Abstract
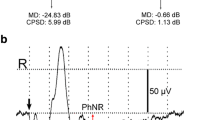
Eighteen patients with acute retrobulbar neuritis were examined by visual field analysis and electroophthalmological recordings. The visual fields were measured to 30° with the automatic perimeter Octopus 201. The pattern-evoked cortical potential showed an increased P-100 latency followed by a decrease in 12 patients during the first two weeks of the disease. This latency change cannot be explained by remyelinization. The positive component of the pattern ERG (P-50) was reduced in all acutely affected eyes in comparison with the fellow eye. During recovery, the amplitude of the positive PERG component increased to normal, but remained slightly reduced in comparison with the response from the fellow eyes. Thirteen patients out of 18 were clinically and electrophysiologically diagnosed as having unilateral retrobulbar neuritis. However, static perimetry showed paracentral scotomas in the fellow eye in 5 cases. Recovery of the severely affected eye was accompanied by complete normalization of the visual field in the fellow eye. Thus static perimetry seems to be a more sensitive test than even the visual evoked potentials for detecting lesions in the visual pathway.
Similar content being viewed by others
References
Glaser JS. Optic neuritides. In: Duane TD, Jaeger EA, eds. Clinical ophthalmology. Philadelphia: Harper & Row, 1986; 2, 5: 43–5.
Percy AK, Nobrega FT, Kurland LT. Optic neuritis and multiple sclerosis: An epidemiologic study. Arch Ophthalmol 1972; 87; 136–9.
Taub RG, Rucker CW. The relation of retrobulbar neuritis to multiple sclerosis. Am J Ophthalmol 1954; 37: 393–9.
Bradley WG, Whitty WM. Acute optic neuritis: Prognosis for development of multiple sclerosis. J Neurol Neurosurg Psychiatry 1968; 31: 10.
Ormerod EC, Miller DH, McDonald WI, du Boulay EPGH, Kendall BE, Moseley IF, Johnson G, Tofts PS, Halliday AM, Bronstein AM, Scaravilli F, Harding AE, Barnes D, Zilkkha KJ. The role of NMR imaging in the assessment of multiple sclerosis and isolated neurological lesions: A quantitative study. Brain 1987; 110: 1579–616.
Halliday AM, McDonald WI, Mushin J. Delayed visual evoked responses in optic neuritis. Lancet 1972; 1: 982–5.
Halliday AM, McDonald WI, Mushin J. Visual evoked response in diagnosis of multiple sclerosis. Br Med J 1973; 4: 661–4.
Meienberg O, Flammer J, Ludin H-P. Subclinical visual defects in multiple sclerosis. J Neurol 1982; 227: 125–13.
van Dalen JTW, Spekreijse H. Comparison of visual field examinations and visual evoked cortical potentials in multiple sclerosis patients. Doc Ophthalmol Proc Series 1981; 27: 139–46.
Fiorentini A, Maffei L, Pirchio M, Spinelli D, Porciatti V. The ERG in response to alternating gratings in patients with disease of the peripheral visual pathways. Invest Ophthalmol Vis Sci 1981; 21: 490–3.
Arden GB, Vaegan, Hogg CR. Clinical and experimental evidence that the pattern electroretinogram (PERG) is generated in more proximal retinal layers than the focal electroretinogram (FERG). Ann NY Acad Sci 1982; 388: 580–601.
Berdjis H, Gedeon B, Staerk N, Jacobi G. Muster-ERG und -VECP nach Optikusneuritis im Kindesalter. Klin Monatsbl Augenheilkd 1984; 184: 533–5.
Plant GT, Hess RF, Thomas SJ. The pattern evoked electroretinogram in optic neuritis. Brain 1986; 109: 469–90.
Sherman J. Simultaneous pattern-reversal electroretinograms and visual evoked potentials in disease of the macula and optic nerve. Ann NY Acad Sci 1982; 388: 214–26.
Celesia GG, Kaufman D: Pattern ERGs and visual evoked potentials in maculopathies and optic nerve diseases. Invest Ophthalmol Vis Sci 1985; 26: 726–35.
McAlpine D. Course and prognosis. In: McAlpine D, Lumsden C, Acheson ED, eds. Multiple sclerosis, a reappraisal. London: Churchill Livingstone, 1972; 197–225.
Arden GB, Carter RM, Hogg CR, Siegel IM, Margolis S. A gold foil electrode: Extending the horizons for clinical electroretinography. Invest Ophthalmol Vis Sci 1979; 18: 421–6.
Hess RF, Baker Jr CL. Human pattern-evoked electroretinogram. J. Neurophysiol 1984; 51: 939–51.
Berninger TA. The pattern electroretinogram and its contamination. Clin Vis Sci 1986; 1: 185–90.
Gloor B, Schmied U, Faessler A. Glaukomgesichtsfelder Analyse von Octopus-Verlaufsbeobachtungen mit einem statistischen Programm. Klin Monatsbl Augenheilkd 1980; 177: 423–35.
Berninger TA, Schuurmans RP. Spatial tuning of the pattern ERG across temporal frequency. DOC Ophthalmol 1985; 61: 17–25.
Holder GE. Significance of abnormal pattern electroretinography in anterior visual pathway dysfunction. Br J Ophthalmol 1987; 71: 161–71.
Drasdo N, Cox W, Thompson DA: The effects of image degradation on retinal illuminance and pattern responses to checkerboard stimuli. Doc Ophthalmol 1987; 66: 267–73.
Harding GFA, Wright CE. Visual evoked potentials in acute optic neuritis. In: Hess RF, Plant GT eds. Optic neuritis. Cambridge: Cambridge University Press 1985; 230–54.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Berninger, T.A., Heider, W. Electrophysiology and perimetry in acute retrobulbar neuritis. Doc Ophthalmol 71, 293–305 (1989). https://doi.org/10.1007/BF00170978
Issue Date:
DOI: https://doi.org/10.1007/BF00170978