Abstract
Background
Better outcomes at high-volume surgical centers have driven regionalization of complex surgical care. In turn, access to high-volume centers often requires travel over longer distances. We sought to characterize travel patterns among patients who underwent a hepatectomy.
Methods
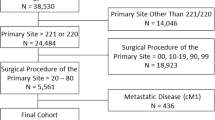
The California Office of Statewide Health Planning database was used to identify patients who underwent hepatectomy between 2005 and 2016. Total distance traveled and whether a patient bypassed the nearest hospital that performed hepatectomy to get to a higher-volume center were assessed. Multivariate analyses were used to identify factors associated with bypassing a local hospital for a higher-volume center.
Results
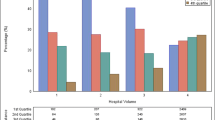
Overall, 13,379 adults underwent a hepatectomy in 229 hospitals; only 26 hospitals were high volume (> 15 cases/year). Median travel time to a hospital that performed hepatectomy was 25.2 min (IQR: 13.1–52.0). The overwhelming majority of patients (91.6%) bypassed the nearest providing hospital to seek care at a destination hospital. Among patients who bypassed a closer hospital, 75.5% went to a high-volume hospital. Outcomes at destination hospitals were improved compared with nearest hospitals (incidence of complications: 20.4% vs. 22.9% %; failure-to-rescue: 7.1% vs 10.9%; mortality 1.5% vs. 2.6%). Medicaid beneficiaries (OR 0.69, 95%CI 0.56–0.85) were less likely to bypass the nearest hospital to go to a high-volume hospital; additionally, Medicaid patients were less likely to undergo hepatectomy at a high-volume hospital independent of bypassing the nearest hospital (OR 0.60, 95%CI 0.48–0.76). Among the 3703 patients who underwent hepatectomy at a low-volume center, 2126 patients had actually bypassed a high-volume hospital. Among the remaining 1577 patients, 95% of individuals would have needed to travel less than 1 additional hour to reach a high-volume center.
Conclusion
Roughly, one-quarter of patients undergoing hepatectomy received care at a low-volume center; nearly all of these patients either bypassed a high-volume hospital or would have needed to travel less than an additional hour to reach a high-volume center. Travel distance needs to be considered in policies and healthcare delivery design to improve care of patients undergoing hepatic resection.


Similar content being viewed by others
References
Levy H, Janke A. Health Literacy and Access to Care. J Health Commun. 2016;21 Suppl 1:43–50.
Schoen C, Osborn R, Squires D, et al. Access, affordability, and insurance complexity are often worse in the United States compared to ten other countries. Health Aff Proj Hope. 2013;32:2205–2215.
Collins SR, Gunja MZ, Doty MM, et al. Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction Available from: http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction. 2016. .
Diaz A, Schoenbrunner A, Pawlik TM. Trends in the Geospatial Distribution of Inpatient Adult Surgical Services across the United States. Ann Surg. . Epub ahead of print May 7, 2019. DOI: https://doi.org/10.1097/SLA.0000000000003366.
Diaz A, Schoenbrunner A, Cloyd J, et al. Geographic Distribution of Adult Inpatient Surgery Capability in the USA. J Gastrointest Surg Off J Soc Surg Aliment Tract. . Epub ahead of print January 7, 2019. DOI: https://doi.org/10.1007/s11605-018-04078-9.
Chhabra KR, Dimick JB. Strategies for Improving Surgical Care: When Is Regionalization the Right Choice? JAMA Surg. 2016;151:1001–1002.
Ellison EC, Pawlik TM, Way DP, et al. The impact of the aging population and incidence of cancer on future projections of general surgical workforce needs. Surgery. . Epub ahead of print November 24, 2017. DOI: https://doi.org/10.1016/j.surg.2017.09.035.
Pfuntner A, Wier LM, Stocks C. Most Frequent Procedures Performed in U.S. Hospitals, 2011: Statistical Brief #165. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US) Available from: http://www.ncbi.nlm.nih.gov/books/NBK174682/. 2006. .
De Oliveira GS, McCarthy RJ, Wolf MS, et al. The impact of health literacy in the care of surgical patients: a qualitative systematic review. BMC Surg.;15 . Epub ahead of print July 17, 2015. DOI: https://doi.org/10.1186/s12893-015-0073-6.
Zogg CK, Scott JW, Jiang W, et al. Differential access to care: The role of age, insurance, and income on race/ethnicity-related disparities in adult perforated appendix admission rates. Surgery. 2016;160:1145–1154.
Beal EW, Mehta R, Merath K, et al. Outcomes After Resection of Hepatocellular Carcinoma: Intersection of Travel Distance and Hospital Volume. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2019;23:1425–1434.
Diaz A, Burns S, Paredes AZ, et al. Accessing Surgical Care for Pancreaticoduodenectomy: Patient Variation in Travel Distance and Choice to Bypass Hospitals to Reach Higher Volume Centers. J Surg Oncol.
Xu Z, Becerra AZ, Justiniano CF, et al. Is the Distance Worth It? Patients With Rectal Cancer Traveling to High-Volume Centers Experience Improved Outcomes. Dis Colon Rectum. 2017;60:1250–1259.
Stitzenberg KB, Sigurdson ER, Egleston BL, et al. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27:4671–4678.
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–2137.
Fong ZV, Loehrer AP, Fernández-Del Castillo C, et al. Potential impact of a volume pledge on spatial access: A population-level analysis of patients undergoing pancreatectomy. Surgery. 2017;162:203–210.
Gani F, Azoulay D, Pawlik TM. Evaluating Trends in the Volume-Outcomes Relationship Following Liver Surgery: Does Regionalization Benefit All Patients the Same? J Gastrointest Surg Off J Soc Surg Aliment Tract. 2017;21:463–471.
Glasgow RE, Showstack JA, Katz PP, et al. The Relationship Between Hospital Volume and Outcomes of Hepatic Resection for Hepatocellular Carcinoma. Arch Surg. 1999;134:30–35.
Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127.
Birkmeyer JD, Siewers AE, Marth NJ, et al. Regionalization of high-risk surgery and implications for patient travel times. JAMA. 2003;290:2703–2708.
The Leapfrong Group. Surgeon Volume and Surgical Appropriateness. Leapfrog. Available from: http://www.leapfroggroup.org/surgeon-volume. 2017. Accessed March 10, 2019.
Alvino DML, Chang DC, Adler JT, et al. How Far Are Patients Willing to Travel for Gastrectomy? Ann Surg. 2017;265:1172–1177.
Finlayson SR, Birkmeyer JD, Tosteson AN, et al. Patient preferences for location of care: implications for regionalization. Med Care. 1999;37:204–209.
Merath K, Chen Q, Diaz A, et al. Local referrals as a strategy for increasing value of surgical care among medicare patients undergoing liver and pancreatic surgery. HPB. . Epub ahead of print April 15, 2019. DOI: https://doi.org/10.1016/j.hpb.2019.03.371.
Smith ME, Shubeck SP, Nuliyalu U, et al. Local Referral of High-risk Patients to High-quality Hospitals: Surgical Outcomes, Cost Savings, and Travel Burdens. Ann Surg. . Epub ahead of print January 17, 2019. https://doi.org/10.1097/SLA.0000000000003208.
Sheetz KH, Dimick JB, Nathan H. Centralization of High-Risk Cancer Surgery Within Existing Hospital Systems. J Clin Oncol Off J Am Soc Clin Oncol. 2019;JCO1802035.
Beal EW, Mehta R, Tsilimigras DI, et al. Travel to a high volume hospital to undergo resection of gallbladder cancer: does it impact quality of care and long-term outcomes? HPB. . Epub ahead of print June 8, 2019. https://doi.org/10.1016/j.hpb.2019.05.004.
Beal EW, Mehta R, Hyer JM, et al. Association Between Travel Distance, Hospital Volume, and Outcomes Following Resection of Cholangiocarcinoma. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2019;23:944–952.
Dimick JB, Cowan JA, Knol JA, et al. Hepatic Resection in the United States: Indications, Outcomes, and Hospital Procedural Volumes From a Nationally Representative Database. Arch Surg. 2003;138:185–191.
Diaz A, Pawlik TM. Optimal Location for Centralization of Hospitals Performing Pancreas Resection in California in California. JAMA Surg.;In Press.
Ryan AM, Krinsky S, Maurer KA, et al. Changes in Hospital Quality Associated with Hospital Value-Based Purchasing. N Engl J Med. 2017;376:2358–2366.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Dr. Diaz received salary support from the Veterans Affairs Office of Academic Affiliations during the time of the study.
Conflict of Interest
The authors of this research have no conflict of interest to report.
Disclaimer
This does not necessarily represent the views of the United States Government or Department of Veterans Affairs.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Diaz, A., Cloyd, J.M., Manilchuk, A. et al. Travel Patterns among Patients Undergoing Hepatic Resection in California: Does Driving Further for Care Improve Outcomes?. J Gastrointest Surg 25, 1471–1478 (2021). https://doi.org/10.1007/s11605-019-04501-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04501-9