39, 675–683 (1969)
Dewar, H.A.: Trial of clofibrate in the treatment of ischemic heart disease. Br. med. J.1971/IV, 767–775
Smith, A.F., Macfie, W.G., Oliver, M.F.: Clofibrate, serum levels, and muscle pain. Br. med. J.1970/II 86–88
Sekowski, I., Samuel, P.: Clofibrate induced muscle syndrome. Am. J. Cardiol.30, 572–574 (1972)
Langer, T., Levy, R.I.: Acute muscular syndrome associated with administration of clofibrate. N. Engl. J. Med.279, 851–858 (1968)
Hampers, C.L., Schupak, E., Lowrie, E.G. et al.: Long-term hemodialysis. Second edition, p. 181. New York: Grune and Stratton 1973
Editorial: is control of hyperlipidemia important in renal dialysis? Med. J. Aust.2, 113–118 (1974)
Bagdade, J.D., Porte, D., Jr., Curtis, F.K., Bierman, E.L.: Uremic lipemia: an unrecognized abnormality in triglyceride synthesis and removal. Trans. Assoc. Amer. Physicians81, 190–202 (1968)
Friedman, S.A., Rosen, H.: Uremia and cardiovascular disease. Ann. int. Med.81, 696–697 (1974)
Bagdade, J.D.: Hyperlipidemia, clinical aspects and uremia. S.G. Massry, A.L. Sellers (eds.), pp. 230–240. Springfield: C.C. Thomas 1976
Bridgman, H.F., Rosen, S.M., Thorp, J.M.: Complications during clofibrate treatment of nephrotic syndrome hyperlipoproteinemia. Lancet1972/II 506–509
Perides, A.M., Alvarez-Ude, F., Kerr, D.N.S., Skillen, A. W.: Clofibrate induced muscular damage in patients with chronic renal failure. Lancet1975/II 1279–1282
Kijima, Y., Sasaoka, T., Kanayama, M., Kubota, S.: Untoward effects of clofibrate in hemodialyzed patients. N. Engl. J. Med.296, 515 (1977)
Kurokawa, K.: Clofibrate in hemodialyzed patients. N. Engl. J. Med.296, 942 (1977)
Goldberg, A.P., Sherrard, D.J., Haas, L.B., Brunzell, J.D.: Control of clofibrate toxicity in uremic hypertriglyceridemia. Clin. Pharmacol. Ther.21, 317–325 (1977)
Gugler, R., Shoeman, D.W., Hoffman, D.H., Cohlmia, J.B., Azarnoff, D.L.: Pharmacokinetics of drugs in patients with the nephrotic syndrome. J. Clin. Invest.55, 1182–1189 (1975)
Gugler, R., Jensen, C.: A rapid gas chromatographic method for the determination of chlorophenoxyisobutyric acid in plasma and urine. J. Chromatog.117, 175–179 (1976)
Westlake, W.J.: Time integral of drug concentration in the central (plasma) compartment. J. Pharm. Sci.59, 722–723 (1970)
Sedaghat, A., Ahrens, E.H., Jr.: Lack of effect of cholestyramine on the pharmacokinetics of clofibrate in man. Eur. J. clin. Invest.44, 177–185 (1975)
Thorp, J.M.: Experimental evaluation of an orally active combination of androsterol with ethyl chlorophenoxy isobutyrate. Lancet1962/I 1323–1326
Gugler, R., Hartlapp, J.: Kinetics of clofibrate following single and multiple dosing. Clin. Pharmacol. Ther. (submitted)
Levy, G., Yacobi, A.: Effect of plasma protein binding on elimination of warfarin. J. Pharm. Sci.63, 805–806 (1974)
Shull, H.J., Wilkinson, G.R., Johnson, R., Schenker, S.: Normal elimination of oxacepam in acute viral hepatitis and cirrhosis. Ann. int. Med.84, 420–425 (1976)
Spector, A.A., Santos, E.C., Ashbrook, J.D., Fletcher, J.E.: Influence of free fatty acid concentration on drug binding to plasma albumin. Ann. N. Y. Acad. Sci.226, 247–258 (1973)
Gibson, T.P., Briggs, W.A., Boone, B.J.: Delivery of di-2-ethylhexyl phthalate to patients during hemodialysis. J. Lab. clin. Med.87, 519–524 (1976)
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gugler, R., Kürten, J.W., Jensen, C.J. et al. Clofibrate disposition in renal failure and acute and chronic liver disease. Eur J Clin Pharmacol 15, 341–347 (1979). https://doi.org/10.1007/BF00558438
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00558438