Abstract
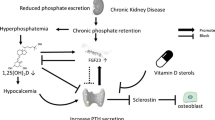
Complications of chronic kidney disease-associated mineral and bone disorders (CKD-MBD) are frequently observed in pediatric kidney transplant recipients and are associated with high morbidity, including growth failure, leg deformities, bone pain, fractures, osteonecrosis, and vascular calcification. Post-transplant CKD-MBD is mainly due to preexisting renal osteodystrophy and cardiovascular changes at the time of transplantation, glucocorticoid treatment, and reduced graft function. In addition, persistent elevated levels of parathyroid hormone (PTH) and fibroblast growth factor 23 may cause hypophosphatemia, resulting in impaired bone mineralization. Patient monitoring should include assessment of growth, leg deformities, and serum levels of calcium, phosphate, magnesium, alkaline phosphatase, 25-hydroxyvitamin D, and PTH. Therapy should primarily focus on regular physical activity, preservation of transplant function, and steroid-sparing immunosuppressive protocols. In addition, adequate monitoring and treatment of vitamin D and mineral metabolism including vitamin D supplementation, oral phosphate, and/or magnesium supplementation, in case of persistent hypophosphatemia/hypomagnesemia, and treatment with active vitamin D in cases of persistent secondary hyperparathyroidism. The latter should be done using the minimum PTH-suppressive dosages aiming at the recommended CKD stage-dependent PTH target range. Finally, treatment with recombinant human growth hormone should be considered in patients lacking catch-up growth within the first year after transplantation.

Similar content being viewed by others
References
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group (2017) KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 7:1–59
Wesseling-Perry K, Bacchetta J (2011) CKD-MBD after kidney transplantation. Pediatr Nephrol 26:2143–2151
Sgambat K, Moudgil A (2014) Optimization of bone health in children before and after renal transplantation: current perspectives and future directions. Front Pediatr 2:13
Haffner D, Schuler U (2014) Metabolic bone disease after renal transplantation. Curr Opin Pediatr 26:198–206
Hohenfellner K, Rauch F, Ariceta G, Awan A, Bacchetta J, Bergmann C, Bechtold S, Cassidy N, Deschenes G, Elenberg E, Gahl WA, Greil O, Harms E, Herzig N, Hoppe B, Koeppl C, Lewis MA, Levtchenko E, Nesterova G, Santos F, Schlingmann KP, Servais A, Soliman NA, Steidle G, Sweeney C, Treikauskas U, Topaloglu R, Tsygin A, Veys K, Vigier VR, Zustin J, Haffner D (2019) Management of bone disease in cystinosis: statement from an international conference. J Inherit Metab Dis 42:1019–1029
Hu MC, Shiizaki K, Kuro-o M, Moe OW (2013) Fibroblast growth factor 23 and klotho: physiology and pathophysiology of an endocrine network of mineral metabolism. Annu Rev Physiol 75:503–533
Portale AA, Wolf M, Juppner H, Messinger S, Kumar J, Wesseling-Perry K, Schwartz GJ, Furth SL, Warady BA, Salusky IB (2014) Disordered FGF23 and mineral metabolism in children with CKD. Clin J Am Soc Nephrol 9:344–353
Hruska KA, Seifert M, Sugatani T (2015) Pathophysiology of the chronic kidney disease-mineral bone disorder. Curr Opin Nephrol Hypertens 24:303–309
Bakkaloglu SA, Borzych D, Soo Ha I, Serdaroglu E, Buscher R, Salas P, Patel H, Drozdz D, Vondrak K, Watanabe A, Villagra J, Yavascan O, Valenzuela M, Gipson D, Ng KH, Warady BA, Schaefer F, International Pediatric Peritoneal Dialysis Network (2011) Cardiac geometry in children receiving chronic peritoneal dialysis: findings from the international pediatric peritoneal dialysis network (IPPN) registry. Clin J Am Soc Nephrol 6:1926–1933
Borzych D, Rees L, Ha IS, Chua A, Valles PG, Lipka M, Zambrano P, Ahlenstiel T, Bakkaloglu SA, Spizzirri AP, Lopez L, Ozaltin F, Printza N, Hari P, Klaus G, Bak M, Vogel A, Ariceta G, Yap HK, Warady BA, Schaefer F, International Pediatric PD Network (IPPN) (2010) The bone and mineral disorder of children undergoing chronic peritoneal dialysis. Kidney Int 78:1295–1304
Salusky IB, Ramirez JA, Oppenheim W, Gales B, Segre GV, Goodman WG (1994) Biochemical markers of renal osteodystrophy in pediatric patients undergoing CAPD/CCPD. Kidney Int 45:253–258
Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, Wang Y, Chung J, Emerick A, Greaser L, Elashoff RM, Salusky IB (2000) Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med 342:1478–1483
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105
Kalantar-Zadeh K, Kuwae N, Regidor DL, Kovesdy CP, Kilpatrick RD, Shinaberger CS, McAllister CJ, Budoff MJ, Salusky IB, Kopple JD (2006) Survival predictability of time-varying indicators of bone disease in maintenance hemodialysis patients. Kidney Int 70:771–780
Denburg MR, Kumar J, Jemielita T, Brooks ER, Skversky A, Portale AA, Salusky IB, Warady BA, Furth SL, Leonard MB (2016) Fracture burden and risk factors in childhood CKD: results from the CKiD cohort study. J Am Soc Nephrol 27:543–550
Querfeld U, Schaefer F (2018) Cardiovascular risk factors in children on dialysis: an update. Pediatr Nephrol. https://doi.org/10.1007/s00467-018-4125-x
Bakkaloglu SA, Wesseling-Perry K, Pereira RC, Gales B, Wang HJ, Elashoff RM, Salusky IB (2010) Value of the new bone classification system in pediatric renal osteodystrophy. Clin J Am Soc Nephrol 5:1860–1866
Baia LC, Heilberg IP, Navis G, de Borst MH, NIGRAM investigators (2015) Phosphate and FGF-23 homeostasis after kidney transplantation. Nat Rev Nephrol 11:656–666
Wesseling-Perry K, Pereira RC, Tsai E, Ettenger R, Juppner H, Salusky IB (2013) FGF23 and mineral metabolism in the early post-renal transplantation period. Pediatr Nephrol 28:2207–2215
Monier-Faugere MC, Mawad H, Qi Q, Friedler RM, Malluche HH (2000) High prevalence of low bone turnover and occurrence of osteomalacia after kidney transplantation. J Am Soc Nephrol 11:1093–1099
Weisinger JR, Carlini RG, Rojas E, Bellorin-Font E (2006) Bone disease after renal transplantation. Clin J Am Soc Nephrol 1:1300–1313
Shroff R, Knott C, Gullett A, Wells D, Marks SD, Rees L (2011) Vitamin D deficiency is associated with short stature and may influence blood pressure control in paediatric renal transplant recipients. Pediatr Nephrol 26:2227–2233
Uslu Gokceoglu A, Comak E, Dogan CS, Koyun M, Akbas H, Akman S (2014) Magnesium excretion and hypomagnesemia in pediatric renal transplant recipients. Ren Fail 36:1056–1059
Mazzola BL, Vannini SD, Truttmann AC, von Vigier RO, Wermuth B, Ferrari P, Bianchetti MG (2003) Long-term calcineurin inhibition and magnesium balance after renal transplantation. Transpl Int 16:76–81
Castiglioni S, Cazzaniga A, Albisetti W, Maier JA (2013) Magnesium and osteoporosis: current state of knowledge and future research directions. Nutrients 5:3022–3033
Van de Cauter J, Sennesael J, Haentjens P (2011) Long-term evolution of the mineral metabolism after renal transplantation: a prospective, single-center cohort study. Transplant Proc 43:3470–3475
Ozturk CF, Karakelleoglu C, Orbak Z, Yildiz L (2012) The effect of serum magnesium levels and serum endothelin-1 levels on bone mineral density in protein energy malnutrition. West Indian Med J 61:213–218
Hayes W, Boyle S, Carroll A, Bockenhauer D, Marks SD (2017) Hypomagnesemia and increased risk of new-onset diabetes mellitus after transplantation in pediatric renal transplant recipients. Pediatr Nephrol 32:879–884
Carpenter TO, DeLucia MC, Zhang JH, Bejnerowicz G, Tartamella L, Dziura J, Petersen KF, Befroy D, Cohen D (2006) A randomized controlled study of effects of dietary magnesium oxide supplementation on bone mineral content in healthy girls. J Clin Endocrinol Metab 91:4866–4872
Franke D, Thomas L, Steffens R, Pavicic L, Gellermann J, Froede K, Querfeld U, Haffner D, Zivicnjak M (2015) Patterns of growth after kidney transplantation among children with ESRD. Clin J Am Soc Nephrol 10:127–134
Bailey JL, Wang X, England BK, Price SR, Ding X, Mitch WE (1996) The acidosis of chronic renal failure activates muscle proteolysis in rats by augmenting transcription of genes encoding proteins of the ATP-dependent ubiquitin-proteasome pathway. J Clin Invest 97:1447–1453
Boirie Y, Broyer M, Gagnadoux MF, Niaudet P, Bresson JL (2000) Alterations of protein metabolism by metabolic acidosis in children with chronic renal failure. Kidney Int 58:236–241
Brungger M, Hulter HN, Krapf R (1997) Effect of chronic metabolic acidosis on the growth hormone/IGF-1 endocrine axis: new cause of growth hormone insensitivity in humans. Kidney Int 51:216–221
Challa A, Chan W, Krieg RJ, Thabet MA, Liu F, Hintz RL, Chan JC (1993) Effect of metabolic acidosis on the expression of insulin-like growth factor and growth hormone receptor. Kidney Int 44:1224–1227
Challa A, Krieg RJ, Thabet MA, Veldhuis JD, Chan JC (1993) Metabolic acidosis inhibits growth hormone secretion in rats: mechanism of growth retardation. Am J Physiol 265:E547–E553
Suzuki Y, Ichikawa Y, Saito E, Homma M (1983) Importance of increased urinary calcium excretion in the development of secondary hyperparathyroidism of patients under glucocorticoid therapy. Metabolism 32:151–156
O'Brien CA, Jia D, Plotkin LI, Bellido T, Powers CC, Stewart SA, Manolagas SC, Weinstein RS (2004) Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strength. Endocrinology 145:1835–1841
Brandenburg VM, Ketteler M, Heussen N, Politt D, Frank RD, Westenfeld R, Ittel TH, Floege J (2005) Lumbar bone mineral density in very long-term renal transplant recipients: impact of circulating sex hormones. Osteoporos Int 16:1611–1620
Klaus G, Jux C, Leiber K, Hugel U, Mehls O (1996) Interaction between insulin-like growth factor I, growth hormone, parathyroid hormone, 1 alpha,25-dihydroxyvitamin D3 and steroids on epiphyseal chondrocytes. Acta Paediatr Suppl 417:69–71
Delucchi A, Toro L, Alzamora R, Barrientos V, Gonzalez M, Andaur R, Leon P, Villanueva F, Galindo M, Heras FL, Montecino M, Moena D, Lazcano A, Pinto V, Salas P, Reyes ML, Mericq V, Michea L (2019) Glucocorticoids decrease longitudinal bone growth in paediatric kidney transplant recipients by stimulating the FGF23/FGFR3 signalling pathway. J Bone Miner Res. https://doi.org/10.1002/jbmr.3761
Terpstra AM, Kalkwarf HJ, Shults J, Zemel BS, Wetzsteon RJ, Foster BJ, Strife CF, Foerster DL, Leonard MB (2012) Bone density and cortical structure after pediatric renal transplantation. J Am Soc Nephrol 23:715–726
Epstein S (1996) Post-transplantation bone disease: the role of immunosuppressive agents and the skeleton. J Bone Miner Res 11:1–7
Alvarez-Garcia O, Carbajo-Perez E, Garcia E, Gil H, Molinos I, Rodriguez J, Ordonez FA, Santos F (2007) Rapamycin retards growth and causes marked alterations in the growth plate of young rats. Pediatr Nephrol 22:954–961
Singha UK, Jiang Y, Yu S, Luo M, Lu Y, Zhang J, Xiao G (2008) Rapamycin inhibits osteoblast proliferation and differentiation in MC3T3-E1 cells and primary mouse bone marrow stromal cells. J Cell Biochem 103:434–446
Billing H, Burmeister G, Plotnicki L, Ahlenstiel T, Fichtner A, Sander A, Hocker B, Tonshoff B, Pape L (2013) Longitudinal growth on an everolimus- versus an MMF-based steroid-free immunosuppressive regimen in paediatric renal transplant recipients. Transpl Int 26:903–909
Forster J, Ahlenstiel-Grunow T, Zapf A, Mynarek M, Pape L (2016) Pubertal development in pediatric kidney transplant patients receiving mammalian target of rapamycin inhibitors or conventional immunosuppression. Transplantation 100:2461–2470
Bartosh SM, Leverson G, Robillard D, Sollinger HW (2003) Long-term outcomes in pediatric renal transplant recipients who survive into adulthood. Transplantation 76:1195–1200
Groothoff JW, Cransberg K, Offringa M, van de Kar NJ, Lilien MR, Davin JC, Heymans HS, Dutch cohort study (2004) Long-term follow-up of renal transplantation in children: a dutch cohort study. Transplantation 78:453–460
Helenius I, Remes V, Salminen S, Valta H, Makitie O, Holmberg C, Palmu P, Tervahartiala P, Sarna S, Helenius M, Peltonen J, Jalanko H (2006) Incidence and predictors of fractures in children after solid organ transplantation: a 5-year prospective, population-based study. J Bone Miner Res 21:380–387
Helenius I, Remes V, Tervahartiala P, Salminen S, Sairanen H, Holmberg C, Palmu P, Helenius M, Peltonen J, Jalanko H (2006) Spine after solid organ transplantation in childhood: a clinical, radiographic, and magnetic resonance imaging analysis of 40 patients. Spine (Phila Pa 1976) 31:2130–2136
Lehmann G, Ott U, Stein G, Steiner T, Wolf G (2007) Renal osteodystrophy after successful renal transplantation: a histomorphometric analysis in 57 patients. Transplant Proc 39:3153–3158
Rojas E, Carlini RG, Clesca P, Arminio A, Suniaga O, De Elguezabal K, Weisinger JR, Hruska KA, Bellorin-Font E (2003) The pathogenesis of osteodystrophy after renal transplantation as detected by early alterations in bone remodeling. Kidney Int 63:1915–1923
Cruz EA, Lugon JR, Jorgetti V, Draibe SA, Carvalho AB (2004) Histologic evolution of bone disease 6 months after successful kidney transplantation. Am J Kidney Dis 44:747–756
Borchhardt K, Sulzbacher I, Benesch T, Fodinger M, Sunder-Plassmann G, Haas M (2007) Low-turnover bone disease in hypercalcemic hyperparathyroidism after kidney transplantation. Am J Transplant 7:2515–2521
Cueto-Manzano AM, Konel S, Crowley V, France MW, Freemont AJ, Adams JE, Mawer B, Gokal R, Hutchison AJ (2003) Bone histopathology and densitometry comparison between cyclosporine a monotherapy and prednisolone plus azathioprine dual immunosuppression in renal transplant patients. Transplantation 75:2053–2058
Keronen S, Martola L, Finne P, Burton IS, Kroger H, Honkanen E (2019) Changes in bone histomorphometry after kidney transplantation. Clin J Am Soc Nephrol 14:894–903
Sanchez CP, Salusky IB, Kuizon BD, Ramirez JA, Gales B, Ettenger RB, Goodman WG (1998) Bone disease in children and adolescents undergoing successful renal transplantation. Kidney Int 53:1358–1364
Leonard MB (2005) Assessment of bone mass following renal transplantation in children. Pediatr Nephrol 20:360–367
Leonard MB (2007) A structural approach to the assessment of fracture risk in children and adolescents with chronic kidney disease. Pediatr Nephrol 22:1815–1824
Reusz GS, Szabo AJ, Peter F, Kenesei E, Sallay P, Latta K, Szabo A, Szabo A, Tulassay T (2000) Bone metabolism and mineral density following renal transplantation. Arch Dis Child 83:146–151
Behnke B, Altrogge H, Delling G, Kruse HP, Muller-Wiefel DE (1996) Bone mineral density in pediatric patients after renal transplantation. Clin Nephrol 46:24–29
Ruth EM, Weber LT, Schoenau E, Wunsch R, Seibel MJ, Feneberg R, Mehls O, Tonshoff B (2004) Analysis of the functional muscle-bone unit of the forearm in pediatric renal transplant recipients. Kidney Int 66:1694–1706
Klare B, Montoya CR, Fischer DC, Stangl MJ, Haffner D (2012) Normal adult height after steroid-withdrawal within 6 months of pediatric kidney transplantation: a 20 years single center experience. Transpl Int 25:276–282
Ruben S, Kreuzer M, Buscher A, Buscher R, Thumfart J, Querfeld U, Staude H, Ahlenstiel-Grunow T, Melk A, Fischer DC, Leifheit-Nestler M, Pape L, Haffner D (2018) Impaired microcirculation in children after kidney transplantation: everolimus versus mycophenolate based immunosuppression regimen. Kidney Blood Press Res 43:793–806
Borchert-Morlins B, Thurn D, Schmidt BMW, Buscher AK, Oh J, Kier T, Bauer E, Baig S, Kanzelmeyer N, Kemper MJ, Buscher R, Melk A (2017) Factors associated with cardiovascular target organ damage in children after renal transplantation. Pediatr Nephrol 32:2143–2154
Schmidt BMW, Sugianto RI, Thurn D, Azukaitis K, Bayazit AK, Canpolat N, Eroglu AG, Caliskan S, Doyon A, Duzova A, Karagoz T, Anarat A, Deveci M, Mir S, Ranchin B, Shroff R, Baskin E, Litwin M, Ozcakar ZB, Buscher R, Soylemezoglu O, Dusek J, Kemper MJ, Matteucci MC, Habbig S, Laube G, Wuhl E, Querfeld U, Sander A, Schaefer F, Melk A, 4C Study Consortium (2018) Early effects of renal replacement therapy on cardiovascular comorbidity in children with end-stage kidney disease: findings from the 4C-T study. Transplantation 102:484–492
Hristova M, van Beek C, Schurgers LJ, Lanske B, Danziger J (2010) Rapidly progressive severe vascular calcification sparing the kidney allograft following warfarin initiation. Am J Kidney Dis 56:1158–1162
Moe SM, O'Neill KD, Reslerova M, Fineberg N, Persohn S, Meyer CA (2004) Natural history of vascular calcification in dialysis and transplant patients. Nephrol Dial Transplant 19:2387–2393
KDOQI Work Group (2009) KDOQI clinical practice guideline for nutrition in children with CKD: 2008 update. executive summary. Am J Kidney Dis 53:S11–S104
Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group (2009) KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant 9(Suppl 3):S1–S155
Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, McCann L, Moe SM, Shroff R, Tonelli MA, Toussaint ND, Vervloet MG, Leonard MB (2017) Executive summary of the 2017 KDIGO chronic kidney disease-mineral and bone disorder (CKD-MBD) guideline update: what’s changed and why it matters. Kidney Int 92:26–36
Ahmed MA, Abd El Samad AA (2013) Benefits of omega-3 fatty acid against bone changes in salt-loaded rats: possible role of kidney. Physiol Rep 1:e00106
Teofilo JM, Leonel DV, Lamano T (2010) Cola beverage consumption delays alveolar bone healing: a histometric study in rats. Braz Oral Res 24:177–181
Shroff R, Wan M, Nagler EV, Bakkaloglu S, Fischer DC, Bishop N, Cozzolino M, Bacchetta J, Edefonti A, Stefanidis CJ, Vande Walle J, Haffner D, Klaus G, Schmitt CP, European Society for Paediatric Nephrology Chronic Kidney Disease Mineral and Bone Disorders and Dialysis Working Groups (2017) Clinical practice recommendations for native vitamin D therapy in children with chronic kidney disease stages 2-5 and on dialysis. Nephrol Dial Transplant 32:1098–1113
Shroff R, Wan M, Nagler EV, Bakkaloglu S, Cozzolino M, Bacchetta J, Edefonti A, Stefanidis CJ, Vande Walle J, Ariceta G, Klaus G, Haffner D, Schmitt CP; European Society for Paediatric Nephrology Chronic Kidney Disease Mineral and Bone Disorders and Dialysis Working Groups (2017) Clinical practice recommendations for treatment with active vitamin D analogues in children with chronic kidney disease stages 2-5 and on dialysis. Nephrol Dial Transplant 32:1114-1127
Rees L (2008) What parathyroid hormone levels should we aim for in children with stage 5 chronic kidney disease; what is the evidence? Pediatr Nephrol 23:179–184
Klaus G, Watson A, Edefonti A, Fischbach M, Ronnholm K, Schaefer F, Simkova E, Stefanidis CJ, Strazdins V, Vande Walle J, Schroder C, Zurowska A, Ekim M, European Pediatric Dialysis Working Group (EPDWG) (2006) Prevention and treatment of renal osteodystrophy in children on chronic renal failure: European guidelines. Pediatr Nephrol 21:151–159
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group (2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 113:S1–S130
Haffner D, Schaefer F (2013) Searching the optimal PTH target range in children undergoing peritoneal dialysis: new insights from international cohort studies. Pediatr Nephrol 28:537–545
Zhang H, Zheng Y, Liu L, Fu Q, Li J, Huang Q, Liu H, Deng R, Wang C (2016) Steroid avoidance or withdrawal regimens in paediatric kidney transplantation: a meta-analysis of randomised controlled trials. PLoS One 11:e0146523
Wu Y, Cheng W, Yang XD, Xiang B (2013) Growth hormone improves growth in pediatric renal transplant recipients--a systemic review and meta-analysis of randomized controlled trials. Pediatr Nephrol 28:129–133
Sanchez CP, Kuizon BD, Goodman WG, Gales B, Ettenger RB, Boechat MI, Wang Y, Elashoff R, Salusky IB (2002) Growth hormone and the skeleton in pediatric renal allograft recipients. Pediatr Nephrol 17:322–328
Drube J, Wan M, Bonthuis M, Wuhl E, Bacchetta J, Santos F, Grenda R, Edefonti A, Harambat J, Shroff R, Tonshoff B, Haffner D, European Society for Paediatric Nephrology Chronic Kidney Disease Mineral and Bone Disorders, Dialysis (2019) Clinical practice recommendations for growth hormone treatment in children with chronic kidney disease. Nat Rev Nephrol 15:577–589
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D.H. has received research grants from Sandoz, Kyowa Kirin, Horizon, and Amgen and has received speaker and/or consultant fees from Amgen, Sandoz, Kyowa Kirn, Pfizer, Merck Serono, Horizon, and Chiesi. M.L.N. received travel grants from Amgen.
Additional information
Answers to multiple choice questions:
1. a; 2. c; 3. a; 4. d; 5. a
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haffner, D., Leifheit-Nestler, M. CKD-MBD post kidney transplantation. Pediatr Nephrol 36, 41–50 (2021). https://doi.org/10.1007/s00467-019-04421-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04421-5