Abstract
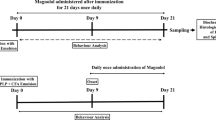
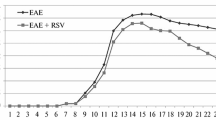
Inflammation, demyelination, glial activation, and oxidative damage are the most pathological hallmarks of multiple sclerosis (MS). Piperine, a main bioactive alkaloid of black pepper, possesses antioxidant, anti-inflammatory, and neuroprotective properties whose therapeutic potential has been less studied in the experimental autoimmune encephalomyelitis (EAE) models. In this study, the efficiency of piperine on progression of EAE model and myelin repair mechanisms was investigated. EAE was induced in female Lewis rats and piperine and its vehicle were daily administrated intraperitoneally from day 8 to 29 post immunization. We found that piperine alleviated neurological deficits and EAE disease progression. Luxol fast blue and H&E staining and immunostaining of lumbar spinal cord cross sections confirmed that piperine significantly reduced the extent of demyelination, inflammation, immune cell infiltration, microglia, and astrocyte activation. Gene expression analysis in lumbar spinal cord showed that piperine treatment decreased the level of pro-inflammatory cytokines (TNF-α, IL-1β) and iNOS and enhanced IL-10, Nrf2, HO-1, and MBP expressions. Piperine supplementation also enhanced the total antioxidant capacity (FRAP) and reduced the level of oxidative stress marker (MDA) in the CNS of EAE rats. Finally, we found that piperine has anti-apoptotic and neuroprotective effect in EAE through reducing caspase-3 (apoptosis marker) and enhancing BDNF and NeuN expressing cells. This study strongly indicates that piperine has a beneficial effect on the EAE progression and could be considered as a potential therapeutic target for MS treatment. Upcoming clinical trials will provide a deeper understanding of piperine’s role for the treatment of the MS.
Graphical abstract









Similar content being viewed by others
Availability of Data and Materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Rezapour A, Almasian Kia A, Goodarzi S, Hasoumi M, Nouraei Motlagh S, Vahedi S (2017) The impact of disease characteristics on multiple sclerosis patients’ quality of life. Epidemiol Health 39:e2017008. https://doi.org/10.4178/epih.e2017008
Burrows DJ, McGown A, Jain SA, De Felice M, Ramesh TM, Sharrack B, Majid A (2019) Animal models of multiple sclerosis: from rodents to zebrafish. Mult Scler 25(3):306–324. https://doi.org/10.1177/1352458518805246
Farooqi N, Gran B, Constantinescu CS (2010) Are current disease-modifying therapeutics in multiple sclerosis justified on the basis of studies in experimental autoimmune encephalomyelitis? J Neurochem 115(4):829–844. https://doi.org/10.1111/j.1471-4159.2010.06982.x
Hauser SL, Oksenberg JR (2006) The neurobiology of multiple sclerosis: genes, inflammation, and neurodegeneration. Neuron 52(1):61–76. https://doi.org/10.1016/j.neuron.2006.09.011
Constantinescu CS, Farooqi N, O’Brien K, Gran B (2011) Experimental autoimmune encephalomyelitis (EAE) as a model for multiple sclerosis (MS). Br J Pharmacol 164(4):1079–1106
Fransson J, Gómez-Conde AI, Romero-Imbroda J, Fernández O, Leyva L, de Fonseca FR, Chun J, Louapre C, Van-Evercooren AB, Zujovic V (2021) Activation of macrophages by lysophosphatidic acid through the lysophosphatidic acid receptor 1 as a novel mechanism in multiple sclerosis pathogenesis. Mol Neurobiol 58(2):470–482
Borggrewe M, Grit C, Vainchtein ID, Brouwer N, Wesseling EM, Laman JD, Eggen BJL, Kooistra SM, Boddeke E (2021) Regionally diverse astrocyte subtypes and their heterogeneous response to EAE. Glia 69(5):1140–1154. https://doi.org/10.1002/glia.23954
Karpus WJ (2020) Cytokines and chemokines in the pathogenesis of experimental autoimmune encephalomyelitis. J Immunol 204(2):316–326. https://doi.org/10.4049/jimmunol.1900914
Meyer R, Weissert R, Diem R, Storch MK, de Graaf KL, Kramer B, Bähr M (2001) Acute neuronal apoptosis in a rat model of multiple sclerosis. J Neurosci 21(16):6214–6220
Stanislaus R, Gilg AG, Singh AK, Singh I (2005) N-acetyl-L-cysteine ameliorates the inflammatory disease process in experimental autoimmune encephalomyelitis in Lewis rats. J Autoimmune Dis 2(1):4. https://doi.org/10.1186/1740-2557-2-4
Gilgun-Sherki Y, Melamed E, Offen D (2004) The role of oxidative stress in the pathogenesis of multiple sclerosis: the need for effective antioxidant therapy. J Neurol 251(3):261–268
Goldschmidt C, McGinley MP (2021) Advances in the treatment of multiple sclerosis. Neurol Clin 39(1):21–33. https://doi.org/10.1016/j.ncl.2020.09.002
Lee MJ, Jang M, Choi J, Chang BS, Kim DY, Kim SH, Kwak YS, Oh S, Lee JH, Chang BJ, Nah SY, Cho IH (2016) Korean red ginseng and ginsenoside-Rb1/-Rg1 alleviate experimental autoimmune encephalomyelitis by suppressing Th1 and Th17 cells and upregulating regulatory T cells. Mol Neurobiol 53(3):1977–2002. https://doi.org/10.1007/s12035-015-9131-4
Minagar A (2013) Current and future therapies for multiple sclerosis. Scientifica (Cairo) 2013:249101. https://doi.org/10.1155/2013/249101
Foti Cuzzola V, Palella E, Celi D, Barresi M, Giacoppo S, Bramanti P, Marino S (2012) Pharmacogenomic update on multiple sclerosis: a focus on actual and new therapeutic strategies. Pharmacogenomics J 12(6):453–461. https://doi.org/10.1038/tpj.2012.41
Wang C, Cai Z, Wang W, Wei M, Kou D, Li T, Yang Z, Guo H, Le W, Li S (2019) Piperine attenuates cognitive impairment in an experimental mouse model of sporadic Alzheimer’s disease. J Nutr Biochem 70:147–155
Shrivastava P, Vaibhav K, Tabassum R, Khan A, Ishrat T, Khan MM, Ahmad A, Islam F, Safhi MM, Islam F (2013) Anti-apoptotic and anti-inflammatory effect of piperine on 6-OHDA induced Parkinson’s rat model. J Nutr Biochem 24(4):680–687. https://doi.org/10.1016/j.jnutbio.2012.03.018
Starossom SC, Mascanfroni ID, Imitola J, Cao L, Raddassi K, Hernandez SF, Bassil R, Croci DO, Cerliani JP, Delacour D, Wang Y, Elyaman W, Khoury SJ, Rabinovich GA (2012) Galectin-1 deactivates classically activated microglia and protects from inflammation-induced neurodegeneration. Immunity 37(2):249–263. https://doi.org/10.1016/j.immuni.2012.05.023
Gutierrez-Miranda B, Gallardo I, Melliou E, Cabero I, Alvarez Y, Magiatis P, Hernandez M, Nieto ML (2020) Oleacein attenuates the pathogenesis of experimental autoimmune encephalomyelitis through both antioxidant and anti-inflammatory effects. Antioxidants (Basel) 9(11). https://doi.org/10.3390/antiox9111161
Qureshi M, Al-Suhaimi EA, Wahid F, Shehzad O, Shehzad A (2018) Therapeutic potential of curcumin for multiple sclerosis. Neurol Sci 39(2):207–214. https://doi.org/10.1007/s10072-017-3149-5
Mohajeri M, Sadeghizadeh M, Najafi F, Javan M (2015) Polymerized nano-curcumin attenuates neurological symptoms in EAE model of multiple sclerosis through down regulation of inflammatory and oxidative processes and enhancing neuroprotection and myelin repair. Neuropharmacology 99:156–167
Muthian G, Bright JJ (2004) Quercetin, a flavonoid phytoestrogen, ameliorates experimental allergic encephalomyelitis by blocking IL-12 signaling through JAK-STAT pathway in T lymphocyte. J Clin Immunol 24(5):542–552. https://doi.org/10.1023/B:JOCI.0000040925.55682.a5
Zarai Z, Boujelbene E, Salem NB, Gargouri Y, Sayari A (2013) Antioxidant and antimicrobial activities of various solvent extracts, piperine and piperic acid from Piper nigrum. LWT Food Sci Technol 50(2):634–641
Buagaew A, Poomipark N (2020) Protective effect of piperine from Piper chaba fruits on LPS-induced inflammation in human intestinal cell line. J Med Plants Res 14(9):438–444
Vaibhav K, Shrivastava P, Javed H, Khan A, Ahmed ME, Tabassum R, Khan MM, Khuwaja G, Islam F, Siddiqui MS (2012) Piperine suppresses cerebral ischemia–reperfusion-induced inflammation through the repression of COX-2, NOS-2, and NF-κB in middle cerebral artery occlusion rat model. Mol Cell Biochem 367(1):73–84
Li S, Wang C, Wang M, Li W, Matsumoto K, Tang Y (2007) Antidepressant like effects of piperine in chronic mild stress treated mice and its possible mechanisms. Life Sci 80(15):1373–1381
Mao K, Lei D, Zhang H, You C (2017) Anticonvulsant effect of piperine ameliorates memory impairment, inflammation and oxidative stress in a rat model of pilocarpine-induced epilepsy. Exp Ther Med 13(2):695–700
Qin B, Yang K, Cao R (2020) Synthesis, radical-scavenging activities, and protective effects against AAPH-induced oxidative damage in DNA and erythrocytes of piperine derivatives. J Chem 2020
Ngo QT, Tran PT, Tran MH, Kim JA, Rho SS, Lim CH, Kim JC, Woo MH, Choi JS, Lee JH (2017) Alkaloids from Piper nigrum exhibit antiinflammatory activity via activating the Nrf2/HO1 pathway. Phytother Res 31(4):663–670
Roshanbakhsh H, Salmani ME, Dehghan S, Nazari A, Javan M, Pourabdolhossein F (2020) Piperine ameliorated memory impairment and myelin damage in lysolecethin induced hippocampal demyelination. Life Sci 253:117671
Hua S, Liu J, Zhang Y, Li J, Zhang X, Dong L, Zhao Y, Fu X (2019) Piperine as a neuroprotective functional component in rats with cerebral ischemic injury. Food Sci Nutr 7(11):3443–3451. https://doi.org/10.1002/fsn3.1185
Chonpathompikunlert P, Wattanathorn J, Muchimapura S (2010) Piperine, the main alkaloid of Thai black pepper, protects against neurodegeneration and cognitive impairment in animal model of cognitive deficit like condition of Alzheimer’s disease. Food Chem Toxicol 48(3):798–802
Bi Y, Qu PC, Wang QS, Zheng L, Liu HL, Luo R, Chen XQ, Ba YY, Wu X, Yang H (2015) Neuroprotective effects of alkaloids from Piper longum in a MPTP-induced mouse model of Parkinson’s disease. Pharm Biol 53(10):1516–1524. https://doi.org/10.3109/13880209.2014.991835
Anissian D, Ghasemi-Kasman M, Khalili-Fomeshi M, Akbari A, Hashemian M, Kazemi S, Moghadamnia AA (2018) Piperine-loaded chitosan-STPP nanoparticles reduce neuronal loss and astrocytes activation in chemical kindling model of epilepsy. Int J Biol Macromol 107:973–983
Liu Z, Hu Q, Wang W, Lu S, Wu D, Ze S, He J, Huang Y, Chen W, Xu Y (2020) Natural product piperine alleviates experimental allergic encephalomyelitis in mice by targeting dihydroorotate dehydrogenase. Biochem Pharmacol 177:114000
Khalili-Fomeshi M, Azizi MG, Esmaeili MR, Gol M, Kazemi S, Ashrafpour M, Moghadamnia AA, Hosseinzadeh S (2018) Piperine restores streptozotocin-induced cognitive impairments: insights into oxidative balance in cerebrospinal fluid and hippocampus. Behav Brain Res 337:131–138
Correia AO, Cruz AAP, Aquino ATRd, Diniz JRG, Santana KBF, Cidade PIM, Peixoto JD, Lucetti DL, Nobre MEP, Cruz GMPd (2015) Neuroprotective effects of piperine, an alkaloid from the Piper genus, on the Parkinson’s disease model in rats.
Beeton C, Garcia A, Chandy KG (2007) Induction and clinical scoring of chronic-relapsing experimental autoimmune encephalomyelitis. JoVE J Vis Exp (5):e224
Ebrahim-Tabar F, Nazari A, Pouramir M, Ashrafpour M, Pourabdolhossein F (2020) Arbutin improves functional recovery and attenuates glial activation in lysolecethin-induced demyelination model in rat optic chiasm. Mol Neurobiol 57(7):3228–3242. https://doi.org/10.1007/s12035-020-01962-x
Benzie I, Devaki M (2018) The ferric reducing/antioxidant power (FRAP) assay for non-enzymatic antioxidant capacity: concepts, procedures, limitations and applications. Measurement of antioxidant activity & capacity: recent trends and applications. Wiley, New York, pp 77–106
Benzie IF, Strain JJ (1996) The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: the FRAP assay. Anal Biochem 239(1):70–76
Chen T-S, Liou S-Y, Wu H-C, Tsai F-J, Tsai C-H, Huang C-Y, Chang Y-L (2010) New analytical method for investigating the antioxidant power of food extracts on the basis of their electron-donating ability: comparison to the ferric reducing/antioxidant power (FRAP) assay. J Agric Food Chem 58(15):8477–8480
Ghani MA, Barril C, Bedgood DR Jr, Prenzler PD (2017) Measurement of antioxidant activity with the thiobarbituric acid reactive substances assay. Food Chem 230:195–207
Pourabdolhossein F, Mozafari S, Morvan-Dubois G, Mirnajafi-Zadeh J, Lopez-Juarez A, Pierre-Simons J, Demeneix BA, Javan M (2014) Nogo receptor inhibition enhances functional recovery following lysolecithin-induced demyelination in mouse optic chiasm. PLoS ONE 9(9):e106378. https://doi.org/10.1371/journal.pone.0106378
Mousavi Majd A, Ebrahim Tabar F, Afghani A, Ashrafpour S, Dehghan S, Gol M, Ashrafpour M, Pourabdolhossein F (2018) Inhibition of GABA A receptor improved spatial memory impairment in the local model of demyelination in rat hippocampus. Behav Brain Res 336:111–121. https://doi.org/10.1016/j.bbr.2017.08.046
Mandler M, Valera E, Rockenstein E, Mante M, Weninger H, Patrick C, Adame A, Schmidhuber S, Santic R, Schneeberger A, Schmidt W, Mattner F, Masliah E (2015) Active immunization against alpha-synuclein ameliorates the degenerative pathology and prevents demyelination in a model of multiple system atrophy. Mol Neurodegener 10:10. https://doi.org/10.1186/s13024-015-0008-9
Seno A, Maruhashi T, Kaifu T, Yabe R, Fujikado N, Ma G, Ikarashi T, Kakuta S, Iwakura Y (2015) Exacerbation of experimental autoimmune encephalomyelitis in mice deficient for DCIR, an inhibitory C-type lectin receptor. Exp Anim 64(2):109–119. https://doi.org/10.1538/expanim.14-0079
Okuda Y, Okuda M, Bernard CC (2002) The suppression of T cell apoptosis influences the severity of disease during the chronic phase but not the recovery from the acute phase of experimental autoimmune encephalomyelitis in mice. J Neuroimmunol 131(1–2):115–125
Pourabdolhossein F, Gil-Perotin S, Garcia-Belda P, Dauphin A, Mozafari S, Tepavcevic V, Manuel Garcia Verdugo J, Baron-Van Evercooren A (2017) Inflammatory demyelination induces ependymal modifications concomitant to activation of adult (SVZ) stem cell proliferation. Glia 65(5):756–772. https://doi.org/10.1002/glia.23124
Dendrou CA, Fugger L, Friese MA (2015) Immunopathology of multiple sclerosis. Nat Rev Immunol 15(9):545–558. https://doi.org/10.1038/nri3871
Linker R, Gold R, Luhder F (2009) Function of neurotrophic factors beyond the nervous system: inflammation and autoimmune demyelination. Crit Rev Immunol 29(1)
Altin JG, Sloan EK (1997) The role of CD45 and CD45-associated molecules in T cell activation. Immunol Cell Biol 75(5):430–445
Kim RY, Hoffman AS, Itoh N, Ao Y, Spence R, Sofroniew MV, Voskuhl RR (2014) Astrocyte CCL2 sustains immune cell infiltration in chronic experimental autoimmune encephalomyelitis. J Neuroimmunol 274(1–2):53–61. https://doi.org/10.1016/j.jneuroim.2014.06.009
Berard JL, Wolak K, Fournier S, David S (2010) Characterization of relapsing-remitting and chronic forms of experimental autoimmune encephalomyelitis in C57BL/6 mice. Glia 58(4):434–445. https://doi.org/10.1002/glia.20935
Choudhury MG, Saha N (2016) Induction of inducible nitric oxide synthase by lipopolysaccharide and the influences of cell volume changes, stress hormones and oxidative stress on nitric oxide efflux from the perfused liver of air-breathing catfish Heteropneustes fossilis. PLoS One 11(3):e0150469. https://doi.org/10.1371/journal.pone.0150469
Kim J, Cha YN, Surh YJ (2010) A protective role of nuclear factor-erythroid 2-related factor-2 (Nrf2) in inflammatory disorders. Mutat Res 690(1–2):12–23. https://doi.org/10.1016/j.mrfmmm.2009.09.007
Paine A, Eiz-Vesper B, Blasczyk R, Immenschuh S (2010) Signaling to heme oxygenase-1 and its anti-inflammatory therapeutic potential. Biochem Pharmacol 80(12):1895–1903. https://doi.org/10.1016/j.bcp.2010.07.014
Janero DR (1990) Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of lipid peroxidation and peroxidative tissue injury. Free Radic Biol Med 9(6):515–540. https://doi.org/10.1016/0891-5849(90)90131-2
D’amelio M, Cavallucci V, Cecconi F (2010) Neuronal caspase-3 signaling: not only cell death. Cell Death Diff 17(7):1104–1114
Martinez B, Peplow PV (2020) Protective effects of pharmacological therapies in animal models of multiple sclerosis: a review of studies 2014–2019. Neural Regen Res 15(7):1220–1234. https://doi.org/10.4103/1673-5374.272572
McFarland HF, Martin R (2007) Multiple sclerosis: a complicated picture of autoimmunity. Nat Immunol 8(9):913–919. https://doi.org/10.1038/ni1507
Wang-Sheng C, Jie A, Jian-Jun L, Lan H, Zeng-Bao X, Chang-Qing L (2017) Piperine attenuates lipopolysaccharide (LPS)-induced inflammatory responses in BV2 microglia. Int Immunopharmacol 42:44–48
Doucette CD, Rodgers G, Liwski RS, Hoskin DW (2015) Piperine from black pepper inhibits activation-induced proliferation and effector function of T lymphocytes. J Cell Biochem 116(11):2577–2588
Murunikkara V, Pragasam SJ, Kodandaraman G, Sabina EP, Rasool M (2012) Anti-inflammatory effect of piperine in adjuvant-induced arthritic rats—a biochemical approach. Inflammation 35(4):1348–1356
Jahan-Abad AJ, Karima S, Shateri S, Baram SM, Rajaei S, Morteza-Zadeh P, Borhani-Haghighi M, Salari AA, Nikzamir A, Gorji A (2020) Serum pro-inflammatory and anti-inflammatory cytokines and the pathogenesis of experimental autoimmune encephalomyelitis. Neuropathology 40(1):84–92. https://doi.org/10.1111/neup.12612
Beck J, Rondot P, Catinot L, Falcoff E, Kirchner H, Wietzerbin J (1988) Increased production of interferon gamma and tumor necrosis factor precedes clinical manifestation in multiple sclerosis: do cytokines trigger off exacerbations? Acta Neurol Scand 78(4):318–323. https://doi.org/10.1111/j.1600-0404.1988.tb03663.x
Bogdan C, Paik J, Vodovotz Y, Nathan C (1992) Contrasting mechanisms for suppression of macrophage cytokine release by transforming growth factor-beta and interleukin-10. J Biol Chem 267(32):23301–23308
da Cruz GM, Felipe CF, Scorza FA, da Costa MA, Tavares AF, Menezes ML, de Andrade GM, Leal LK, Brito GA, da Graca N-M, Cavalheiro EA, de Barros Viana GS (2013) Piperine decreases pilocarpine-induced convulsions by GABAergic mechanisms. Pharmacol Biochem Behav 104:144–153. https://doi.org/10.1016/j.pbb.2013.01.002
Zhai W-J, Zhang Z-B, Xu N-N, Guo Y-F, Qiu C, Li C-Y, Deng G-Z, Guo M-Y (2016) Piperine plays an anti-inflammatory role in Staphylococcus aureus endometritis by inhibiting activation of NF-κB and MAPK pathways in mice. Evid Based Complement Alternat Med 2016
Liu T, Zhang L, Joo D, Sun SC (2017) NF-kappaB signaling in inflammation. Signal Transduct Target Ther 2.https://doi.org/10.1038/sigtrans.2017.23
Saraiva M, O’Garra A (2010) The regulation of IL-10 production by immune cells. Nat Rev Immunol 10(3):170–181. https://doi.org/10.1038/nri2711
Couper KN, Blount DG, Riley EM (2008) IL-10: the master regulator of immunity to infection. J Immunol 180(9):5771–5777
Salmaggi A, Dufour A, Eoli M, Corsini E, La Mantia L, Massa G, Nespolo A, Milanese C (1996) Low serum interleukin-10 levels in multiple sclerosis: further evidence for decreased systemic immunosuppression? J Neurol 243(1):13–17. https://doi.org/10.1007/BF00878525
Correale J, Gilmore W, McMillan M, Li S, McCarthy K, Le T, Weiner LP (1995) Patterns of cytokine secretion by autoreactive proteolipid protein-specific T cell clones during the course of multiple sclerosis. J Immunol 154(6):2959–2968
Samoilova EB, Horton JL, Chen Y (1998) Acceleration of experimental autoimmune encephalomyelitis in interleukin-10-deficient mice: roles of interleukin-10 in disease progression and recovery. Cell Immunol 188(2):118–124
Carvalho Jennings Pereira WL, Marques Andrade R, Muliterno Pelegrino L, Donizete Borelli S, Kaimen-Maciel DR (2013) Cytokine profile in relapsing-remitting multiple sclerosis patients and the association between progression and activity of the disease. Mol Med Rep 7(3):1010–1020
Pang Y, Fan LW, Tien LT, Dai X, Zheng B, Cai Z, Lin RC, Bhatt A (2013) Differential roles of astrocyte and microglia in supporting oligodendrocyte development and myelination in vitro. Brain Behav 3(5):503–514. https://doi.org/10.1002/brb3.152
Traiffort E, Kassoussi A, Zahaf A, Laouarem Y (2020) Astrocytes and microglia as major players of myelin production in normal and pathological conditions. Front Cell Neurosci 14:79. https://doi.org/10.3389/fncel.2020.00079
Miron VE, Boyd A, Zhao JW, Yuen TJ, Ruckh JM, Shadrach JL, van Wijngaarden P, Wagers AJ, Williams A, Franklin RJM, Ffrench-Constant C (2013) M2 microglia and macrophages drive oligodendrocyte differentiation during CNS remyelination. Nat Neurosci 16(9):1211–1218. https://doi.org/10.1038/nn.3469
Haindl MT, Kock U, Zeitelhofer-Adzemovic M, Fazekas F, Hochmeister S (2019) The formation of a glial scar does not prohibit remyelination in an animal model of multiple sclerosis. Glia 67(3):467–481. https://doi.org/10.1002/glia.23556
Thompson KK, Tsirka SE (2020) Guanabenz modulates microglia and macrophages during demyelination. Sci Rep 10(1):1–12
Singh S, Metz I, Amor S, van der Valk P, Stadelmann C, Brück W (2013) Microglial nodules in early multiple sclerosis white matter are associated with degenerating axons. Acta Neuropathol 125(4):595–608
Heppner FL, Greter M, Marino D, Falsig J, Raivich G, Hovelmeyer N, Waisman A, Rulicke T, Prinz M, Priller J, Becher B, Aguzzi A (2005) Experimental autoimmune encephalomyelitis repressed by microglial paralysis. Nat Med 11(2):146–152. https://doi.org/10.1038/nm1177
Lassmann H, van Horssen J (2011) The molecular basis of neurodegeneration in multiple sclerosis. FEBS Lett 585(23):3715–3723
Nair A, Frederick TJ, Miller SD (2008) Astrocytes in multiple sclerosis: a product of their environment. Cell Mol Life Sci 65(17):2702–2720. https://doi.org/10.1007/s00018-008-8059-5
Chen X, Ma X, Jiang Y, Pi R, Liu Y, Ma L (2011) The prospects of minocycline in multiple sclerosis. J Neuroimmunol 235(1–2):1–8. https://doi.org/10.1016/j.jneuroim.2011.04.006
Guo X, Nakamura K, Kohyama K, Harada C, Behanna HA, Watterson DM, Matsumoto Y, Harada T (2007) Inhibition of glial cell activation ameliorates the severity of experimental autoimmune encephalomyelitis. Neurosci Res 59(4):457–466. https://doi.org/10.1016/j.neures.2007.08.014
Yang W, Chen YH, Liu H, Qu HD (2015) Neuroprotective effects of piperine on the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced Parkinson’s disease mouse model. Int J Mol Med 36(5):1369–1376. https://doi.org/10.3892/ijmm.2015.2356
Naeimi R, Safarpour F, Hashemian M, Tashakorian H, Ahmadian SR, Ashrafpour M, Ghasemi-Kasman M (2018) Curcumin-loaded nanoparticles ameliorate glial activation and improve myelin repair in lyolecithin-induced focal demyelination model of rat corpus callosum. Neurosci Lett 674:1–10. https://doi.org/10.1016/j.neulet.2018.03.018
Ghasemi F, Bagheri H, Barreto GE, Read MI, Sahebkar A (2019) Effects of curcumin on microglial cells. Neurotox Res 36(1):12–26. https://doi.org/10.1007/s12640-019-00030-0
Bo L, Dawson TM, Wesselingh S, Mork S, Choi S, Kong PA, Hanley D, Trapp BD (1994) Induction of nitric oxide synthase in demyelinating regions of multiple sclerosis brains. Ann Neurol 36(5):778–786. https://doi.org/10.1002/ana.410360515
Adamczyk B, Adamczyk-Sowa M (2016) New insights into the role of oxidative stress mechanisms in the pathophysiology and treatment of multiple sclerosis. Oxid Med Cell Longev 2016:1973834. https://doi.org/10.1155/2016/1973834
Gaweł S, Wardas M, Niedworok E, Wardas P (2004) Malondialdehyde (MDA) as a lipid peroxidation marker. Wiadomosci Lekarskie (Warsaw, Poland: 1960) 57(9–10):453–455
Yuste JE, Tarragon E, Campuzano CM, Ros-Bernal F (2015) Implications of glial nitric oxide in neurodegenerative diseases. Front Cell Neurosci 9:322
Ljubisavljevic S, Stojanovic I, Pavlovic D, Milojkovic M, Sokolovic D, Stevanovic I, Petrovic A (2013) Suppression of the lipid peroxidation process in the CNS reduces neurological expression of experimentally induced autoimmune encephalomyelitis. Folia Neuropathol 51(1):51–57
AlFadhli S, Mohammed EM, Al Shubaili A (2013) Association analysis of nitric oxide synthases: NOS1, NOS2A and NOS3 genes, with multiple sclerosis. Ann Hum Biol 40(4):368–375
Buendia I, Michalska P, Navarro E, Gameiro I, Egea J, Leon R (2016) Nrf2–ARE pathway: an emerging target against oxidative stress and neuroinflammation in neurodegenerative diseases. Pharmacol Ther 157:84–104
Sivandzade F, Prasad S, Bhalerao A, Cucullo L (2019) NRF2 and NF-қB interplay in cerebrovascular and neurodegenerative disorders: molecular mechanisms and possible therapeutic approaches. Redox Biol 21:101059
Kappos L, Gold R, Miller DH, MacManus DG, Havrdova E, Limmroth V, Polman CH, Schmierer K, Yousry TA, Yang M (2008) Efficacy and safety of oral fumarate in patients with relapsing-remitting multiple sclerosis: a multicentre, randomised, double-blind, placebo-controlled phase IIb study. The Lancet 372(9648):1463–1472
Liu Y, Zhu B, Luo L, Li P, Paty DW, Cynader MS (2001) Heme oxygenase-1 plays an important protective role in experimental autoimmune encephalomyelitis. NeuroReport 12(9):1841–1845
Chora ÂA, Fontoura P, Cunha A, Pais TF, Cardoso S, Ho PP, Lee LY, Sobel RA, Steinman L, Soares MP (2007) Heme oxygenase–1 and carbon monoxide suppress autoimmune neuroinflammation. J Clin Investig 117(2):438–447
Ferguson B, Matyszak MK, Esiri MM, Perry VH (1997) Axonal damage in acute multiple sclerosis lesions. Brain 120(3):393–399
Hobom M, Storch MK, Weissert R, Maier K, Radhakrishnan A, Kramer B, Bähr M, Diem R (2004) Mechanisms and time course of neuronal degeneration in experimental autoimmune encephalomyelitis. Brain Pathol 14(2):148–157
Eldadah BA, Faden AI (2000) Caspase pathways, neuronal apoptosis, and CNS injury. J Neurotrauma 17(10):811–829
Ahmed Z, Doward AI, Pryce G, Taylor DL, Pocock JM, Leonard JP, Baker D, Cuzner ML (2002) A role for caspase-1 and -3 in the pathology of experimental allergic encephalomyelitis: inflammation versus degeneration. Am J Pathol 161(5):1577–1586. https://doi.org/10.1016/S0002-9440(10)64436-7
Gusel’Nikova V, Korzhevskiy D (2015) NeuN as a neuronal nuclear antigen and neuron differentiation marker. Acta Naturae (aнглoязычнaя вepcия) 7(2(25))
Yousef A, Robinson JL, Irwin DJ, Byrne MD, Kwong LK, Lee EB, Xu Y, Xie SX, Rennert L, Suh E (2017) Neuron loss and degeneration in the progression of TDP-43 in frontotemporal lobar degeneration. Acta Neuropathol Commun 5(1):1–15
Makar TK, Trisler D, Sura KT, Sultana S, Patel N, Bever CT (2008) Brain derived neurotrophic factor treatment reduces inflammation and apoptosis in experimental allergic encephalomyelitis. J Neurol Sci 270(1–2):70–76. https://doi.org/10.1016/j.jns.2008.02.011
Fletcher JL, Murray SS, Xiao J (2018) Brain-derived neurotrophic factor in central nervous system myelination: a new mechanism to promote myelin plasticity and repair. Int J Mol Sci 19(12):4131
Van’t Veer A, Du Y, Fischer TZ, Boetig DR, Wood MR, Dreyfus CF, (2009) Brain-derived neurotrophic factor effects on oligodendrocyte progenitors of the basal forebrain are mediated through trkB and the MAP kinase pathway. J Neurosci Res 87(1):69–78
Tongiorgi E, Sartori A, Baj G, Bratina A, Di Cola F, Zorzon M, Pizzolato G (2012) Altered serum content of brain-derived neurotrophic factor isoforms in multiple sclerosis. J Neurol Sci 320(1–2):161–165
Qu Z, Zheng N, Zhang Y, Zhang L, Liu J, Wang Q, Yin L (2016) Preventing the BDNF and NGF loss involved in the effects of cornel iridoid glycoside on attenuation of experimental autoimmune encephalomyelitis in mice. Neurol Res 38(9):831–837. https://doi.org/10.1080/01616412.2016.1200766
Mao QQ, Huang Z, Zhong XM, Xian YF, Ip SP (2014) Brain-derived neurotrophic factor signalling mediates the antidepressant-like effect of piperine in chronically stressed mice. Behav Brain Res 261:140–145. https://doi.org/10.1016/j.bbr.2013.12.020
Liu H, Luo R, Chen X, Liu J, Bi Y, Zheng L, Wu X (2013) Tissue distribution profiles of three antiparkinsonian alkaloids from Piper longum L. in rats determined by liquid chromatography-tandem mass spectrometry. J Chromatogr B Anal Technol Biomed Life Sci 928:78–82. https://doi.org/10.1016/j.jchromb.2013.03.021
Acknowledgements
The authors would like to gratefully appreciate the kind support of Dr. Mohammad Javan from physiology department of Tarbiat Modares University Tehran-Iran and technical assistance of Mrs. Atena Nazari during the study.
Funding
This work was supported by a grant from the Deputy of Research and Technology (No. 724132502), Babol University of Medical Sciences, Babol, Iran, and was performed as a part of Master of Science thesis in Clinical Biochemistry in the Physiology and Biochemistry Departments at Babol University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Reza Nasrnezhad, Sohrab Halalkhor, and Fereshteh Pourabdolhossein. Data analysis and interpretation was done by Reza Nasrnezhad, Farzin Sadeghi, and Fereshteh Pourabdolhossein. The first draft of the manuscript was written by Reza Nasrnezhad and its major revision was performed by Fereshteh Pourabdolhossein. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All experimental procedures of this study were conducted according to the international guidelines for care and use of laboratory animals and approved (Ethic code number: IR.MUBABOL.HRI.REC.1398.315) by the ethical committee of Babol University of Medical Sciences.
Consent to Participate and/or Consent for Publication
It is not applicable in our study because this article does not contain any studies involving human participants performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nasrnezhad, R., Halalkhor, S., Sadeghi, F. et al. Piperine Improves Experimental Autoimmune Encephalomyelitis (EAE) in Lewis Rats Through its Neuroprotective, Anti-inflammatory, and Antioxidant Effects. Mol Neurobiol 58, 5473–5493 (2021). https://doi.org/10.1007/s12035-021-02497-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-021-02497-5