Abstract
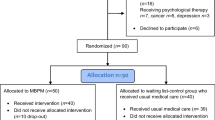
Findings from clinical trials of mindfulness-based interventions (MBI) support significant effects on chronic pain, yet the mechanisms underlying these effects are not well understood. A limitation of current research is reliance on global measures of functioning or narrow, self-report ratings of chronic pain severity. The present research aims to explore potential mechanisms that may explain the effects of MBIs on chronic pain by focusing on acute pain ratings, using quantitative sensory pain testing (QST) rather than chronic pain ratings. Thirty-six patients (10 men, 26 women, mean age = 58.03, ± 14.9) with chronic low back pain (CLBP) were randomly assigned to an 8-week MBI or wait-list control. QST measures of thermal and pain thresholds, as well as pain ratings to fixed stimuli, self-report measures of chronic pain severity, and interference with daily activities were assessed at baseline and after 8 weeks. We found a significant group X time interactions in self-report ratings of chronic pain severity (p = .04, ηp2 = .12) and interference (p = .04, ηp2 = .11): The MBI group showed a decrease in ratings while the control group showed an increase. Also, while patients in the control group exhibited an increase in suprathreshold pain ratings over time (p = .03, ηp2 = .15), indicating an apparent sensitization effect to painful stimuli, participants in the MBI group maintained their original ratings. The results suggest that mindfulness practice may have a “buffering effect” for CLBP patients, by attenuating their tendency to facilitate pain experience.



Similar content being viewed by others
References
Al-Obaidi, S., Nelson, R., Al-Awadhi, S., & Spine, N. A.-S. (2000). The role of anticipation and fear of pain in the persistence of avoidance behavior in patients with chronic low back pain. Spine, 25(9), 1126–1131.
Arendt-Nielsen, L., & Yarnitsky, D. (2009). Experimental and clinical applications of quantitative sensory testing applied to skin, muscles and viscera. The Journal of Pain, 10(6), 556–572.
Ballantyne, J. C., & LaForge, K. S. (2007). Opioid dependence and addiction during opioid treatment of chronic pain. Pain, 129(3), 235–255. https://doi.org/10.1016/j.pain.2007.03.028.
Bawa, F. L. M., Mercer, S. W., Atherton, R. J., Clague, F., Keen, A., Scott, N. W., & Bond, C. M. (2015). Does mindfulness improve outcomes in patients with chronic pain? Systematic review and meta-analysis. British Journal of General Practice, 65(635), e387–e400. https://doi.org/10.3399/bjgp15X685297.
Bohlmeijer, E., Prenger, R., Taal, E., & Cuijpers, P. (2010). The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. Journal of Psychosomatic Research, 68(6), 539–544. https://doi.org/10.1016/j.jpsychores.2009.10.005.
Brown, C. A., & Jones, A. K. P. (2013). Psychobiological correlates of improved mental health in patients with musculoskeletal pain after a mindfulness-based pain management program. The Clinical Journal of Pain, 29(3), 233–244. https://doi.org/10.1097/AJP.0b013e31824c5d9f.
Cleeland, C. S., & Ryan, K. M. (1994). Pain assessment: global use of the brief pain inventory. Annals of the Academy of Medicine, Singapore, 23(2), 129–138.
Crombez, G., Vlaeyen, J., Heuts, P., & Pain, R. L. (1999). Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain, 80(1–2), 329–339.
Dworkin, R., Turk, D., Farrar, J., & Haythornthwaite, J. (2005). Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain, 113(1–2), 9–19.
Edwards, R. R., & Fillingim, R. B. (2007). Self-reported pain sensitivity: lack of correlation with pain threshold and tolerance. European Journal of Pain, 11(5), 594–598. https://doi.org/10.1016/j.ejpain.2006.09.008.
Elzahaf, R. A., Tashani, O. A., Unsworth, B. A., & Johnson, M. I. (2012). The prevalence of chronic pain with an analysis of countries with a human development index less than 0.9: a systematic review without meta-analysis. Current Medical Research and Opinion, 28(7), 1221–1229. https://doi.org/10.1185/03007995.2012.703132.
Esmer, G., Blum, J., Rulf, J., & Pier, J. (2010). Mindfulness-based stress reduction for failed back surgery syndrome: a randomized controlled trial. Journal of the American Osteopathic Association, 110(11), 646–652.
Gourlay, D. L., Heit, H. A., & Almahrezi, A. (2005). Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Medicine, 6(2), 107–112. https://doi.org/10.1111/j.1526-4637.2005.05031.x.
Granot, M., Granovsky, Y., Sprecher, E., Nir, R.-R., & Yarnitsky, D. (2006). Contact heat-evoked temporal summation: tonic versus repetitive-phasic stimulation. Pain, 122(3), 295–305. https://doi.org/10.1016/j.pain.2006.02.003.
Grant, J. a., & Rainville, P. (2009). Pain sensitivity and analgesic effects of mindful states in Zen meditators: a cross-sectional study. Psychosomatic Medicine, 71(1), 106–114. https://doi.org/10.1097/PSY.0b013e31818f52ee.
Grant, J. A., Courtemanche, J., Duerden, E. G., Duncan, G. H., & Rainville, P. (2010). Cortical thickness and pain sensitivity in zen meditators. Emotion, 10(1), 43–53. https://doi.org/10.1037/a0018334.
Greenberg, J., Reiner, K., Meiran, N., Buchner, A., & Goolkasian, P. (2012). “Mind the trap”: mindfulness practice reduces cognitive rigidity. PLoS One, 7(5), e36206. https://doi.org/10.1371/journal.pone.0036206.
Grosen, K., Fischer, I., & Olesen, A. (2013). Can quantitative sensory testing predict responses to analgesic treatment? European Journal of Pain, 17(9), 1267–1280.
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: model, processes and outcomes. Behaviour Research and Therapy. https://doi.org/10.1016/j.brat.2005.06.006.
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary. General Hospital Psychiatry, 4(1), 33–47.
Kabat-Zinn, J., Massion, A., Hebert, J., & Rosenbaum, E. (1998). Meditation. In J. C. Holland (Ed.), Textbook on Psychooncology. Oxford: Oxford University Press.
Lutz, A., McFarlin, D., Perlman, D., Salomons, T., & Davidson, R. (2013). Altered anterior insula activation during anticipation and experience of painful stimuli in expert meditators. Neuroimage, 64, 538–546.
Martell, B. A., O’Connor, P. G., Kerns, R. D., Becker, W. C., Morales, K. H., Kosten, T. R., & Fiellin, D. A. (2007). Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Annals of Internal Medicine. American College of Physicians. https://doi.org/10.7326/0003-4819-146-2-200701160-00006.
Morone, N. E., Greco, C. M., & Weiner, D. K. (2008). Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain, 134(3), 310–319. https://doi.org/10.1016/j.pain.2007.04.038.
Neville, A., Peleg, R., Singer, Y., & Sherf, M. (2008). Chronic pain: a population-based study. The Israel Medical Association Journal, 10(10), 676–680.
Perlman, D. M., Salomons, T. V., Davidson, R. J., & Lutz, A. (2010). Differential effects on pain intensity and unpleasantness of two meditation practices. Emotion, 10(1), 65–71. https://doi.org/10.1037/a0018440.
Pfau, D. B., Geber, C., Birklein, F., & Treede, R.-D. (2012). Quantitative sensory testing of neuropathic pain patients: potential mechanistic and therapeutic implications. Current Pain and Headache Reports, 16(3), 199–206. https://doi.org/10.1007/s11916-012-0261-3.
Pfingsten, M., Leibing, E., Harter, W., Kröner-Herwig, B., Hempel, D., Kronshage, U., & Hildebrandt, J. (2001). Fear-avoidance behavior and anticipation of pain in patients with chronic low back pain: a randomized controlled study. Pain Medicine, 2(4), 259–266. https://doi.org/10.1046/j.1526-4637.2001.01044.x.
Phillips, K., & Clauw, D. J. (2011). Central pain mechanisms in chronic pain states--maybe it is all in their head. Best Practice & Research. Clinical Rheumatology, 25(2), 141–154. https://doi.org/10.1016/j.berh.2011.02.005.
Ploghaus, A., Tracey, I., Gati, J., Clare, S., Menon, R., Matthews, P., & Rawlins, J. (1999). Dissociating pain from its anticipation in the human brain. Science, 284(5422), 1979–1981.
Reiner, K., Tibi, L., & Lipsitz, J. D. (2013). Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Medicine, 14(2), 230–242. https://doi.org/10.1111/pme.12006.
Rosier, E. M., Iadarola, M. J., & Coghill, R. C. (2002). Reproducibility of pain measurement and pain perception. Pain, 98(1–2), 205–216. https://doi.org/10.1016/S0304-3959(02)00048-9.
Segal, Z., Williams, J., & Teasdale, J. (2002). Mindfulness-based cognitive therapy for depression: a new approach to relapse prevention. New York: Guilford.
Shvartzman, P., Friger, M., Shani, A., & Barak, F. (2003). Pain control in ambulatory cancer patients—Can we do better? Journal of Pain and Symptom Management, 26(2), 716–722.
Staud, R. (2009). Abnormal pain modulation in patients with spatially distributed chronic pain: fibromyalgia. Rheumatic Disease Clinics of North America. https://doi.org/10.1016/j.rdc.2009.05.006.
Staud, R. (2012). Abnormal endogenous pain modulation is a shared characteristic of many chronic pain conditions. Expert Review of Neurotherapeutics, 12(5), 577–585. https://doi.org/10.1586/ern.12.41.
Toblin, R. L., Mack, K. A., Perveen, G., & Paulozzi, L. J. (2011). A population-based survey of chronic pain and its treatment with prescription drugs. Pain, 152(6), 1249–1255. https://doi.org/10.1016/j.pain.2010.12.036.
Valencia, C., Fillingim, R. B., & George, S. Z. (2011). Suprathreshold heat pain response is associated with clinical pain intensity for patients with shoulder pain. The Journal of Pain, 12(1), 133–140. https://doi.org/10.1016/j.jpain.2010.06.002.
Veehof, M. M., Trompetter, H. R., Bohlmeijer, E. T., & Schreurs, K. M. G. (2016). Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cognitive Behaviour Therapy, 45(1), 5–31. https://doi.org/10.1080/16506073.2015.1098724.
Yarnitsky, D., Sprecher, E., Zaslansky, R., & Hemli, J. A. (1995). Heat pain thresholds: normative data and repeatability. Pain, 60(3), 329–332. https://doi.org/10.1016/0304-3959(94)00132-X.
Yarnitsky, D., Sprecher, E., Zaslansky, R., & Hemli, J. A. (1996). Multiple session experimental pain measurement. Pain, 67(2–3), 327–333. https://doi.org/10.1016/0304-3959(96)03110-7.
Zeidan, F., Martucci, K. T., Kraft, R. A., Gordon, N. S., McHaffie, J. G., & Coghill, R. C. (2011). Brain mechanisms supporting the modulation of pain by mindfulness meditation. The Journal of Neuroscience, 31(14), 5540–5548. https://doi.org/10.1523/JNEUROSCI.5791-10.2011.
Zgierska, A., Burzinski, C., Cox, J., & Kloke, J. (2016). Mindfulness meditation and cognitive behavioral therapy intervention reduces pain severity and sensitivity in opioid-treated chronic low back pain: pilot findings from a randomized controlled trial. Pain Medicine, 17(10), 1865–1881.
Acknowledgments
Special thanks are given to Dr. Yamima Osher for her professional and generous help. This paper is dedicated to professor Joshua D. Lipsitz, our beloved mentor, who inspired and encouraged the making of this work.
Author information
Authors and Affiliations
Contributions
KRN designed and executed the study, analyzed the data, and wrote the manuscript. PS collaborated with the design and writing of the study. ZZC collaborated in the writing, re-analyzed the data and edited the final manuscript. JDL designed the study and wrote the manuscript.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study before their inclusion in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Reiner, K., Shvartzman, P., Cohen, Z.Z. et al. Assessing the Effectiveness of Mindfulness in the Treatment of Chronic Back Pain: Use of Quantitative Sensory Pain Assessment. Mindfulness 10, 943–952 (2019). https://doi.org/10.1007/s12671-018-1053-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-018-1053-6