Abstract
Purpose of Review
To introduce recent advances in the understanding of diabetic retinopathy and to summarize current and emerging strategies to treat this common and complex cause of vision loss.
Recent Findings
Advances in retinal imaging and functional analysis indicate that retinal vascular and neural pathologies exist long before the development of clinically visible retinopathy. Such diagnostics could facilitate risk stratification and selective early intervention in high-risk patients. Antagonists of the vascular endothelial growth factor pathway effectively reduce vision loss in diabetes and promote regression of disease severity. Promising new strategies to treat diabetic retinopathy involve novel systemic diabetes therapy and ocular therapies that antagonize angiogenic growth factor signaling, improve blood-retina barrier function and neurovascular coupling, modulate neuroretinal metabolism, or provide neuroprotection.
Summary
Long considered a pure microvasculopathy, diabetic retinopathy in fact affects the neural and vascular retina as well as neurovascular communication. Emerging therapies include those that target neuroretinal dysfunction in addition to those modulating vascular biology.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Centers for Disease Control and Prevention: National Diabetes Statistics Report: Estimates of diabetes and its burden in the United States, 2017. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed June 3, 2019.
Klein R, Knudtson MD, Lee KE, Gangnon R, Klein BE. The Wisconsin Epidemiologic Study of Diabetic Retinopathy XXIII: the twenty-five-year incidence of macular edema in persons with type 1 diabetes. Ophthalmology. 2009;116(3):497–503. https://doi.org/10.1016/j.ophtha.2008.10.016.
Thompson JT, de Bustros S, Michels RG, Rice TA. Results and prognostic factors in vitrectomy for diabetic traction retinal detachment of the macula. Arch Ophthalmol. 1987;105(4):497–502.
Abunajma MA, Al-Dhibi H, Abboud EB, Al Zahrani Y, Alharthi E, Alkharashi A, et al. The outcomes and prognostic factors of vitrectomy in chronic diabetic traction macular detachment. Clin Ophthalmol. 2016;10:1653–61. https://doi.org/10.2147/OPTH.S98555.
Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331(22):1480–7. https://doi.org/10.1056/NEJM199412013312203.
Ip MS, Domalpally A, Sun JK, Ehrlich JS. Long-term effects of therapy with ranibizumab on diabetic retinopathy severity and baseline risk factors for worsening retinopathy. Ophthalmology. 2015;122(2):367–74. https://doi.org/10.1016/j.ophtha.2014.08.048.
• Mitchell P, McAllister I, Larsen M, Staurenghi G, Korobelnik JF, Boyer DS, et al. Evaluating the impact of intravitreal aflibercept on diabetic retinopathy progression in the VIVID-DME and VISTA-DME studies. Ophthalmol Retina. 2018;2(10):988–96. https://doi.org/10.1016/j.oret.2018.02.011. In a sub-analysis of the phase 3 VIVID and VISTA studies in which patients with center-involving DME were treated with two different regimens of aflibercept, more patients receiving aflibercept experienced 2-step improvement in DR severity score compared with those in the laser control arm.
• Wykoff CC, Eichenbaum DA, Roth DB, Hill L, Fung AE, Haskova Z. Ranibizumab induces regression of diabetic retinopathy in most patients at high risk of progression to proliferative diabetic retinopathy. Ophthalmol Retina. 2018;2(10):997–1009. https://doi.org/10.1016/j.oret.2018.06.005. In a post hoc analysis of the phase 3 RISE and RIDE trials in which patients with center-involving DME were treated with two different doses of ranibizumab, more patients receiving ranibizumab experienced 2-step improvement in DR severity score compared with those in the laser control arm. Effects were greatest among patients with baseline severity score of 47/53.
Ashton N. Vascular changes in diabetes with particular reference to the retinal vessels; preliminary report. Br J Ophthalmol. 1949;33(7):407–20. https://doi.org/10.1136/bjo.33.7.407.
Cogan DG. Diabetic retinopathy. N Engl J Med. 1964;270:787–8. https://doi.org/10.1056/NEJM196404092701508.
Toussaint D, Cogan DG, Kuwabara T. Extravascular lesions of diabetic retinopathy. Arch Ophthalmol. 1962;67:42–7.
de Carlo TE, Chin AT, Bonini Filho MA, Adhi M, Branchini L, Salz DA, et al. Detection of microvascular changes in eyes of patients with diabetes but not clinical diabetic retinopathy using optical coherence tomography angiography. Retina. 2015;35(11):2364–70. https://doi.org/10.1097/IAE.0000000000000882.
• Dimitrova G, Chihara E, Takahashi H, Amano H, Okazaki K. Quantitative retinal optical coherence tomography angiography in patients with diabetes without diabetic retinopathy. Invest Ophthalmol Vis Sci. 2017;58(1):190–6. https://doi.org/10.1167/iovs.16-20531. In this OCT-A analysis of parafoveal vascular parameters, superficial and deep retinal vessel density was decreased in patients with diabetes and no retinopathy compared with healthy subjects.
Takase N, Nozaki M, Kato A, Ozeki H, Yoshida M, Ogura Y. Enlargement of foveal avascular zone in diabetic eyes evaluated by en face optical coherence tomography angiography. Retina. 2015;35(11):2377–83. https://doi.org/10.1097/IAE.0000000000000849.
Scarinci F, Nesper PL, Fawzi AA. Deep retinal capillary nonperfusion is associated with photoreceptor disruption in diabetic macular ischemia. Am J Ophthalmol. 2016;168:129–38. https://doi.org/10.1016/j.ajo.2016.05.002.
Hwang TS, Zhang M, Bhavsar K, Zhang X, Campbell JP, Lin P, et al. Visualization of 3 distinct retinal plexuses by projection-resolved optical coherence tomography angiography in diabetic retinopathy. JAMA Ophthalmol. 2016;134(12):1411–9. https://doi.org/10.1001/jamaophthalmol.2016.4272.
Baxter SL, Ashir A, Nguyen BJ, Nudleman E. Quantification of retinal nonperfusion associated with posterior segment neovascularization in diabetic retinopathy using ultra-widefield fluorescein angiography. Ophthalmic Surg Lasers Imaging Retina. 2019;50(2):86–92. https://doi.org/10.3928/23258160-20190129-04.
Lorenzi M. The polyol pathway as a mechanism for diabetic retinopathy: attractive, elusive, and resilient. Exp Diabetes Res. 2007;2007:61038–10. https://doi.org/10.1155/2007/61038.
Gugliucci A. Formation of fructose-mediated advanced glycation end products and their roles in metabolic and inflammatory diseases. Adv Nutr. 2017;8(1):54–62. https://doi.org/10.3945/an.116.013912.
Zong H, Ward M, Stitt AW. AGEs, RAGE, and diabetic retinopathy. Curr Diabetes Rep. 2011;11(4):244–52. https://doi.org/10.1007/s11892-011-0198-7.
Sun JK, Keenan HA, Cavallerano JD, Asztalos BF, Schaefer EJ, Sell DR, et al. Protection from retinopathy and other complications in patients with type 1 diabetes of extreme duration: the Joslin 50-year medalist study. Diabetes Care. 2011;34(4):968–74. https://doi.org/10.2337/dc10-1675.
Geraldes P, King GL. Activation of protein kinase C isoforms and its impact on diabetic complications. Circ Res. 2010;106(8):1319–31. https://doi.org/10.1161/CIRCRESAHA.110.217117.
Ayloo S, Gu C. Transcytosis at the blood-brain barrier. Curr Opin Neurobiol. 2019;57:32–8. https://doi.org/10.1016/j.conb.2018.12.014.
Diaz-Coranguez M, Ramos C, Antonetti DA. The inner blood-retinal barrier: cellular basis and development. Vis Res. 2017;139:123–37. https://doi.org/10.1016/j.visres.2017.05.009.
Miloudi K, Oubaha M, Menard C, Dejda A, Guber V, Cagnone G, et al. NOTCH1 signaling induces pathological vascular permeability in diabetic retinopathy. Proc Natl Acad Sci U S A. 2019;116:4538–47. https://doi.org/10.1073/pnas.1814711116.
Stewart PA, Tuor UI. Blood-eye barriers in the rat: correlation of ultrastructure with function. J Comp Neurol. 1994;340(4):566–76. https://doi.org/10.1002/cne.903400409.
Daneman R, Zhou L, Kebede AA, Barres BA. Pericytes are required for blood-brain barrier integrity during embryogenesis. Nature. 2010;468(7323):562–6. https://doi.org/10.1038/nature09513.
Enge M, Bjarnegard M, Gerhardt H, Gustafsson E, Kalen M, Asker N, et al. Endothelium-specific platelet-derived growth factor-B ablation mimics diabetic retinopathy. EMBO J. 2002;21(16):4307–16.
Tikhonenko M, Lydic TA, Wang Y, Chen W, Opreanu M, Sochacki A, et al. Remodeling of retinal fatty acids in an animal model of diabetes: a decrease in long-chain polyunsaturated fatty acids is associated with a decrease in fatty acid elongases Elovl2 and Elovl4. Diabetes. 2010;59(1):219–27. https://doi.org/10.2337/db09-0728.
Sapieha P, Chen J, Stahl A, Seaward MR, Favazza TL, Juan AM, et al. Omega-3 polyunsaturated fatty acids preserve retinal function in type 2 diabetic mice. Nutr Diabetes. 2012;2:e36. https://doi.org/10.1038/nutd.2012.10.
• Kady NM, Liu X, Lydic TA, Syed MH, Navitskaya S, Wang Q, et al. ELOVL4-mediated production of very long-chain ceramides stabilizes tight junctions and prevents diabetes-induced retinal vascular permeability. Diabetes. 2018;67(4):769–81. https://doi.org/10.2337/db17-1034. In a mouse model of DR, correction of diabetes-induced reduction of VLC-PUFA by AAV-mediated ELOVL4 overexpression restores ceramide-dependent BRB integrity.
Abcouwer SF, Lin CM, Wolpert EB, Shanmugam S, Schaefer EW, Freeman WM, et al. Effects of ischemic preconditioning and bevacizumab on apoptosis and vascular permeability following retinal ischemia-reperfusion injury. Invest Ophthalmol Vis Sci. 2010;51(11):5920–33. https://doi.org/10.1167/iovs.10-5264.
Muthusamy A, Lin CM, Shanmugam S, Lindner HM, Abcouwer SF, Antonetti DA. Ischemia-reperfusion injury induces occludin phosphorylation/ubiquitination and retinal vascular permeability in a VEGFR-2-dependent manner. J Cereb Blood Flow Metab. 2014;34(3):522–31. https://doi.org/10.1038/jcbfm.2013.230.
Nakahara T, Hoshino M, Hoshino S, Mori A, Sakamoto K, Ishii K. Structural and functional changes in retinal vasculature induced by retinal ischemia-reperfusion in rats. Exp Eye Res. 2015;135:134–45. https://doi.org/10.1016/j.exer.2015.02.020.
Puro DG. Diabetes-induced dysfunction of retinal Muller cells. Trans Am Ophthalmol Soc. 2002;100:339–52.
Metea MR, Newman EA. Glial cells dilate and constrict blood vessels: a mechanism of neurovascular coupling. J Neurosci. 2006;26(11):2862–70. https://doi.org/10.1523/JNEUROSCI.4048-05.2006.
Shen W, Fruttiger M, Zhu L, Chung SH, Barnett NL, Kirk JK, et al. Conditional Muller cell ablation causes independent neuronal and vascular pathologies in a novel transgenic model. J Neurosci. 2012;32(45):15715–27. https://doi.org/10.1523/JNEUROSCI.2841-12.2012.
Harada T, Harada C, Watanabe M, Inoue Y, Sakagawa T, Nakayama N, et al. Functions of the two glutamate transporters GLAST and GLT-1 in the retina. Proc Natl Acad Sci U S A. 1998;95(8):4663–6. https://doi.org/10.1073/pnas.95.8.4663.
Karwoski CJ, Lu HK, Newman EA. Spatial buffering of light-evoked potassium increases by retinal Muller (glial) cells. Science. 1989;244(4904):578–80.
Fine BS, Brucker AJ. Macular edema and cystoid macular edema. Am J Ophthalmol. 1981;92(4):466–81.
Mizutani M, Gerhardinger C, Lorenzi M. Muller cell changes in human diabetic retinopathy. Diabetes. 1998;47(3):445–9.
Bai Y, Ma JX, Guo J, Wang J, Zhu M, Chen Y, et al. Muller cell-derived VEGF is a significant contributor to retinal neovascularization. J Pathol. 2009;219(4):446–54. https://doi.org/10.1002/path.2611.
Feenstra DJ, Yego EC, Mohr S. Modes of retinal cell death in diabetic retinopathy. J Clin Exp Ophthalmol. 2013;4(5):298. https://doi.org/10.4172/2155-9570.1000298.
Newman EA. Functional hyperemia and mechanisms of neurovascular coupling in the retinal vasculature. J Cereb Blood Flow Metab. 2013;33(11):1685–95. https://doi.org/10.1038/jcbfm.2013.145.
Lasta M, Pemp B, Schmidl D, Boltz A, Kaya S, Palkovits S, et al. Neurovascular dysfunction precedes neural dysfunction in the retina of patients with type 1 diabetes. Invest Ophthalmol Vis Sci. 2013;54(1):842–7. https://doi.org/10.1167/iovs.12-10873.
Lott ME, Slocomb JE, Shivkumar V, Smith B, Quillen D, Gabbay RA, et al. Impaired retinal vasodilator responses in prediabetes and type 2 diabetes. Acta Ophthalmol. 2013;91(6):e462–9. https://doi.org/10.1111/aos.12129.
Mishra A, Newman EA. Inhibition of inducible nitric oxide synthase reverses the loss of functional hyperemia in diabetic retinopathy. Glia. 2010;58(16):1996–2004. https://doi.org/10.1002/glia.21068.
Mishra A, Newman EA. Aminoguanidine reverses the loss of functional hyperemia in a rat model of diabetic retinopathy. Front Neuroenerg. 2011;3:10. https://doi.org/10.3389/fnene.2011.00010.
Bresnick GH, Korth K, Groo A, Palta M. Electroretinographic oscillatory potentials predict progression of diabetic retinopathy. Preliminary report. Arch Ophthalmol. 1984;102(9):1307–11.
Bresnick GH, Palta M. Oscillatory potential amplitudes. Relation to severity of diabetic retinopathy. Arch Ophthalmol. 1987;105(7):929–33.
Bresnick GH, Palta M. Temporal aspects of the electroretinogram in diabetic retinopathy. Arch Ophthalmol. 1987;105(5):660–4.
Harrison WW, Bearse MA Jr, Ng JS, Jewell NP, Barez S, Burger D, et al. Multifocal electroretinograms predict onset of diabetic retinopathy in adult patients with diabetes. Invest Ophthalmol Vis Sci. 2011;52(2):772–7. https://doi.org/10.1167/iovs.10-5931.
Holopigian K, Seiple W, Lorenzo M, Carr R. A comparison of photopic and scotopic electroretinographic changes in early diabetic retinopathy. Invest Ophthalmol Vis Sci. 1992;33(10):2773–80.
Palmowski AM, Sutter EE, Bearse MA Jr, Fung W. Mapping of retinal function in diabetic retinopathy using the multifocal electroretinogram. Invest Ophthalmol Vis Sci. 1997;38(12):2586–96.
Aung MH, Kim MK, Olson DE, Thule PM, Pardue MT. Early visual deficits in streptozotocin-induced diabetic Long Evans rats. Invest Ophthalmol Vis Sci. 2013;54(2):1370–7. https://doi.org/10.1167/iovs.12-10927.
Rajagopal R, Bligard GW, Zhang S, Yin L, Lukasiewicz P, Semenkovich CF. Functional deficits precede structural lesions in mice with high-fat diet-induced diabetic retinopathy. Diabetes. 2016;65(4):1072–84. https://doi.org/10.2337/db15-1255.
Bresnick GH, Palta M. Predicting progression to severe proliferative diabetic retinopathy. Arch Ophthalmol. 1987;105(6):810–4.
Bearse MA Jr, Adams AJ, Han Y, Schneck ME, Ng J, Bronson-Castain K, et al. A multifocal electroretinogram model predicting the development of diabetic retinopathy. Prog Retin Eye Res. 2006;25(5):425–48. https://doi.org/10.1016/j.preteyeres.2006.07.001.
Jackson GR, Scott IU, Quillen DA, Walter LE, Gardner TW. Inner retinal visual dysfunction is a sensitive marker of non-proliferative diabetic retinopathy. Br J Ophthalmol. 2012;96(5):699–703. https://doi.org/10.1136/bjophthalmol-2011-300467.
Muntoni S, Serra A, Mascia C, Songini M. Dyschromatopsia in diabetes mellitus and its relation to metabolic control. Diabetes Care. 1982;5(4):375–8. https://doi.org/10.2337/diacare.5.4.375.
Sokol S, Moskowitz A, Skarf B, Evans R, Molitch M, Senior B. Contrast sensitivity in diabetics with and without background retinopathy. Arch Ophthalmol. 1985;103(1):51–4.
Henson DB, North RV. Dark adaptation in diabetes mellitus. Br J Ophthalmol. 1979;63(8):539–41. https://doi.org/10.1136/bjo.63.8.539.
Jain M, Devan S, Jaisankar D, Swaminathan G, Pardhan S, Raman R. Pupillary abnormalities with varying severity of diabetic retinopathy. Sci Rep. 2018;8(1):5636. https://doi.org/10.1038/s41598-018-24015-9.
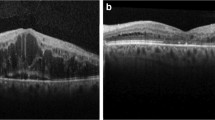
•• Sohn EH, van Dijk HW, Jiao C, Kok PH, Jeong W, Demirkaya N, et al. Retinal neurodegeneration may precede microvascular changes characteristic of diabetic retinopathy in diabetes mellitus. Proc Natl Acad Sci U S A. 2016;113(19):E2655–64. https://doi.org/10.1073/pnas.1522014113. In patients without visible DR, inner retinal thinning is detectable by high-resolution OCT analysis. These changes were progressive and independent of glycemic control.
Abramoff MD, Fort PE, Han IC, Jayasundera KT, Sohn EH, Gardner TW. Approach for a clinically useful comprehensive classification of vascular and neural aspects of diabetic retinal disease. Invest Ophthalmol Vis Sci. 2018;59(1):519–27. https://doi.org/10.1167/iovs.17-21873.
Lynch SK, Abramoff MD. Diabetic retinopathy is a neurodegenerative disorder. Vis Res. 2017;139:101–7. https://doi.org/10.1016/j.visres.2017.03.003.
van Dijk HW, Verbraak FD, Kok PH, Stehouwer M, Garvin MK, Sonka M, et al. Early neurodegeneration in the retina of type 2 diabetic patients. Invest Ophthalmol Vis Sci. 2012;53(6):2715–9. https://doi.org/10.1167/iovs.11-8997.
Antonetti DA, Klein R, Gardner TW. Diabetic retinopathy. N Engl J Med. 2012;366(13):1227–39. https://doi.org/10.1056/NEJMra1005073.
Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Edwards AR, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(6):1064–77.e35. https://doi.org/10.1016/j.ophtha.2010.02.031.
Elman MJ, Qin H, Aiello LP, Beck RW, Bressler NM, Ferris FL 3rd, et al. Intravitreal ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: three-year randomized trial results. Ophthalmology. 2012;119(11):2312–8. https://doi.org/10.1016/j.ophtha.2012.08.022.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789–801. https://doi.org/10.1016/j.ophtha.2011.12.039
The Diabetic Retinopathy Clinical Research N. Aflibercept. Bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372:1193–203. https://doi.org/10.1056/NEJMoa1414264.
Kern TS, Engerman RL. Capillary lesions develop in retina rather than cerebral cortex in diabetes and experimental galactosemia. Arch Ophthalmol. 1996;114(3):306–10.
Cogan DG, Toussaint D, Kuwabara T. Retinal vascular patterns. IV Diabetic retinopathy. Arch Ophthalmol. 1961;66:366–78.
•• Joyal JS, Sun Y, Gantner ML, Shao Z, Evans LP, Saba N, et al. Retinal lipid and glucose metabolism dictates angiogenesis through the lipid sensor Ffar1. Nat Med. 2016;22(4):439–45. https://doi.org/10.1038/nm.4059. This paper provides evidence that photoreceptors oxidize fatty acids to generate ATP, in addition to using the more traditional substrate, glucose. Moreover, disruption of a key lipid sensor necessary for fatty acid uptake into photoreceptors causes abnormal retinal vascularization, suggesting this metabolic pathway could be relevant to neovascular diseases of the retina.
Kooragayala K, Gotoh N, Cogliati T, Nellissery J, Kaden TR, French S, et al. Quantification of oxygen consumption in retina ex vivo demonstrates limited reserve capacity of photoreceptor mitochondria. Invest Ophthalmol Vis Sci. 2015;56(13):8428–36. https://doi.org/10.1167/iovs.15-17901.
Wong-Riley MT. Energy metabolism of the visual system. Eye Brain. 2010;2:99–116. https://doi.org/10.2147/EB.S9078.
Reiter CE, Gardner TW. Functions of insulin and insulin receptor signaling in retina: possible implications for diabetic retinopathy. Prog Retin Eye Res. 2003;22(4):545–62.
Reiter CE, Wu X, Sandirasegarane L, Nakamura M, Gilbert KA, Singh RS, et al. Diabetes reduces basal retinal insulin receptor signaling: reversal with systemic and local insulin. Diabetes. 2006;55(4):1148–56.
Arden GB. The absence of diabetic retinopathy in patients with retinitis pigmentosa: implications for pathophysiology and possible treatment. Br J Ophthalmol. 2001;85(3):366–70.
de Gooyer TE, Stevenson KA, Humphries P, Simpson DA, Gardiner TA, Stitt AW. Retinopathy is reduced during experimental diabetes in a mouse model of outer retinal degeneration. Invest Ophthalmol Vis Sci. 2006;47(12):5561–8. https://doi.org/10.1167/iovs.06-0647.
Sternberg P Jr, Landers MB 3rd, Wolbarsht M. The negative coincidence of retinitis pigmentosa and proliferative diabetic retinopathy. Am J Ophthalmol. 1984;97(6):788–9.
Berkowitz BA, Kern TS, Bissig D, Patel P, Bhatia A, Kefalov VJ, et al. Systemic retinaldehyde treatment corrects retinal oxidative stress, rod dysfunction, and impaired visual performance in diabetic mice. Invest Ophthalmol Vis Sci. 2015;56(11):6294–303. https://doi.org/10.1167/iovs.15-16990.
• Bavinger JC, Dunbar GE, Stem MS, Blachley TS, Kwark L, Farsiu S, et al. The effects of diabetic retinopathy and pan-retinal photocoagulation on photoreceptor cell function as assessed by dark adaptometry. Invest Ophthalmol Vis Sci. 2016;57(1):208–17. https://doi.org/10.1167/iovs.15-17281. Clinical dark adaptometry demonstrated significant phtoreceptor and/or retinal pigment epithelial dysfunction in patients with DR, with abnormalities in dark adaption correlating to severity of disease.
Arden GB, Sidman RL, Arap W, Schlingemann RO. Spare the rod and spoil the eye. Br J Ophthalmol. 2005;89(6):764–9. https://doi.org/10.1136/bjo.2004.062547.
•• Gross JG, Glassman AR, Liu D, Sun JK, Antoszyk AN, Baker CW, et al. Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2018;136(10):1138–48. https://doi.org/10.1001/jamaophthalmol.2018.3255. In this report of five-year outcomes in a pivotal trial conducted by the Diabetic Retinopathy Clinical Research Network, therapy with intravitreous ranibizumab was comparable with panretinal phocoagulation in the management of PDR.
•• Sivaprasad S, Prevost AT, Vasconcelos JC, Riddell A, Murphy C, Kelly J, et al. Clinical efficacy of intravitreal aflibercept versus panretinal photocoagulation for best corrected visual acuity in patients with proliferative diabetic retinopathy at 52 weeks (CLARITY): a multicentre, single-blinded, randomised, controlled, phase 2b, non-inferiority trial. Lancet. 2017;389(10085):2193–203. https://doi.org/10.1016/S0140-6736(17)31193-5. This landmark study demonstrated that intraviteous aflibercept was comparable with panretinal photocoagulation in the management of PDR.
Scott IU, Jackson GR, Quillen DA, Larsen M, Klein R, Liao J, et al. Effect of doxycycline vs placebo on retinal function and diabetic retinopathy progression in patients with severe nonproliferative or non-high-risk proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2014;132(5):535–43. https://doi.org/10.1001/jamaophthalmol.2014.93.
Stahel M, Becker M, Graf N, Michels S. Systemic interleukin 1beta inhibition in proliferative diabetic retinopathy: a prospective open-label study using canakinumab. Retina. 2016;36(2):385–91. https://doi.org/10.1097/IAE.0000000000000701.
Group P-D, Aiello LP, Davis MD, Girach A, Kles KA, Milton RC, et al. Effect of ruboxistaurin on visual loss in patients with diabetic retinopathy. Ophthalmology. 2006;113(12):2221–30. https://doi.org/10.1016/j.ophtha.2006.07.032.
• Simo R, Hernandez C, Porta M, Bandello F, Grauslund J, Harding SP, et al. Effects of topically administered neuroprotective drugs in early stages of diabetic retinopathy: results of the EUROCONDOR Clinical Trial. Diabetes. 2019;68(2):457–63. https://doi.org/10.2337/db18-0682. Topical therapy with brimonidine and somatostatin, two compounds with potential neuroprotective effects, was associated with decreased progression of neuroretinopathy endpoints in patients with diabetes.
Li F, Zhang L, Wang Y, Xu W, Jiao W, Ma A, et al. One-year outcome of conbercept therapy for diabetic macular edema. Curr Eye Res. 2018;43(2):218–23. https://doi.org/10.1080/02713683.2017.1379542.
Xu Y, Rong A, Xu W, Niu Y, Wang Z. Comparison of 12-month therapeutic effect of conbercept and ranibizumab for diabetic macular edema: a real-life clinical practice study. BMC Ophthalmol. 2017;17(1):158. https://doi.org/10.1186/s12886-017-0554-8.
Krishnadev N, Forooghian F, Cukras C, Wong W, Saligan L, Chew EY, et al. Subconjunctival sirolimus in the treatment of diabetic macular edema. Graefe’s Arch Clin Exp Ophthalmol = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2011;249(11):1627–33. https://doi.org/10.1007/s00417-011-1694-9.
• Sivaprasad S, Vasconcelos JC, Prevost AT, Holmes H, Hykin P, George S, et al. Clinical efficacy and safety of a light mask for prevention of dark adaptation in treating and preventing progression of early diabetic macular oedema at 24 months (CLEOPATRA): a multicentre, phase 3, randomised controlled trial. Lancet Diabetes Endocrinol. 2018;6(5):382–91. https://doi.org/10.1016/S2213-8587(18)30036-6. This innovative phase 3 trial, light masks worn at night time were used to treat DME by reducing metabolic demands of photoreceptors in patients with diabetes. However, this therapy did not confer signficant benefits.
Sjolie AK, Klein R, Porta M, Orchard T, Fuller J, Parving HH, et al. Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): a randomised placebo-controlled trial. Lancet. 2008;372(9647):1385–93. https://doi.org/10.1016/S0140-6736(08)61411-7.
Nguyen QD, Schachar RA, Nduaka CI, Sperling M, Basile AS, Klamerus KJ, et al. Dose-ranging evaluation of intravitreal siRNA PF-04523655 for diabetic macular edema (the DEGAS study). Invest Ophthalmol Vis Sci. 2012;53(12):7666–74. https://doi.org/10.1167/iovs.12-9961.
Staurenghi G, Ye L, Magee MH, Danis RP, Wurzelmann J, Adamson P, et al. Darapladib, a lipoprotein-associated phospholipase A2 inhibitor, in diabetic macular edema: a 3-month placebo-controlled study. Ophthalmology. 2015;122(5):990–6. https://doi.org/10.1016/j.ophtha.2014.12.014.
de Andrade GC, de Oliveira Dias JR, Maia A, Farah ME, Meyer CH, Rodrigues EB. Intravitreal ziv-aflibercept for diabetic macular edema: 48-week outcomes. Ophthalmic Surg Lasers Imaging Retina. 2018;49(4):245–50. https://doi.org/10.3928/23258160-20180329-06.
The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. https://doi.org/10.1056/nejm199309303291401.
Stratton IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, Manley SE, et al. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia. 2001;44(2):156–63. https://doi.org/10.1007/s001250051594.
Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. 2000;342(6):381–9. https://doi.org/10.1056/nejm200002103420603.
Early worsening of diabetic retinopathy in the Diabetes Control and Complications Trial. Arch Ophthalmol. 1998;116(7):874–86.
Feldman-Billard S, Larger E, Massin P. Standards for screening and surveillance of ocular complications in people with diabetes SFDsg. Early worsening of diabetic retinopathy after rapid improvement of blood glucose control in patients with diabetes. Diabetes Metab. 2018;44(1):4–14. https://doi.org/10.1016/j.diabet.2017.10.014.
• Hernandez C, Bogdanov P, Corraliza L, Garcia-Ramirez M, Sola-Adell C, Arranz JA, et al. Topical administration of GLP-1 receptor agonists prevents retinal neurodegeneration in experimental diabetes. Diabetes. 2016;65(1):172–87. https://doi.org/10.2337/db15-0443. Topical or systemic administration of GLP-1RAs prevented diabetes-associated neurodegeneration and gliosis in this preclinical study performed in a mouse model of T2DM.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44. https://doi.org/10.1056/NEJMoa1607141.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22. https://doi.org/10.1056/NEJMoa1603827.
Obrosova IG, Minchenko AG, Vasupuram R, White L, Abatan OI, Kumagai AK, et al. Aldose reductase inhibitor fidarestat prevents retinal oxidative stress and vascular endothelial growth factor overexpression in streptozotocin-diabetic rats. Diabetes. 2003;52(3):864–71.
A randomized trial of sorbinil, an aldose reductase inhibitor, in diabetic retinopathy. Sorbinil Retinopathy Trial Research Group. Arch Ophthalmol. 1990;108(9):1234–44.
Sun W, Oates PJ, Coutcher JB, Gerhardinger C, Lorenzi M. A selective aldose reductase inhibitor of a new structural class prevents or reverses early retinal abnormalities in experimental diabetic retinopathy. Diabetes. 2006;55(10):2757–62. https://doi.org/10.2337/db06-0138.
Gardner TW, Antonetti DA. Ruboxistaurin for diabetic retinopathy. Ophthalmology. 2006;113(12):2135–6. https://doi.org/10.1016/j.ophtha.2006.09.003.
Chew EY, Ambrosius WT, Davis MD, Danis RP, Gangaputra S, Greven CM, et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med. 2010;363(3):233–44. https://doi.org/10.1056/NEJMoa1001288.
Patel V, Rassam S, Newsom R, Wiek J, Kohner E. Retinal blood flow in diabetic retinopathy. BMJ. 1992;305(6855):678–83.
Behl T, Kotwani A. Potential of angiotensin II receptor blockers in the treatment of diabetic retinopathy. Life Sci. 2017;176:1–9. https://doi.org/10.1016/j.lfs.2017.03.020.
Wang B, Wang F, Zhang Y, Zhao SH, Zhao WJ, Yan SL, et al. Effects of RAS inhibitors on diabetic retinopathy: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(4):263–74. https://doi.org/10.1016/s2213-8587(14)70256-6.
Chew EY, Klein ML, Ferris FL 3rd, Remaley NA, Murphy RP, Chantry K, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch Ophthalmol. 1996;114(9):1079–84.
• Srinivasan S, Raman R, Kulothungan V, Swaminathan G, Sharma T. Influence of serum lipids on the incidence and progression of diabetic retinopathy and macular oedema: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetics Study-II. Clin Exp Ophthalmol. 2017;45(9):894–900. https://doi.org/10.1111/ceo.12990. This observational study performed in South Asian volunteers with T2DM, serum cholesterol and triglyceride abnormalities were strongly correlated to DR progression and DME.
• Itoh H, Komuro I, Takeuchi M, Akasaka T, Daida H, Egashira Y, et al. Intensive treat-to-target statin therapy in high-risk Japanese patients with hypercholesterolemia and diabetic retinopathy: report of a randomized study. Diabetes Care. 2018;41(6):1275–84. https://doi.org/10.2337/dc17-2224. In this large, multicenter, randomized clinical trial, high-dose statin therapy to intensively decrease LDL-C levels was associated with a significant reduction in retinopathy endpoints.
Kang EY, Chen TH, Garg SJ, Sun CC, Kang JH, Wu WC, et al. Association of statin therapy with prevention of vision-threatening diabetic retinopathy. JAMA Ophthalmol. 2019;137:363. https://doi.org/10.1001/jamaophthalmol.2018.6399.
Keech AC, Mitchell P, Summanen PA, O’Day J, Davis TM, Moffitt MS, et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet. 2007;370(9600):1687–97. https://doi.org/10.1016/s0140-6736(07)61607-9.
Chen Y, Hu Y, Lin M, Jenkins AJ, Keech AC, Mott R, et al. Therapeutic effects of PPARα agonists on diabetic retinopathy in type 1 diabetes models. Diabetes. 2013;62(1):261–72. https://doi.org/10.2337/db11-0413.
•• Hu J, Dziumbla S, Lin J, Bibli SI, Zukunft S, de Mos J, et al. Inhibition of soluble epoxide hydrolase prevents diabetic retinopathy. Nature. 2017;552(7684):248–52. https://doi.org/10.1038/nature25013. Here, soluble epoxide hydrolase was identified as a pro-permeability factor in diabetic mouse models, operating by promoting DHA breakdown. Inhibition of this enzyme improved retinal barrier function, whereas its overexpression in Muller cells exacerbated retinal leakage.
•• Sala-Vila A, Diaz-Lopez A, Valls-Pedret C, Cofan M, Garcia-Layana A, Lamuela-Raventos RM, et al. Dietary marine omega-3 fatty acids and incident sight-threatening retinopathy in middle-aged and older individuals with type 2 diabetes: prospective investigation from the PREDIMED Trial. JAMA Ophthalmol. 2016;134(10):1142–9. https://doi.org/10.1001/jamaophthalmol.2016.2906. In this randomized trial among patients with T2DM, dietary supplementation with 500 mg/day of long chain PUFA was associated with a 48% relative reduction in risk of sight-threatening DR after a median follow-up of 6 years.
Tikhonenko M, Lydic TA, Opreanu M, Li Calzi S, Bozack S, McSorley KM, et al. N-3 polyunsaturated fatty acids prevent diabetic retinopathy by inhibition of retinal vascular damage and enhanced endothelial progenitor cell reparative function. PLoS One. 2013;8(1):e55177. https://doi.org/10.1371/journal.pone.0055177.
Group ETDRSR. Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Ophthalmology. 1991;98(5):766–85.
Group DRSR. Photocoagulation treatment of proliferative diabetic retinopathy: clinical application of diabetic retinopathy study (DRS) findings, DRS report number 8. Ophthalmology. 1981;88(7):583–600.
• Maturi RK, Glassman AR, Liu D, Beck RW, Bhavsar AR, Bressler NM, et al. Effect of adding dexamethasone to continued ranibizumab treatment in patients with persistent diabetic macular edema: a DRCR network phase 2 randomized clinical trial. JAMA Ophthalmol. 2018;136(1):29–38. https://doi.org/10.1001/jamaophthalmol.2017.4914. Addition of a long-acting dexamethsone implant (0.7mg) to a regimen of ranibizumab injections was associated with superior anatomic outcomes compared with ranibizumab monotherapy in this 24-month analysis among patients with chronic DME. Patients who were pseudophakic at baseline demonstrated superior visual acuity outcomes in the combination therapy group.
Boyer DS, Yoon YH, Belfort R Jr, Bandello F, Maturi RK, Augustin AJ, et al. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014;121(10):1904–14. https://doi.org/10.1016/j.ophtha.2014.04.024.
Campochiaro PA, Brown DM, Pearson A, Ciulla T, Boyer D, Holz FG, et al. Long-term benefit of sustained-delivery fluocinolone acetonide vitreous inserts for diabetic macular edema. Ophthalmology. 2011;118(4):626–35.e2. https://doi.org/10.1016/j.ophtha.2010.12.028.
Fraser-Bell S, Lim LL, Campain A, Mehta H, Aroney C, Bryant J, et al. Bevacizumab or dexamethasone implants for DME: 2-year results (the BEVORDEX study). Ophthalmology. 2016;123(6):1399–401. https://doi.org/10.1016/j.ophtha.2015.12.012.
Cunha-Vaz J, Ashton P, Iezzi R, Campochiaro P, Dugel PU, Holz FG, et al. Sustained delivery fluocinolone acetonide vitreous implants: long-term benefit in patients with chronic diabetic macular edema. Ophthalmology. 2014;121(10):1892–903. https://doi.org/10.1016/j.ophtha.2014.04.019.
Brown DM, Schmidt-Erfurth U, Do DV, Holz FG, Boyer DS, Midena E, et al. Intravitreal aflibercept for diabetic macular edema: 100-week results from the VISTA and VIVID studies. Ophthalmology. 2015;122(10):2044–52. https://doi.org/10.1016/j.ophtha.2015.06.017.
Wang W, Lo ACY. Diabetic retinopathy: pathophysiology and treatments. Int J Mol Sci. 2018;19(6). https://doi.org/10.3390/ijms19061816.
Gross JG, Glassman AR, Jampol LM, Inusah S, Aiello LP, Antoszyk AN, et al. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA. 2015;314(20):2137–46. https://doi.org/10.1001/jama.2015.15217.
Semenza GL. HIF-1 and human disease: one highly involved factor. Genes Dev. 2000;14(16):1983–91.
Qaum T, Xu Q, Joussen AM, Clemens MW, Qin W, Miyamoto K, et al. VEGF-initiated blood–retinal barrier breakdown in early diabetes. Invest Ophthalmol Vis Sci. 2001;42(10):2408–13.
Apte RS, Chen DS, Ferrara N. VEGF in signaling and disease: beyond discovery and development. Cell. 2019;176(6):1248–64. https://doi.org/10.1016/j.cell.2019.01.021.
Semenza GL. Oxygen sensing, hypoxia-inducible factors, and disease pathophysiology. Annu Rev Pathol. 2014;9:47–71. https://doi.org/10.1146/annurev-pathol-012513-104720.
Wells JA, Glassman AR, Ayala AR, Jampol LM, Bressler NM, Bressler SB, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123(6):1351–9. https://doi.org/10.1016/j.ophtha.2016.02.022.
Kiss S, Dugel PU, Khanani AM, Broder MS, Chang E, Sun GH, et al. Endophthalmitis rates among patients receiving intravitreal anti-VEGF injections: a USA claims analysis. Clin Ophthalmol. 2018;12:1625–35. https://doi.org/10.2147/opth.S169143.
Patel S. Medicare spending on anti-vascular endothelial growth factor medications. Ophthalmol Retina. 2018;2(8):785–91. https://doi.org/10.1016/j.oret.2017.12.006.
Dugel PU, Jaffe GJ, Sallstig P, Warburton J, Weichselberger A, Wieland M, et al. Brolucizumab versus aflibercept in participants with neovascular age-related macular degeneration: a randomized trial. Ophthalmology. 2017;124(9):1296–304. https://doi.org/10.1016/j.ophtha.2017.03.057.
Dugel PU, Koh A, Ogura Y, Jaffe G, Schmidt-Erfurth U, Brown D, et al. HAWK and HARRIER: phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2019. https://doi.org/10.1016/j.ophtha.2019.04.017.
Milam KE, Parikh SM. The angiopoietin-Tie2 signaling axis in the vascular leakage of systemic inflammation. Tissue Barriers. 2015;3(1–2):e957508. https://doi.org/10.4161/21688362.2014.957508.
Shen J, Frye M, Lee BL, Reinardy JL, McClung JM, Ding K, et al. Targeting VE-PTP activates TIE2 and stabilizes the ocular vasculature. J Clin Invest. 2014;124(10):4564–76. https://doi.org/10.1172/jci74527.
Sahni J, Patel SS, Dugel PU, Khanani AM, Jhaveri CD, Wykoff CC, et al. Simultaneous inhibition of angiopoietin-2 and vascular endothelial growth factor-a with faricimab in diabetic macular edema: BOULEVARD phase 2 randomized trial. Ophthalmology. 2019. https://doi.org/10.1016/j.ophtha.2019.03.023.
Buehler A, Sitaras N, Favret S, Bucher F, Berger S, Pielen A, et al. Semaphorin 3F forms an anti-angiogenic barrier in outer retina. FEBS Lett. 2013;587(11):1650–5. https://doi.org/10.1016/j.febslet.2013.04.008.
Segarra M, Ohnuki H, Maric D, Salvucci O, Hou X, Kumar A, et al. Semaphorin 6A regulates angiogenesis by modulating VEGF signaling. Blood. 2012;120(19):4104–15. https://doi.org/10.1182/blood-2012-02-410076.
Cerani A, Tetreault N, Menard C, Lapalme E, Patel C, Sitaras N, et al. Neuron-derived semaphorin 3A is an early inducer of vascular permeability in diabetic retinopathy via neuropilin-1. Cell Metab. 2013;18(4):505–18. https://doi.org/10.1016/j.cmet.2013.09.003.
Thomas J, Liu F, Link DC. Mechanisms of mobilization of hematopoietic progenitors with granulocyte colony-stimulating factor. Curr Opin Hematol. 2002;9(3):183–9.
• Chakravarthy H, Navitskaya S, O’Reilly S, Gallimore J, Mize H, Beli E, et al. Role of acid sphingomyelinase in shifting the balance between proinflammatory and reparative bone marrow cells in diabetic retinopathy. Stem Cells. 2016;34(4):972–83. https://doi.org/10.1002/stem.2259. Acid sphingomyelinase was identified in this study as a key factor promoting aberrant vascular repair by bone marrow-derived hematopoietic stem cells in the diabetic milieu secondary to an upregulation of membrane ceramides. Inhibition of this enzyme corrected these defects in circulating stem cells and prevented pathology associated with DR in a mouse model.
Park SS, Moisseiev E, Bauer G, Anderson JD, Grant MB, Zam A, et al. Advances in bone marrow stem cell therapy for retinal dysfunction. Prog Retin Eye Res. 2017;56:148–65. https://doi.org/10.1016/j.preteyeres.2016.10.002.
Arden GB, Jyothi S, Hogg CH, Lee YF, Sivaprasad S. Regression of early diabetic macular oedema is associated with prevention of dark adaptation. Eye. 2011;25(12):1546–54. https://doi.org/10.1038/eye.2011.264.
Arden GB, Gunduz MK, Kurtenbach A, Volker M, Zrenner E, Gunduz SB, et al. A preliminary trial to determine whether prevention of dark adaptation affects the course of early diabetic retinopathy. Eye. 2010;24(7):1149–55. https://doi.org/10.1038/eye.2009.328.
Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54(6):1615–25.
Alam NM, Mills WC, Wong AA, Douglas RM, Szeto HH, Prusky GT. A mitochondrial therapeutic reverses visual decline in mouse models of diabetes. Dis Model Mech. 2015;8(7):701–10. https://doi.org/10.1242/dmm.020248.
Aung MH, Park HN, Han MK, Obertone TS, Abey J, Aseem F, et al. Dopamine deficiency contributes to early visual dysfunction in a rodent model of type 1 diabetes. J Neurosci. 2014;34(3):726–36. https://doi.org/10.1523/JNEUROSCI.3483-13.2014.
Gastinger MJ, Singh RS, Barber AJ. Loss of cholinergic and dopaminergic amacrine cells in streptozotocin-diabetic rat and Ins2Akita-diabetic mouse retinas. Invest Ophthalmol Vis Sci. 2006;47(7):3143–50. https://doi.org/10.1167/iovs.05-1376.
Pardue MT, Allen RS. Neuroprotective strategies for retinal disease. Prog Retin Eye Res. 2018;65:50–76. https://doi.org/10.1016/j.preteyeres.2018.02.002.
Funding
Eric Nudleman reports grants from the National Eye Institute (5K08EY028999-02). Rithwick Rajagopal reports grants from the National Eye Institute (K08EY025269) and grants from the Research to Prevent Blindness (Career Development Award).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Avinash Honasoge, Eric Nudleman, Morton Smith, and Rithwick Rajagopal declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Microvascular Complications—Retinopathy
Rights and permissions
About this article
Cite this article
Honasoge, A., Nudleman, E., Smith, M. et al. Emerging Insights and Interventions for Diabetic Retinopathy. Curr Diab Rep 19, 100 (2019). https://doi.org/10.1007/s11892-019-1218-2
Published:
DOI: https://doi.org/10.1007/s11892-019-1218-2