Abstract
Background
Medial opening-wedge high tibial osteotomy (HTO) is one of the most common and effective HTO techniques, in which the proximal tibia is cut medially, leaving an intact lateral hinge of bone that can be opened to a variable amount for the desired correction, but the technical complications of lateral cortex fracture and intra-articular fracture are well described. The lateral bone hinge for medial opening-wedge HTO is crucial. If the hinge is too small, the tibia can fracture and become unstable, requiring further fixation. If the hinge is too large, the osteotomy can propagate into the joint as an intra-articular fracture when opening the osteotomy.
Purpose
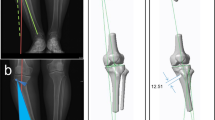
We propose a new technique that utilizes digital preoperative templating to improve the accuracy of the cut. Preoperative digital templating may allow the surgeon to reproducibly obtain a lateral bone hinge of 10 mm, while also reducing radiation exposure relative to the traditional fluoroscopically assisted technique.
Methods
Ten cadaver extremities from five cadavers were matched into pairs and randomized into two groups: those with and without preoperative templating. The templating protocol measures the distance between two points on the medial and lateral cortices, and 20 mm is subtracted to determine the depth of the saw cut (10 mm for the hinge and another 10 mm because the proximal tibia is oval in shape). The control method was done by making the cut using fluoroscopy with tactile feedback. Postoperative computed tomography scans were obtained of all legs to measure the width of the lateral bone hinge. Intraoperative fluoroscopy used during both techniques and the numbers of fluoroscopy shots were recorded.
Results
We found neither the treatment group with preoperative planning nor the control group with the conventional technique had bone hinge widths that were different from the ideal 10 mm. The average hinge widths for the treatment and control groups were 11.2 and 11.5 mm, respectively. However, the treatment group was exposed to significantly less intraoperative fluoroscopy during the osteotomy cut. The average total number of fluoroscopy shots was 2.2 in the treatment group versus 6.3 for the control group.
Conclusions
This new preoperative planning technique achieves similar accuracy of the lateral bone hinge when compared to current methods but exposes the patient, surgeon, and staff to significantly less intraoperative radiation.


Similar content being viewed by others
References
Badawy M, Fenstad AM, Indrekvam K, Havelin LI, Furnes O. The risk of revision in total knee arthroplasty is not affected by previous high tibial osteotomy. Acta Orthop. 2015;86(6):734–739. https://doi.org/10.3109/17453674.2015.1060402
Badman BL. Radiation exposure with use of the mini-c-arm for routine orthopaedic imaging procedures. J Bone Joint Surg. 2005;87(1):13. https://doi.org/10.2106/JBJS.D.02162
Bar-On E, Weigl DM, Becker T, Katz K, Konen O. Intraoperative C-arm radiation affecting factors and reduction by an intervention program. J Pediatr Orthop. 2010;30(4):320–323. https://doi.org/10.1097/BPO.0b013e3181d98f06
Blattert TR, Fill UA, Kunz E, Panzer W, Weckbach A, Regulla DF. Skill dependence of radiation exposure for the orthopaedic surgeon during interlocking nailing of long-bone shaft fractures: a clinical study. Arch Orthop Trauma Surg. 2004;124(10):659–664. https://doi.org/10.1007/s00402-004-0743-9
Bode G, von Heyden J, Pestka J, et al. Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):1949–1955. https://doi.org/10.1007/s00167-013-2762-y
Botchu R, Ravikumar K. Radiation exposure from fluoroscopy during fixation of hip fracture and fracture of ankle: Effect of surgical experience. Indian J Orthop. 2008;42(4):471–473. https://doi.org/10.4103/0019-5413.43398
Brinkman J-M, Lobenhoffer P, Agneskirchner JD, et al. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg [Br]. 2008;90:1548–1557. https://doi.org/10.1302/0301-620X.90B12
Chou LB, Cox CA, Tung JJ, Harris AHS, Brooks-Terrell D, Sieh W. Prevalence of cancer in female orthopaedic surgeons in the United States. J Bone Joint Surg Am. 2010;92(1):240–244. https://doi.org/10.2106/JBJS.H.01691
Chou LB, Lerner LB, Harris AHS, Brandon AJ, Girod S, Butler LM. Cancer Prevalence among a Cross-sectional Survey of Female Orthopedic, Urology, and Plastic Surgeons in the United States. Womens Health Issues. 2015; 25(5):476–481. https://doi.org/10.1016/j.whi.2015.05.005
DeMeo PJ, Johnson EM, Chiang PP, Flamm AM, Miller MC. Midterm follow-up of opening-wedge high tibial osteotomy. Am J Sports Med. 2010;38(10):2077–2084. https://doi.org/10.1177/0363546510371371
Dexel J, Fritzsche H, Beyer F, Harman MK, Lützner J. Open-wedge high tibial osteotomy: incidence of lateral cortex fractures and influence of fixation device on osteotomy healing. Knee Surg Sports Traumatol Arthrosc. 2015. https://doi.org/10.1007/s00167-015-3730-5
Domholdt E. Physical Therapy Research. Philadelphia: W.B. Saunden Company; 1993.
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):170–180. https://doi.org/10.1007/s00167-012-2087-2
Giordano BD, Grauer JN, Miller CP, Morgan TL, Rechtine GR. Radiation exposure issues in orthopaedics. J Bone Joint Surg Am. 2011;93(12):e69(1)-e69(10). https://doi.org/10.2106/JBJS.J.01328
Giuseffi SA, Replogle WH, Shelton WR. Opening-Wedge High Tibial Osteotomy: Review of 100 Consecutive Cases. Arthroscopy. 2015;31(11):2128–2137. https://doi.org/10.1016/j.arthro.2015.04.097
Greene DJ, Tenggadjaja CF, Bowman RJ, Agarwal G, Ebrahimi KY, Baldwin DD. Comparison of a reduced radiation fluoroscopy protocol to conventional fluoroscopy during uncomplicated ureteroscopy. Urology. 2011;78(2):286–290. https://doi.org/10.1016/j.urology.2010.11.020
Hui C, Salmon LJ, Kok A, et al. Long-term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am J Sports Med. 2011;39(1):64–70. https://doi.org/10.1177/0363546510377445
Kessler OC, Jacob HAC, Romero J. Avoidance of medial cortical fracture in high tibial osteotomy: improved technique. Clin Orthop Relat Res. 2002;(395):180–185.
Khan IA, Kamalasekaran S, Fazal MA. Risk of ionising radiation to trainee orthopaedic surgeons. Acta Orthop Belg. 2012;78(1):106–110.
Kolb W, Guhlmann H, Windisch C, Kolb K, Koller H, Grützner P. Opening-wedge high tibial osteotomy with a locked low-profile plate. J Bone Joint Surg Am. 2009;91(11):2581–2588. https://doi.org/10.2106/JBJS.H.01047
Lee YS, Moon GH. Comparative analysis of osteotomy accuracy between the conventional and devised technique using a protective cutting system in medial open-wedge high tibial osteotomy. J Orthop Sci. 2015;20(1):129–136. https://doi.org/10.1007/s00776-014-0663-7
Mastrangelo G, Fedeli U, Fadda E, Giovanazzi A, Scoizzato L, Saia B. Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond). 2005;55(6):498–500. https://doi.org/10.1093/occmed/kqi048
Miller ME, Davis ML, MacClean CR, Davis JG, Smith BL, Humphries JR. Radiation exposure and associated risks to operating-room personnel during use of fluoroscopic guidance for selected orthopaedic surgical procedures. J Bone Joint Surg Am. 1983;65(1):1–4.
Nelson EM, Monazzam SM, Kim KD, Seibert JA, Klineberg EO. Intraoperative fluoroscopy, portable X-ray, and CT: patient and operating room personnel radiation exposure in spinal surgery. Spine J. 2014;14(12):2985–2991. https://doi.org/10.1016/j.spinee.2014.06.003
Poignard A. Revisiting high tibial osteotomy: fifty years of experience with the opening-wedge technique. J Bone Joint Surg. 2010;92(Supplement_2):187. https://doi.org/10.2106/JBJS.I.00771
Riley SA. Radiation exposure from fluoroscopy during orthopedic surgical procedures. Clin Orthop Relat Res. 1989;(248):257–260.
Saragaglia D, Blaysat M, Inman D, Mercier N. Outcome of opening wedge high tibial osteotomy augmented with a Biosorb® wedge and fixed with a plate and screws in 124 patients with a mean of ten years follow-up. Int Orthop. 2011;35(8):1151–1156. https://doi.org/10.1007/s00264-010-1102-9
Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005; 13(1):69–76.
Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia—early results in 92 cases. Injury. 2003;34 Suppl 2:B55–62.
W-Dahl A, Toksvig-Larsen S, Lindstrand A. Ten-year results of physical activity after high tibial osteotomy in patients with knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2015. https://doi.org/10.1007/s00167-015-3693-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Elad Spitzer, MD, Joseph J. Ruzbarsky, MD, John B. Doyle, BA, Kaitlyn L. Yin, BA, declare they have no conflict of interest. Robert G. Marx, MD, MSc, FRCS, reports receiving research funding from DePuy Synthes to support this work, as well as book royalties from Springer and Demos Health and Deputy and Associate Editorships at Journal of Bone and Joint Surgery outside this work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
N/A
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Rights and permissions
About this article
Cite this article
Spitzer, E., Ruzbarsky, J.J., Doyle, J.B. et al. A New Preoperative Planning Technique Can Reduce Radiation Exposure During the Performance of Medial Opening-Wedge High Tibial Osteotomy. HSS Jrnl 14, 251–257 (2018). https://doi.org/10.1007/s11420-017-9591-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-017-9591-3