Abstract
Purpose
The aim of this study is to investigate changes in physical activity (PA) and sedentary time (ST) over 12 months following bariatric surgery.
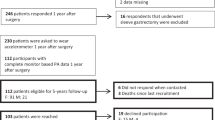
Methods
Pre-surgery and at 3, 6, 9, and 12 months post-surgery, wearable devices were used to measure PA at different intensities, grouped according to energy expenditure and daily step count, and ST. Measures were also collected of weight and self-efficacy for exercise. Pre- and 12 months post-surgery, measures were collected of body composition and cardiovascular fitness.
Results
Thirty adults scheduled for bariatric surgery were recruited (20 females, 44.1 [range, 22.0 to 65.0] years, body mass index 39.6 [range, 30.9 to 50.9] kg/m2). When compared to pre-surgery measures, over the 12 months post-surgery, there were no changes in the percentage of waking hours (mean [95% CI]) spent in ST (− 2% [− 6 to 3]), light intensity PA (1% [− 3 to 5]), and moderate-to-vigorous intensity PA (1% [− 1 to 3]). At all time points, participants spent most (> 70%) of their waking hours accumulating ST, with little time spent in light intensity PA (~ 21%) and almost no time in moderate-to-vigorous intensity PA (~ 5%). Step count and cardiovascular fitness were also unchanged. There were significant changes in weight, self-efficacy for exercise, and body composition.
Conclusions
Although bariatric surgery resulted in substantial weight loss and improved self-efficacy for exercise, it was insufficient to effect change in PA, ST or cardiovascular fitness. Complementing surgical intervention with behavioral interventions may optimize change in PA and ST.
Graphical abstract


Similar content being viewed by others
References
King WC, Belle SH, Eid GM, et al. Physical activity levels of patients undergoing bariatric surgery in the Longitudinal Assessment of Bariatric Surgery study. Surg Obes Relat Dis. 2008;4(6):721–8. https://doi.org/10.1016/j.soard.2008.08.022.
Bond DS, Unick JL, Jakicic JM, et al. Objective assessment of time spent being sedentary in bariatric surgery candidates. Obes Surg. 2011;21(6):811–4. https://doi.org/10.1007/s11695-010-0151-x.
Bond DS, Jakicic JM, Vithiananthan S, et al. Objective quantification of physical activity in bariatric surgery candidates and normal-weight controls. Surg Obes Relat Dis. 2010;6(1):72–8. https://doi.org/10.1016/j.soard.2009.08.012.
Unick JL, Bond DS, Jakicic JM, et al. Comparison of two objective monitors for assessing physical activity and sedentary behaviors in bariatric surgery patients. Obes Surg. 2012;22(3):347–52. https://doi.org/10.1007/s11695-011-0491-1.
Bond DS, Unick JL, Jakicic JM, et al. Physical activity and quality of life in severely obese individuals seeking bariatric surgery or lifestyle intervention. Health Qual Life Outcomes. 2012;10:86–90. https://doi.org/10.1186/1477-7525-10-86.
Langenberg S, Schulze M, Bartsch M, et al. Physical activity is unrelated to cognitive performance in pre-bariatric surgery patients. J Psychosom Res. 2015;79(2):165–70. https://doi.org/10.1016/j.jpsychores.2015.03.008.
Bond DS, Thomas JG. Measurement and intervention on physical activity and sedentary behaviours in bariatric surgery patients: emphasis on mobile technology. Eur Eat Disord Rev. 2015;23(6):470–8. https://doi.org/10.1002/erv.2394.
Ekkekakis P, Lind E, Vazou S. Affective responses to increasing levels of exercise intensity in normal-weight, overweight, and obese middle-aged women. Obesity (Silver Spring). 2010;18(1):79–85. https://doi.org/10.1038/oby.2009.204.
Bond DS, Jakicic JM, Unick JL, et al. Pre- to postoperative physical activity changes in bariatric surgery patients: self report vs. objective measures. Obesity (Silver Spring). 2010;18(12):2395–7. https://doi.org/10.1038/oby.2010.88.
King WC, Hsu JY, Belle SH, et al. Pre- to postoperative changes in physical activity: report from the Longitudinal Assessment of Bariatric Surgery-2 (LABS-2). Surg Obes Relat Dis. 2012;8(5):522–32. https://doi.org/10.1016/j.soard.2011.07.018.
King WC, Chen JY, Bond DS, et al. Objective assessment of changes in physical activity and sedentary behavior: pre- through 3 years post-bariatric surgery. Obesity (Silver Spring). 2015;23(6):1143–50. https://doi.org/10.1002/oby.21106.
Berglind D, Willmer M, Tynelius P, et al. Accelerometer-measured versus self-reported physical activity levels and sedentary behavior in women before and 9 months after Roux-en-Y gastric bypass. Obes Surg. 2016;26(7):1463–70. https://doi.org/10.1007/s11695-015-1971-5.
Afshar S, Seymour K, Kelly SB, et al. Changes in physical activity after bariatric surgery: using objective and self-reported measures. Surg Obes Relat Dis. 2017;13(3):474–83. https://doi.org/10.1016/j.soard.2016.09.012.
Crisp AH, Verlengia R, Ravelli MN, et al. Changes in Physical Activities and Body Composition after Roux-Y Gastric Bypass Surgery. Obes Surg. 2018;28(6):1665–71. https://doi.org/10.1007/s11695-017-3074-y.
Sellberg F, Possmark S, Willmer M, et al. Meeting physical activity recommendations is associated with health-related quality of life in women before and after Roux-en-Y gastric bypass surgery. Qual Life Res. 2019;28:1497–507. https://doi.org/10.1007/s11136-019-02120-0.
Herman KM, Carver TE, Christou NV, et al. Keeping the weight off: physical activity, sitting time, and weight loss maintenance in bariatric surgery patients 2 to 16 years postsurgery. Obes Surg. 2014;24(7):1064–72. https://doi.org/10.1007/s11695-014-1212-3.
Amundsen T, Strommen M, Martins C. Suboptimal weight loss and weight regain after gastric bypass surgery-postoperative status of energy intake, eating behavior, physical activity, and psychometrics. Obes Surg. 2017;27(5):1316–23. https://doi.org/10.1007/s11695-016-2475-7.
Ruiz-Tovar J, Zubiaga L, Llavero C, et al. Serum cholesterol by morbidly obese patients after laparoscopic sleeve gastrectomy and additional physical activity. Obes Surg. 2014;24(3):385–9. https://doi.org/10.1007/s11695-013-1082-0.
Vatier C, Henegar C, Ciangura C, et al. Dynamic relations between sedentary behavior, physical activity, and body composition after bariatric surgery. Obes Surg. 2012;22(8):1251–6. https://doi.org/10.1007/s11695-012-0619-y.
Josbeno DA, Jakicic JM, Hergenroeder A, et al. Physical activity and physical function changes in obese individuals after gastric bypass surgery. Surg Obes Relat Dis. 2010;6(4):361–6. https://doi.org/10.1016/j.soard.2008.08.003.
Bond DS, Vithiananthan S, Graham Thomas J, et al. Bari-Active: a randomized controlled trial of a preoperative intervention to increase physical activity in bariatric surgery patients. Surg Obes Relat Dis. 2015;11(1):169–77. https://doi.org/10.1016/j.soard.2014.07.010.
King WC, Kalarchian MA, Steffen KJ, et al. Associations between physical activity and mental health among bariatric surgical candidates. J Psychosom Res. 2013;74(2):161–9. https://doi.org/10.1016/j.jpsychores.2012.11.010.
Bandura A. Guide for constructing self-efficacy scales. In: Pajares F, Urdan T, editors. Self-efficacy Beliefs of Adolescents. Greenwich: Information Age Publishing; 2006. p. 307–37.
Igelstrom H, Emtner M, Lindberg E, et al. Physical activity and sedentary time in persons with obstructive sleep apnea and overweight enrolled in a randomized controlled trial for enhanced physical activity and healthy eating. Sleep Breath. 2013;17(4):1257–66. https://doi.org/10.1007/s11325-013-0831-6.
Everett B, Salamonson Y, Davidson PM. Bandura's exercise self-efficacy scale: validation in an Australian cardiac rehabilitation setting. Int J Nurs Stud. 2009;46(6):824–9. https://doi.org/10.1016/j.ijnurstu.2009.01.016.
Carrasco F, Ruz M, Rojas P, et al. Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg. 2009;19(1):41–6. https://doi.org/10.1007/s11695-008-9638-0.
Strauss BJ, Marks SJ, Growcott JP, et al. Body composition changes following laparoscopic gastric banding for morbid obesity. Acta Diabetol. 2003;40(1 Suppl):S266–S9. https://doi.org/10.1007/s00592-003-0083-1.
Strain GW, Gagner M, Pomp A, et al. Comparison of weight loss and body composition changes with four surgical procedures. Surg Obes Relat Dis. 2009;5(5):582–7. https://doi.org/10.1016/j.soard.2009.04.001.
Campbell PT, Katzmarzyk PT, Malina RM, et al. Prediction of physical activity and physical work capacity (PWC150) in young adulthood from childhood and adolescence with consideration of parental measures. Am J Hum Biol. 2001;13(2):190–6. https://doi.org/10.1002/1520-6300(200102/03)13:2<190::AID-AJHB1028>3.0.CO;2-N.
Bland J, Pfeiffer K, Eisenmann JC. The PWC170: comparison of different stage lengths in 11-16 year olds. Eur J Appl Physiol. 2012;112(5):1955–61. https://doi.org/10.1007/s00421-011-2157-z.
Hands B, Larkin D, Parker H, et al. The relationship among physical activity, motor competence and health-related fitness in 14-year-old adolescents. Scand J Med Sci Sports. 2009;19(5):655–63. https://doi.org/10.1111/j.1600-0838.2008.00847.x.
Wallman KE, Campbell L. Test-retest reliability of the Aerobic Power Index submaximal exercise test in an obese population. J Sci Med Sport. 2007;10(3):141–6. https://doi.org/10.1016/j.jsams.2006.05.024.
Wong PC, Chia MY, Tsou IY, et al. Effects of a 12-week exercise training programme on aerobic fitness, body composition, blood lipids and C-reactive protein in adolescents with obesity. Ann Acad Med Singap. 2008;37(4):286–93.
Healy GN, Clark BK, Winkler EA, et al. Measurement of adults' sedentary time in population-based studies. Am J Prev Med. 2011;41(2):216–27. https://doi.org/10.1016/j.amepre.2011.05.005.
Loprinzi PD, Kohli M. Effect of physical activity and sedentary behavior on serum prostate-specific antigen concentrations: results from the National Health and Nutrition Examination Survey (NHANES), 2003-2006. Mayo Clin Proc. 2013;88(1):11–21. https://doi.org/10.1016/j.mayocp.2012.10.012.
Chapman N, Hill K, Taylor S, et al. Patterns of physical activity and sedentary behavior after bariatric surgery: An observational study. Surg Obes Relat Dis. 2014;10(3):524–30. https://doi.org/10.1016/j.soard.2013.10.012.
Straker L, Campbell A, Mathiassen SE, et al. Capturing the pattern of physical activity and sedentary behavior: Exposure variation analysis of accelerometer data. J Phys Act Health. 2014;11(3):614–25. https://doi.org/10.1123/jpah.2012-0105.
Benedix F, Westphal S, Patschke R, et al. Weight loss and changes in salivary ghrelin and adiponectin: comparison between sleeve gastrectomy and Roux-en-Y gastric bypass and gastric banding. Obes Surg. 2011;21(5):616–24. https://doi.org/10.1007/s11695-011-0374-5.
Carlin AM, Zeni TM, English WJ, et al. The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg. 2013;257(5):791–7. https://doi.org/10.1097/SLA.0b013e3182879ded.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-Year outcomes from the fourth IFSO global registry report 2018. Obes Surg. 2019;29(3):782–95. https://doi.org/10.1007/s11695-018-3593-1.
Wilms B, Ernst B, Thurnheer M, et al. Differential changes in exercise performance after massive weight loss induced by bariatric surgery. Obes Surg. 2012;23(3):365–71. https://doi.org/10.1007/s11695-012-0795-9.
Hansen N, Hardin E, Bates C, et al. Preoperative change in 6-minute walk distance correlates with early weight loss after sleeve gastrectomy. Journal of the Society of Laparoendoscopic Surgeons. 2014;18(3):1–4. https://doi.org/10.4293/JSLS.2014.00383.
Berglind D, Willmer M, Eriksson U, et al. Longitudinal assessment of physical activity in women undergoing Roux-en-Y gastric bypass. Obes Surg. 2015;25(1):119–25. https://doi.org/10.1007/s11695-014-1331-x.
Livhits M, Mercado C, Yermilov I, et al. Patient behaviors associated with weight regain after laparoscopic gastric bypass. Obes Res Clin Pract. 2011;5(3):e169–266. https://doi.org/10.1016/j.orcp.2011.03.004.
Freire RH, Borges MC, Alvarez-Leite JI, et al. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition. 2012;28(1):53–8. https://doi.org/10.1016/j.nut.2011.01.011.
Karmali S, Brar B, Shi X, et al. Weight recidivism post-bariatric surgery: A systematic review. Obes Surg. 2013;23(11):1922–33. https://doi.org/10.1007/s11695-013-1070-4.
Alvarez V, Carrasco F, Cuevas A, et al. Mechanisms of long-term weight regain in patients undergoing sleeve gastrectomy. Nutrition. 2015; https://doi.org/10.1016/j.nut.2015.08.023.
Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31(2):369–71. https://doi.org/10.2337/dc07-1795.
Chau JY, van der Ploeg HP, Merom D, et al. Cross-sectional associations between occupational and leisure-time sitting, physical activity and obesity in working adults. Prev Med. 2012;54(3-4):195–200. https://doi.org/10.1016/j.ypmed.2011.12.020.
Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30(6):1384–9. https://doi.org/10.2337/dc07-0114.
Adams MM, Davis PG, Gill DL. A hybrid online intervention for reducing sedentary behavior in obese women. Front Public Health. 2013;1:45–50. https://doi.org/10.3389/fpubh.2013.00045.
Rosenberg DE, Gell NM, Jones SM, et al. The feasibility of reducing sitting time in overweight and obese older adults. Health Educ Behav. 2015;42(5):669–76. https://doi.org/10.1177/1090198115577378.
Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380:258–71.
Zabatiero J, Smith A, Hill K, et al. Do factors related to participation in physical activity change following restrictive bariatric surgery? a qualitative study. Obes Res Clin Pract. 2017;12:307–16. https://doi.org/10.1016/j.orcp.2017.11.001.
Teixeira PJ, Marques MM, Silva MN, et al. Classification of techniques used in self-determination theory-based interventions in health contexts: An expert consensus study. Motivation Science. 2020;6:438–55. https://doi.org/10.1037/mot0000172.
Clark BK, Healy GN, Winkler EA, et al. Relationship of television time with accelerometer-derived sedentary time: NHANES. Med Sci Sports Exerc. 2011;43(5):822–8. https://doi.org/10.1249/MSS.0b013e3182019510.
Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps per day in US adults. Med Sci Sports Exerc. 2009;41(7):1384–91. https://doi.org/10.1249/MSS.0b013e318199885c.
Olander EK, Fletcher H, Williams S, et al. What are the most effective techniques in changing obese individuals' physical activity self-efficacy and behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2013;10:29–43. https://doi.org/10.1186/1479-5868-10-29.
McEwan D, Harden SM, Zumbo BD, et al. The effectiveness of multi-component goal setting interventions for changing physical activity behaviour: a systematic review and meta-analysis. Health Psychol Rev. 2015;10:1–22. https://doi.org/10.1080/17437199.2015.1104258.
O'Brien N, McDonald S, Araujo-Soares V, et al. The features of interventions associated with long-term effectiveness of physical activity interventions in adults aged 55-70 years: asystematic review and meta-analysis. Health Psychol Rev. 2015;9(4):417–33. https://doi.org/10.1080/17437199.2015.1012177.
Gonzalez-Cutre D, Megias A, Beltran-Carrillo VJ, et al. Effects of a physical activity program on post-bariatric patients: a qualitative study from a self-determination theory perspective. J Health Psychol. 2018;1359105318770729:1743–54. https://doi.org/10.1177/1359105318770729.
Chastin SF, Palarea-Albaladejo J, Dontje ML, et al. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: a novel compositional data analysis Approach. PLoS One. 2015;10(10):1–37. https://doi.org/10.1371/journal.pone.0139984.
Bailey DP, Locke CD. Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J Sci Med Sport. 2015;18(3):294–8. https://doi.org/10.1016/j.jsams.2014.03.008.
Funding
Juliana Zabatiero was funded by a Curtin Strategic International Research Scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Device-based physical activity and sedentary time do not change post-surgery
• The majority of waking hours were spent accumulating sedentary time
• Little time was spent in light or moderate-to-vigorous intensity physical activity
Rights and permissions
About this article
Cite this article
Zabatiero, J., Smith, A., Gucciardi, D.F. et al. Patterns of Change in Device-Based Physical Activity and Sedentary Time Following Bariatric Surgery: a Longitudinal Observational Study. OBES SURG 31, 3015–3025 (2021). https://doi.org/10.1007/s11695-021-05337-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05337-6