Abstract
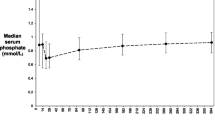
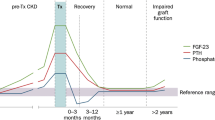
In 1981 cyclosporin A (CyA) became available and replaced azathioprine (Aza) as the immunosuppressive agent in kidney transplantation at the University Hospitals in Basel, Switzerland. Patients on CyA and prednisone (CyA/p) therapy frequently demonstrated an isolated rise in bone-derived serum alkaline phosphatase (aP) concentration, but patients on Aza and prednisone (Aza/p) therapy did not. On the basis of long-term aP concentration and using noninvasive means, the present retrospective study was designed to investigate biochemical markers and radiographic signs of bone disease after successful kidney transplantation in patients on Cya/p treatment. Similar investigations were performed in patients on Aza/p and the results were compared. Follow-up examinations included clinical examination, radiography of the hand, and biochemical analysis of serum and urine. In 139 renal transplant patients on CyA/p, aP increased transiently after successful grafting (at transplantation 84±43 U/l; on day 90, 112±82 U/l). In 50 patients aP levels were higher at the time of transplantation (120±80 U/l) and aP peaked after 8±6 months, at a mean concentration of 242±103 U/l. In these patients aP concentrations exceeded the normal range for 16±10 months. None of the patients on CyA/p showed symptoms of bone disease when aP was increased. Radiological surveys revealed more pronouced osteodystrophy in patients at the time of transplantation, which increased aP to above the normal range after transplantation. Despite this rise in aP, over the long term bone lesions improved radiographically while bone mass remained stable. In constrast, patients treated with Aza/p demonstrated a significant decrease in aP level after transplantation from 75±33 U/l to 54±29 U/l on day 90. In addition, radiographic bone changes persisted and bone mass decreased significantly. After a 2-year follow-up, serum parathyroid hormone, 1,25-(OH)2-vitamin D3, calcium, and phosphorus concentrations, urinary excretion of hydroxyproline, and tubular reabsorption of phosphate did not differ between patients on CyA/p and controls on Aza/p. We conclude that after successful kidney transplantation and initiation of CyA/p therapy, a transient increase in bone-derived aP frequently occurred. These patients more often demonstrated radiographic signs of pre-existing osteodystrophy. However, over the long term, these changes improved.
Similar content being viewed by others
References
Alfrey AC, Jenkins D, Groth CG, Schorr WS, Gecelter L, Ogden DA (1968) Resolution of hyperparathyoidism, renal osteodystrophy and metastatic calcification after renal homotransplantation. N Engl J Med 279: 1349
Behr W, Barnert J, Kanitz W, Vogt H (1986) Quantitative Bestimmung der alkalischen Knochenphosphatase durch Ausfällung mit Weizenkeimlektin. Aerztl Lab 32: 159
Binswanger U, Sherrard DJ, Rich C, Curtis FK (1973) Dialysis bone disease: a quantitative histologic study. Nephron 12: 1
Born W, Dambacher MA, Meyrier A, Ardaillou R, Fischer JA (1982) Parathyroid suppressibility in hyperparathyroidism due to chronic renal failure: studies with autotransplanted parathyroid tissue. Clin Endocrinol 17: 333
Bourbigot B, Moal MC, Cledes J (1988) Bone histology in renal transplant patients receiving cyclosporin (letter). Lancet I: 1049
Calne RY (1987) Cyclosporine in cadaveric renal transplantation: 5-year follow-up of a multicentre trial. Lancet II: 506
Cundy T, Kanis JA (1987) Rapid suppression of plasma alkaline phosphatase activity after renal transplantation in patients with osteodystrophy. Clin Chim Acta 164: 285–291
Delmez JA, Fallon MD, Bergfeld MA, Gearing BK, Dougan CS, Teitelbaum SL (1986) Continuous ambulatory peritoneal dialysis and bone. Kidney Int 30: 379
European Multicentre Trial Group (1983) Cyclosporin in cadaveric renal transplantation: one-year follow-up of a multicentre trial. Lancet II: 986
Haef JG, Joffe P, Podenphant J, Andersen JR (1987) Noninvasive diagnosis of uremic osteodystrophy: uses and limitations. Am J Nephrol 7: 203
Huffer WE, Kuzela D, Popoutzer MM, Starzl TE (1975) Metabolic bone disease in chronic renal failure. II. Renal transplant patients. Am J Pathol 78: 203
Jaeger P, Burckhardt P, Wauters JP, Trachsel U, Bonjour JP (1985) Evidence for a particularly severe secondary hyperparathyroidism in analgesic abuse nephropathy. Am J Nephrol 5: 342
Johnson RWG for the European Multicentre Trial Group (1986) Cyclosporine in cadaveric renal transplantation: three-year follow-up of a European multicentre trial. Transplant Proc 18: 1229
Julian BA, Lawskow DA, Dubovsky J, Dubovsky EV, Curtis JJ, Quarles LD (1991) Rapid loss of vertebral mineral density after renal transplantation. N Engl J Med 325: 544
Lörtscher R, Thiel G, Harder F, Brunner F (1983) Persistent elevation of alkaline phosphatase in cyclosporine-treated renal transplant recipients. Transplantation 36: 115
Malluche HH, Faugere MC (1990) Renal bone disease 1990: an unmet challenge for the nephrologist. Kidney Int 38: 193
Mora Palma FJ, Ellis HA, Cook DB, Dewar JH, Ward MK, Wilkinson R, Kerr DNS (1983) Osteomalacia in patients with chronic renal failure before dialysis or transplantation. Q J Med New Series 207: 332
Movsowitz C, Epstein S, Fallon M, Ismail F, Thomas S (1988) Cyclosporine A in vivo produces severe osteopenia in the rat: effect of dose and duration of administration. Endocrinology 123: 2571
Posen S, Cornish C, Kleerckoper M (1974) Alkaline phosphatase and metabolic bone diseases. In: Avioli LV, Krane SM (eds) Metabolic bone disease. Academic Press, New York
Ritz E, Malluche HH, Bommer J, Mehls O, Krempien B (1974) Metabolic bone disease in patients on maintenance hemodialysis. Nephron 12: 393
Scharla S, Schmidt-Gayk H, Reichel H, Mayer E (1984) A sensitive and simplified radioimmunoassay for 1,25-dihydroxy vitamin D3. Clin Chim Acta 142: 325
Siede WH, Seiffert UB, Bundschuh F, Malluche HH, Schoeppe W (1980) Alkaline phosphatase bone isoenzyme activity in serum in various degrees of micromorphometrically assessed renal osteopathy. Clin Nephrol 13: 277
Stewart PJ, Stern PH (1989) Interaction of cyclosporin A and calcitonin on bone resorption in vitro. Horm Metab Res 21: 194
Stewart PJ, Green OC, Stern PH (1986) Cyclosporine A inhibits calcemic hormone-induced bone resorption in vitro. J Bone Miner Res 1: 285–291
Torres A, Lorenzo V, Gonzales Posada JM (1986) Comparison of histomorphometry and computerized tomography of the spine in quantitating trabecular bone in renal osteodystrophy. Nephron 44: 282
Warren SB, Pelker RR, Friedlaender G (1985) Effects of shortterm cyclosporin A on biomechanical properties of intact and fractured bone in rat. J Orthop Res 3: 96
Author information
Authors and Affiliations
About this article
Cite this article
Briner, V.A., Landmann, J., Brunner, F.P. et al. Cyclosporin A-induced transient rise in plasma alkaline phosphatase in kidney transplant patients. Transplant Int 6, 99–107 (1993). https://doi.org/10.1007/BF00336653
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00336653