Abstract
Adrenocortical carcinoma (ACC) is often diagnosed incidentally. However, significant difficulties persist in diagnosing the rare ACC among the very common benign adrenal tumors, which are present in up to 5 % of the population. Due to the very low prevalence of ACC, prospective studies are impossible to conduct. Two recent studies took the approach of reviewing preexisting adrenal tumors prior to the diagnosis of ACC. These data challenge current concepts of diagnosis and surveillance of incidentally discovered masses. Oncocytomas (benign and malignant) represent an entity that can be difficult to be diagnosed by radiographic characteristics and even histologically. However, some recent data provides insight into their appearance in imaging procedures. With regards to ACC specific imaging, which could be applied for differential diagnosis of adrenal tumors, surgery planning and surveillance several radionucleotides have been evaluated over the last decades showing promising results. Of particular interest, these substances can potentially be used for therapy as well.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Imaging Evaluation of Adrenal Tumors
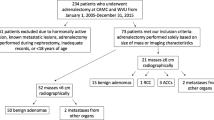
The management of adrenal tumors is a public health challenge of growing importance, as these tumors are detected with increasing frequency in a population that has widespread access to advanced imaging technology. The prevalence of incidentally discovered adrenal masses on CT examinations has been reported to be 0.35–5.0 % [1]. Biochemical testing is necessary to distinguish between functional and non-functional adrenal masses. In hormonally non-functioning tumors, it is a major diagnostic challenge to differentiate between benign and malignant lesions, as the perceived risk of malignancy defines the necessity of surgical intervention. In non-oncological patients, adrenocortical carcinoma (ACC) is thought to be the most frequently observed adrenal malignancy with a prevalence of up to 4–6 % depending on size and appearance [1]. However, this is likely a significant overestimate as more recent unbiased imaging approaches found a prevalence of 0–1 % [2, 3]. Currently, tumor size and a low lipid content of an adrenal mass and the velocity of the washout of contrast medium are probably the best criteria for diagnosing ACC. Benign adrenocortical adenomas usually have a high content of lipids, resulting in a low attenuation coefficient on unenhanced CT (<10 Hounsfield units (HU)). In a retrospective analysis of CT scans from 51 patients with ACC and 25 patients with benign adrenal tumors, the median unenhanced HU value was 34 (range 14–74) in ACCs. A cutoff value of 21 HU revealed a sensitivity of 96 % and specificity 80 %. One hundred percent sensitivity was reached at a threshold of 13.9 with a specificity of 68 % [4]. On delayed contrast-enhanced CT, adenomas typically exhibit rapid washout of contrast medium, whereas non-adenomatous tumors display delayed washout of contrast material [5, 6]. However, despite these highly useful criteria, a significant number of adrenal incidentalomas (around 30 % of tumors >3 cm) are not reliably characterized by these standard imaging procedures and these tumors are largely considered an indication for surgery. However, based on histopathology, the majority of these cases are benign adenomas [7]. Fine-needle biopsy should be avoided in adrenal incidentalomas, as it is often non-informative and potentially hazardous with regards to the diagnosis ACC [8]. Furthermore, several tumors, including carcinomas of the lung, breast, kidney, and melanoma, frequently metastasize into the adrenal glands and adrenal metastasis may be the first indication of a yet unknown malignancy. A recent retrospective analysis assessed imaging characteristics of adrenal tumors preceding the diagnosis of ACC. In this case series, 10 % of tumors demonstrated initial imaging characteristics in CT or MRI that were suggestive of a benign tumor. Twenty-five percent of tumors were small lesions <2 cm, and the growth pattern showed high variability with long-term stability of size over up to 8 years in single cases [9]. Another study provided comparable results, even including some tumors arising in patients that had recent CT scans not showing any adrenal tumor, proving a rapid de novo growth in some patients [10]. One main conclusion from these data is the great variation in time to progression to the clinical diagnosis of ACC. In addition, the current recommendations of following at least some incidentalomas with suspicious features for up to 2 years might only identify 50 % of ACC. Taken the rarity of ACC among adrenal incidentalomas, caution needs to be applied. On a population basis, imaging procedures for the initial differential diagnosis and surveillance might incur more harm (e.g., XRT induced cancers, psychological stress) and costs than benefit in identifying the rare ACCs. Employing these potentially risk-baring procedures for determining the further differential diagnosis of an adrenal tumor should only be conducted in a selected population of patients. While it might certainly be possible to definitively diagnose the underlying pathology of every adrenal mass (e.g., in the theoretical setting of surgery for every patient with an incidentally discovered adrenal mass), clinical practice and future guidelines need to apply a thoughtful integration of risks associated with diagnostic procedures and potential benefit of curing early stage ACCs.
Radiographic Characteristics of Oncocytic Adrenal Lesions
Oncocytic adrenal neoplasms (OANs) are rare tumors whose imaging characteristics have not been well described and generally pose a challenge with regardmn to their biological behavior. Histologically, oncocytic adrenal neoplasms (OANs) demonstrate >75 % oncocytes—epithelial cells with abundant granular eosinophilic cytoplasm. OANs may be benign (oncocytomas) or malignant. Several imaging features often used to distinguish benign from malignant adrenal neoplasms could be applied to oncocytic neoplasms [11]. These include homogeneity, smaller size, and percentage enhancement washout characteristics. Benign OANs were often homogeneous and lacked calcification or hemorrhage. The mean diameter of the oncocytomas was 3.7 cm (range 2.6–5.3) whereas the malignant OANs measured greater than 5 cm in diameter. The benign OANs measured >10 HU on unenhanced CT which is consistent with histologic findings that lipid content is not a distinguishing characteristic of an OAN. However, the oncocytomas demonstrated washout characteristics similar to adenomas showing washouts greater than 60 %. Also of note, benign OANs were not associated with imaging features of aggression such as venous invasion, enlarged regional lymph nodes, or perilesional fat stranding. Malignant OANs and ACCs also had overlapping CT imaging characteristics, including larger size, heterogeneity, and internal necrosis. However, a larger number of cases are needed to confirm these conclusions and to better understand these adrenal tumors.
Imaging Techniques for Initial Diagnosis and Surveillance of ACC
Thus, improved tools for characterizing adrenal masses prior to surgery are of great clinical interest. Functional imaging tools may significantly contribute to the diagnostic evaluation of adrenal masses. In adrenal tumors, 18F-FDG-PET was first evaluated in patients with known extraadrenal malignancies. Qualitative visual evaluation was considered as equally accurate as quantitative evaluation using standardized uptake values (SUV) for identification of adrenal metastases with a high specificity but only relatively low sensitivity. However, Schulkin et al. demonstrated that also pheochromocytomas frequently show an increased fludeoxyglucose (FDG) uptake on PET [12]. Furthermore, malignant adrenal lesions that may produce false-negative PET results have also been reported in patients with adrenal metastases, e.g., secondary to pulmonary carcinoid, renal, and alveolar lung carcinoma. In a series of 105 patients with incidental adrenal masses, adrenocortical carcinomas demonstrated a high FDG uptake, as did the majority of pheochromocytomas. Furthermore, adrenal metastases also demonstrated increased FDG activity [13]. In a prospective trial, 81 patients with adrenal masses (size >3 cm, spontaneous attenuation value >10 HU, heterogeneous aspect, abnormal MIBG or norcholesterol scan or hormonal hypersecretion) undergoing surgery were investigated. Sixty percent would have qualified for surgery according to histological and clinical criteria while 40 % represented benign non-secreting lesions, mostly adrenocortical adenomas. 18F FDG-PET was negative in 97 % of non-surgical lesions and positive in 73 % of potentially surgical ones. Thus, a high FDG uptake was highly predictive of malignancy [14].
In known ACC, 18F-FDG PET imaging results may have a further impact on the management of ACC compared to conventional imaging. In a retrospective analysis of patients with ACC undergoing 18F-FDG-PET/CT, PET/CT changed the management plan in 5 % at initial staging and 9 % at restaging. No PET/CT parameters were associated with survival at either initial diagnosis or recurrence [15].
These findings indicate that FDG-PET has good accuracy to assess the malignant potential of an adrenal lesion without providing robust information on the origin of the adrenal mass.
More recently, metomidate derivatives which bind with high specificity and avidity to CYP11B enzymes of adrenocortical cells have been developed as tracers for adrenal imaging. These tracers have the advantage of a highly specific binding to molecules that are uniquely expressed in adrenocortical cells. The following tracers have been introduced into clinical practice: [11C]metomidate (MTO), [18F]fluoro-etomidate (FETO) for PET imaging, and [123I]iodometomidate for SPECT imaging.
For example, Juhlin et al. found high uptake of MTO in all tumors originating from the adrenal cortex, whereas all other processes were negative [16]. Similarly, Minn et al. found the highest uptake in ACC followed by active adenomas and non-secretory adenomas and very low uptake in non-cortical tumors [17]. In a retrospective evaluation of 212 MTO-PET examinations in 173 patients, Hennings et al. reported that non-adrenocortical lesions were negative in MTO-PET [18]. Zettinig et al. investigated 16 patients with 18F-FDG-PET and [11C]metomidate and demonstrated that metomidate could distinguish adrenocortical from non-adrenocortical tissue, whereas 18F-FDG PET differentiated malignant from benign disease [19]. Similar results have been obtained with [123I]iodometomidate with the clear advantage that this SPECT tracer does not require the local availability of a cyclotron facilitating its widespread use and also demonstrating high specificity [20]. Taken together, these studies indicate that this new imaging modality might confer significant specificity to the characterization of adrenal neoplasia. Combined imaging with 18F FDG-PET and metomidate derivatives may be of great help to non-invasively characterize adrenal lesions and to better distinguish between lesions with an indication for surgical removal from those not requiring surgery.
Advanced ACC has an overall poor prognosis and a strong tendency toward rapid progression. Despite the lack of prospective, controlled trials, mitotane was approved in Europe in 2004. Most data derive from retrospective series, and the objective response rate is at best 24 %. In the only available phase III trial comparing efficacy of the so far best available treatment options of cytotoxic chemotherapy in patients with advanced ACC, median survival was only 12–15 months, indicating the urgent need for improved treatment strategies [21]. The clinical utility of a theranostics concept employing radiolabeled iodometomidate for both diagnoses of adrenal tumors and as targeted treatment of advanced ACC has recently been shown [20, 22, 23]. Studies with [123I]iodometomidate in patients with ACC have demonstrated that a high percentage of patients (>30 %) show high tracer uptake in their metastatic lesions [20]. In a recent series of ten patients with advanced ACC, for the first time, a therapeutic potential of treatment with [131I]iodometomidate could be demonstrated. [131I]Iodometomidate induced a partial response or a lasting stabilization of disease in the majority of patients while treatment was very well tolerated [23]. However, studies of the metabolic activity of [123I]iodometomidate revealed rapid metabolic inactivation in vivo by esterases limiting the radiation doses achievable in target tissue. Thus, metomidate derivatives more resistant to rapid degradation but still maintaining high avidity to adrenal CYP11B enzymes are currently under development and show first promising results [24]. They could allow both a lower radiation exposure during imaging and a significantly higher effective dose in the targeted treatment of ACC lesions.
References
Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y, Bornstein SR (2004) The clinically inapparent adrenal mass: update in diagnosis and management. Endocr Rev 25:309–340
Song JH, Chaudhry FS, Mayo-Smith WW (2008) The incidental adrenal mass on CT: prevalence of adrenal disease in 1,049 consecutive adrenal masses in patients with no known malignancy. AJR Am J Roentgenol 190:1163–1168
Cawood TJ, Hunt PJ, O'Shea D, Cole D, Soule S (2009) Recommended evaluation of adrenal incidentalomas is costly, has high false-positive rates and confers a risk of fatal cancer that is similar to the risk of the adrenal lesion becoming malignant; time for a rethink? Eur J Endocrinol 161:513–527
Petersenn S, Richter PA, Broemel T et al (2015) Computed tomography criteria for discrimination of adrenal adenomas and adrenocortical carcinomas: analysis of the German ACC registry. Eur J Endocrinol 172:415–422
Boland GW, Lee MJ, Gazelle GS, Halpern EF, McNicholas MM, Mueller PR (1998) Characterization of adrenal masses using unenhanced CT: an analysis of the CT literature. AJR Am J Roentgenol 171:201–204
Sangwaiya MJ, Boland GW, Cronin CG, Blake MA, Halpern EF, Hahn PF (2010) Incidental adrenal lesions: accuracy of characterization with contrast-enhanced washout multidetector CT—10-minute delayed imaging protocol revisited in a large patient cohort. Radiology 256:504–510
O'Neill CJ, Spence A, Logan B et al (2010) Adrenal incidentalomas: risk of adrenocortical carcinoma and clinical outcomes. J Surg Oncol 102:450–453
Williams AR, Hammer GD, Else T (2014) Transcutaneous biopsy of adrenocortical carcinoma is rarely helpful in diagnosis, potentially harmful, but does not affect patient outcome. Eur J Endocrinol 170:829–835
Nogueira TM, Lirov R, Caoili EM et al (2015) Radiographic characteristics of adrenal masses preceding the diagnosis of adrenocortical cancer. Horm Cancer 6:176–181
Ozsari L, Kutahyalioglu M, Elsayes KM et al (2015) Preexisting adrenal masses in patients with adrenocortical carcinoma: clinical and radiological factors contributing to delayed diagnosis. Endocrine
Khan M, Caoili EM, Davenport MS et al (2014) CT imaging characteristics of oncocytic adrenal neoplasms (OANs): comparison with adrenocortical carcinomas. Abdom Imaging 39:86–91
Shulkin BL, Thompson NW, Shapiro B, Francis IR, Sisson JC (1999) Pheochromocytomas: imaging with 2-[fluorine-18]fluoro-2-deoxy-D-glucose PET. Radiology 212:35–41
Han SJ, Kim TS, Jeon SW et al (2007) Analysis of adrenal masses by 18F-FDG positron emission tomography scanning. Int J Clin Pract 61:802–809
Ansquer C, Scigliano S, Mirallie E et al (2010) 18F-FDG PET/CT in the characterization and surgical decision concerning adrenal masses: a prospective multicentre evaluation. Eur J Nucl Med Mol Imaging 37:1669–1678
Takeuchi S, Balachandran A, Habra MA et al (2014) Impact of (1)(8)F-FDG PET/CT on the management of adrenocortical carcinoma: analysis of 106 patients. Eur J Nucl Med Mol Imaging 41:2066–2073
Juhlin C, Tornblom S, Rastad J et al (1998) Differential diagnosis in adrenal gland tumors using PET and 11C-metomidate. Nord Med 113:306–307
Minn H, Salonen A, Friberg J et al (2004) Imaging of adrenal incidentalomas with PET using (11)C-metomidate and (18)F-FDG. J Nucl Med 45:972–979
Hennings J, Lindhe O, Bergstrom M, Langstrom B, Sundin A, Hellman P (2006) [11C]metomidate positron emission tomography of adrenocortical tumors in correlation with histopathological findings. J Clin Endocrinol Metab 91:1410–1414
Zettinig G, Mitterhauser M, Wadsak W et al (2004) Positron emission tomography imaging of adrenal masses: (18)F-fluorodeoxyglucose and the 11beta-hydroxylase tracer (11)C-metomidate. Eur J Nucl Med Mol Imaging 31:1224–1230
Kreissl MC, Schirbel A, Fassnacht M et al (2013) [(1)(2)(3)I]Iodometomidate imaging in adrenocortical carcinoma. J Clin Endocrinol Metab 98:2755–2764
Fassnacht M, Terzolo M, Allolio B et al (2012) Combination chemotherapy in advanced adrenocortical carcinoma. N Engl J Med 366:2189–2197
Hahner S, Kreissl MC, Fassnacht M et al (2013) Functional characterization of adrenal lesions using [123I]IMTO-SPECT/CT. J Clin Endocrinol Metab 98:1508–1518
Hahner S, Kreissl MC, Fassnacht M et al (2012) [131I]iodometomidate for targeted radionuclide therapy of advanced adrenocortical carcinoma. J Clin Endocrinol Metab 97:914–922
Hahner S, Heinze B, Herrmann K et al (2015) [123/131I] azetidinylamide—a novel radiotracer for diagnosis and treatment of adrenocortical tumours—from bench to bedside. Abstract band of the 17th European Congress of Endocrinology Endocrine Abstracts (2015) 37 OC1.3
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hahner, S., Caoili, E. & Else, T. 5th International ACC Symposium: Imaging for Diagnosis and Surveillance of Adrenal Tumors—New Advances and Reviews of Old Concepts. HORM CANC 7, 40–43 (2016). https://doi.org/10.1007/s12672-015-0245-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-015-0245-y