Abstract
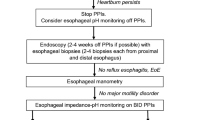
Functional heartburn (FH) is a functional gastro-intestinal disorder characterized by symptoms of heartburn not related to gastro-esophageal reflux. The absence of evidence of reflux-related symptoms relies on absence of esophagitis at endoscopy (including biopsies to exclude eosinophilic esophagitis), a normal esophageal acid exposure during esophageal pH-monitoring together with a negative symptom-reflux association analysis and an unsatisfactory response to proton pump inhibitor therapy. Addition of impedance measurement to pH-monitoring is likely to increase the number of patients with recognized reflux-related symptoms. The pathophysiology of functional heartburn remains largely unknown but involves disturbed esophageal perception and psychological factors such as depression, anxiety and somatization. The treatment of FH remains largely empirical and an individual approach is therefore recommended. The clinician should provide reassurance and refrain from performing too many invasive tests or therapeutic procedures. The use of pain modulators is recommended by most experts despite the lack of appropriate clinical trials to support it.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Locke 3rd GR, Talley NJ, Fett SL, et al. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–56.
Carlsson R, Dent J, Bolling-Sternevald E, et al. The usefulness of a structured questionnaire in the assessment of symptomatic gastroesophageal reflux disease. Scand J Gastroenterol. 1998;33:1023–9.
Bredenoord AJ, Weusten BL, Smout AJ. Symptom association analysis in ambulatory gastro-oesophageal reflux monitoring. Gut. 2005;54:1810–7.
Sifrim D, Castell D, Dent J, et al. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024–31.
Zerbib F, Roman S, Ropert A, et al. Esophageal pH-impedance monitoring and symptom analysis in GERD: a study in patients off and on therapy. Am J Gastroenterol. 2006;101:1956–63.
Clouse RE, Richter J, Heading RC. Functional esophageal disorders. In: Corazziari E, Talley NJ, Thompson WG, Whitehead WE, editors. Rome II—the functional gastrointestinal disorders. 2nd ed. MacLean: Degnon Associates; 2000. p. 247–98.
Galmiche JP, Clouse RE, Balint A, et al. Functional esophageal disorders. Gastroenterology. 2006;130:1459–65.
Fass R, Sifrim D. Management of heartburn not responding to proton pump inhibitors. Gut. 2009;58:295–309.
Shi G, Bruley des Varannes S, Scarpignato C, et al. Reflux related symptoms in patients with normal oesophageal exposure to acid. Gut. 1995;37:457–64.
Trimble KC, Douglas S, Pryde A, et al. Clinical characteristics and natural history of symptomatic but not excess gastroesophageal reflux. Dig Dis Sci. 1995;40:1098–104.
Watson RG, Tham TC, Johnston BT, et al. Double blind cross-over placebo controlled study of omeprazole in the treatment of patients with reflux symptoms and physiological levels of acid reflux—the “sensitive oesophagus”. Gut. 1997;40:587–90.
Sacher-Huvelin S, Gournay J, Amouretti M, et al. Acid-sensitive esophagus: natural history and effect on the quality of life. Comparison with gastroesophageal reflux. Gastroenterol Clin Biol. 2000;24:911–6.
Dent J, Armstrong D, Delaney B, et al. Symptom evaluation in reflux disease: workshop background, processes, terminology, recommendations, and discussion outputs. Gut. 2004;53 Suppl 4:iv1–iv24.
• Savarino E, Marabotto E, Zentilin P, et al. The added value of impedance-pH monitoring to Rome III criteria in distinguishing functional heartburn from non-erosive reflux disease. Dig Liver Dis. 2011;43:542–7. This study demonstrates that pH-impedance monitoring decreases the proportion of patients with functional heartburn since it allows identification of more patients with positive symptom association analysis (compared to pH alone monitoring).
• Frazzoni M, Conigliaro R, Mirante VG, et al. The added value of quantitative analysis of on-therapy impedance-pH parameters in distinguishing refractory non-erosive reflux disease from functional heartburn. Neurogastroenterol Motil. 2011. doi:10.1039/C1AY05569K. This study suggests that pH-impedance on PPIs can help identifying patients with functional heartburn whose characteristics are different from NERD patients.
Aanen MC, Weusten BL, Numans ME, et al. Effect of proton-pump inhibitor treatment on symptoms and quality of life in GERD patients depends on the symptom-reflux association. J Clin Gastroenterol. 2008;42:441–7.
Taghavi SA, Ghasedi M, Saberi-Firoozi M, et al. Symptom association probability and symptom sensitivity index: preferable but still suboptimal predictors of response to high dose omeprazole. Gut. 2005;54:1067–71.
Mainie I, Tutuian R, Shay S, et al. Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut. 2006;55:1398–402.
Lam HG, Breumelhof R, van Berge Henegouwen GP, et al. Temporal relationships between episodes of non-cardiac chest pain and abnormal oesophageal function. Gut. 1994;35:733–6.
Slaughter JC, Goutte M, Rymer JA, et al. Caution about overinterpretation of symptom indexes in reflux monitoring for refractory gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2012; [Epub ahead of print].
Numans ME, Lau J, de Wit NJ, et al. Short-term treatment with proton-pump inhibitors as a test for gastroesophageal reflux disease: a meta-analysis of diagnostic test characteristics. Ann Intern Med. 2004;140:518–27.
Martinez SD, Malagon IB, Garewal HS, et al. Non-erosive reflux disease (NERD)–acid reflux and symptom patterns. Aliment Pharmacol Ther. 2003;17:537–45.
• Zerbib F, Belhocine K, Simon M, et al. Clinical, but not oesophageal pH-impedance, profiles predict response to proton pump inhibitors in gastro-oesophageal reflux disease. Gut. 2012;61:501–6. This study shows that, when multivariate analysis is performed, only clinical features (i.e. no esophagitis, functional disorders and normal or low BMI) are associated with PPI failure. No pH-impedance parameter could predict the response to PPIs.
• Savarino E, Pohl D, Zentilin P, et al. Functional heartburn has more in common with functional dyspepsia than with non-erosive reflux disease. Gut. 2009;58:1185–91. This study show a high prevalence of functional dyspepsia symptoms in patients with functional heartburn.
Lee SY, Lee KJ, Kim SJ, et al. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: a population-based study. Digestion. 2009;79:196–201.
Nojkov B, Rubenstein JH, Adlis SA, et al. The influence of co-morbid IBS and psychological distress on outcomes and quality of life following PPI therapy in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2008;27:473–82.
Jung HK, Halder S, McNally M, et al. Overlap of gastro-oesophageal reflux disease and irritable bowel syndrome: prevalence and risk factors in the general population. Aliment Pharmacol Ther. 2007;26:453–61.
Fass R, Tougas G. Functional heartburn: the stimulus, the pain, and the brain. Gut. 2002;51:885–92.
Fass R, Naliboff B, Higa L, et al. Differential effect of long-term esophageal acid exposure on mechanosensitivity and chemosensitivity in humans. Gastroenterology. 1998;115:1363–73.
Knowles CH, Aziz Q. Visceral hypersensitivity in non-erosive reflux disease. Gut. 2008;57:674–83.
• Vela MF, Craft BM, Sharma N, et al. Refractory heartburn: comparison of intercellular space diameter in documented GERD vs. functional heartburn. Am J Gastroenterol. 2011;106:844–50. This study shows that DIS is associated with NERD but not functional heartburn and may be a marker of GERD.
Farre R, Fornari F, Blondeau K, et al. Acid and weakly acidic solutions impair mucosal integrity of distal exposed and proximal non-exposed human oesophagus. Gut. 2010;59:164–9.
Fried M, Feinle C. The role of fat and cholecystokinin in functional dyspepsia. Gut. 2002;51 Suppl 1:i54–7.
Meyer JH, Lembo A, Elashoff JD, et al. Duodenal fat intensifies the perception of heartburn. Gut. 2001;49:624–8.
Yang M, Li ZS, Xu XR, et al. Characterization of cortical potentials evoked by oesophageal balloon distention and acid perfusion in patients with functional heartburn. Neurogastroenterol Motil. 2006;18:292–9.
Kern MK, Birn RM, Jaradeh S, et al. Identification and characterization of cerebral cortical response to esophageal mucosal acid exposure and distention. Gastroenterology. 1998;115:1353–62.
Kern M, Hofmann C, Hyde J, et al. Characterization of the cerebral cortical representation of heartburn in GERD patients. Am J Physiol Gastrointest Liver Physiol. 2004;286:G174–81.
Yang M, Li ZS, Chen DF, et al. Quantitative assessment and characterization of visceral hyperalgesia evoked by esophageal balloon distention and acid perfusion in patients with functional heartburn, nonerosive reflux disease, and erosive esophagitis. Clin J Pain. 2010;26:326–31.
Fass R, Naliboff BD, Fass SS, et al. The effect of auditory stress on perception of intraesophageal acid in patients with gastroesophageal reflux disease. Gastroenterology. 2008;134:696–705.
Schey R, Dickman R, Parthasarathy S, et al. Sleep deprivation is hyperalgesic in patients with gastroesophageal reflux disease. Gastroenterology. 2007;133:1787–95.
Naliboff BD, Mayer M, Fass R, et al. The effect of life stress on symptoms of heartburn. Psychosom Med. 2004;66:426–34.
Johnston BT, Lewis SA, Collins JS, et al. Acid perception in gastro-oesophageal reflux disease is dependent on psychosocial factors. Scand J Gastroenterol. 1995;30:1–5.
Shapiro M, Green C, Bautista JM, et al. Functional heartburn patients demonstrate traits of functional bowel disorder but lack a uniform increase of chemoreceptor sensitivity to acid. Am J Gastroenterol. 2006;101:1084–91.
Furuta GT, Liacouras CA, Collins MH, et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007;133:1342–63.
Ponce J, Ortiz V, Maroto N, et al. High prevalence of heartburn and low acid sensitivity in patients with idiopathic achalasia. Dig Dis Sci. 2011;56:773–6.
Prakash C, Clouse RE. Value of extended recording time with wireless pH monitoring in evaluating gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2005;3:329–34.
Gonlachanvit S. Are rice and spicy diet good for functional gastrointestinal disorders? J Neurogastroenterol Motil;16:131–8.
Viazis N, Karamanolis G, Vienna E, et al. Selective-serotonin reuptake inhibitors for the treatment of hypersensitive esophagus. Therap Adv Gastroenterol. 2011;4:295–300.
Viazis N, Keyoglou A, Kanellopoulos AK, et al. Selective serotonin reuptake inhibitors for the treatment of hypersensitive esophagus: a randomized, double-blind, placebo-controlled study. Am J Gastroenterol. 2011;Epub ahead of print.
McDonald-Haile J, Bradley LA, Bailey MA, et al. Relaxation training reduces symptom reports and acid exposure in patients with gastroesophageal reflux disease. Gastroenterology. 1994;107:61–9.
Miner Jr PB, Rodriguez-Stanley S, Proskin HM, et al. Tegaserod in patients with mechanical sensitivity and overlapping symptoms of functional heartburn and functional dyspepsia. Curr Med Res Opin. 2008;24:2159–72.
Krarup AL, Ny L, Astrand M, et al. Randomised clinical trial: the efficacy of a transient receptor potential vanilloid 1 antagonist AZD1386 in human oesophageal pain. Aliment Pharmacol Ther. 2011;33:1113–22.
Khajanchee YS, Hong D, Hansen PD, et al. Outcomes of antireflux surgery in patients with normal preoperative 24-hour pH test results. Am J Surg. 2004;187:599–603.
Campos GM, Peters JH, DeMeester TR, et al. Multivariate analysis of factors predicting outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg. 1999;3:292–300.
Mainie I, Tutuian R, Agrawal A, et al. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br J Surg. 2006;93:1483–7.
Broeders JA, Draaisma WA, Bredenoord AJ, et al. Impact of symptom-reflux association analysis on long-term outcome after Nissen fundoplication. Br J Surg. 2011;98:247–54.
Thompson SK, Cai W, Jamieson GG, et al. Recurrent symptoms after fundoplication with a negative pH study–recurrent reflux or functional heartburn? J Gastrointest Surg. 2009;13:54–60.
Arts J, Sifrim D, Rutgeerts P, et al. Influence of radiofrequency energy delivery at the gastroesophageal junction (the Stretta procedure) on symptoms, acid exposure, and esophageal sensitivity to acid perfusion in gastroesophagal reflux disease. Dig Dis Sci. 2007;52:2170–7.
Disclosure
Dr. S. Bruley des Varannes has been a board member for Janssen Cilag, IPRAD Laboratories, Cephalon Laboratories, Mayoli Spindler Laboratories, a consultant for Given Imaging, Novartis, and Danone, and has received payment for lectures from Astra Zeneca, Takeda, and Nycomed; Dr. J. P. Galmiche has been a board member and consultant for Astra Zeneca, and a consultant for Norgine and Xenoport. He has received payment for development of educational presentations from Shire Movetis, travel and accommodation reimbursement from Given Imaging, and support from Mauna Kea Technology; Dr. F. Zerbib has been a board member for Shire Movetis and a consultant for Given Imaging, Shire Movetis, Norgine, Xenoport, and Addex Pharma. He has received payment for lectures from Janssen Cilag, Abbott France, and AstraZeneca, and payment for development of educational presentations from Cephalon, Pfizer, and Nycomed; Dr. M. Simon reported no potential conflicts of interest relevant to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zerbib, F., Bruley des Varannes, S., Simon, M. et al. Functional Heartburn: Definition and Management Strategies. Curr Gastroenterol Rep 14, 181–188 (2012). https://doi.org/10.1007/s11894-012-0255-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11894-012-0255-7