Abstract
Purpose
The aim of this study was to evaluate the accuracy of a patient-specific cutting guide on both coronal and sagittal alignment compared to the pre-operative planning in OWHTO.
Methods
Twelve OWHTO on 6 cadaveric specimens were performed by 3 experienced knee surgeons using patient-specific cutting guides based on 3D pre-operative planning. Since the specimens had no major deformities, a fixed correction of 6° on the left and 10° on the right legs were carried out to simulate different scenarios. A pre-operative and post-OWHTO 3D CT scans were performed, and images were superimposed using the dedicated 3D planning software to align their reference axes. A pre-operative planning was performed considering both Medial Proximal Tibial Angle (MPTA) and Posterior Tibial Slope (PTS), and a patient-specific cutting guide was produced. Planned and post-OWHTO MPTA and PTS were evaluated (mean and standard deviation), and Pearson’s correlation coefficient was calculated to assess precision and accuracy of the whole treatment.
Results
A mean correction of 6,1° (SD 1,9°) and 1,2° (SD 1°) was obtained respectively in the coronal plane (MPTA) and in the sagittal plane (PTS). The average difference between planned and post-OWHTO MPTA and PTS was respectively 1,2° (SD 0,6°) and 1,2° (SD 1°) in the sagittal plane (PTS). Pearson’s correlation coefficient demonstrated a good accuracy of the treatment in both coronal and sagittal plane (respectively r=0,95 and r=0,86). No lateral hinge fractures were detected at the post-operative CT scan.
Conclusion
OWTHO performed with the help of 3D patient specific cutting guide on cadaveric specimens demonstrated good accuracy and reliability in obtaining the planned correction. In vivo studies are necessary to confirm these results and evaluate cost-effectiveness of this system.
Level of evidence
Level IV cadaveric study.
Similar content being viewed by others
Introduction
Opening Wedge High Tibial Osteotomy (OWHTO) is a valid treatment for medial compartment arthritis/overload in young patients with a varus aligned knee [1, 2]. The aim of OWHTO is to correct the limb malalignment on the coronal plane, but some effect on posterior tibial slope (PTS) should be expected. Particularly, Noyes et al demonstrated that medial OWHTO increases the tibial slope only if the anteromedial gap is equal to the posteromedial gap, whereas the slope does not change if the anteromedial gap is smaller than the posteromedial one [3]. Furthermore, it has been recently confirmed that not all the varus deformities should be corrected on the tibia only, because it can produce an excessive increase of the medial Mechanical Proximal Tibial Angle (MPTA) which may result in pathological lateral inclination of the joint line, increased cartilage shear stress and possible inferior clinical outcome [2, 4]. Historically, the goal of OWHTO was to shift the mechanical axis from the medial to the lateral side of the knee, aiming at the Fujisawa point, which was located on the tibial plateau at 62.5% of the medial-lateral width [5]. However, in the last years different authors demonstrated that correcting up to Fujisawa point may lead to a greater risk for lateral compartment damage, and a correction to 55% of the tibial width, which represent the apex of the lateral tibial spine, may be a good compromise to avoid excessive under-correction or lateral compartment damage [6].
In this scenario, an accurate pre-operative planning with identification of the correct osteotomy site and amount of correction on both coronal and sagittal plane is mandatory [7, 8]. Different studies confirmed that accuracy of correction relative to preoperative planning is strictly associated to HTO outcomes [9, 10]. Unfortunately, conventional technique (i.e. radiopaque cable under fluoroscopy) achieves post-operative alignment within 3° of planned mechanical femoro-tibial angle (mFTA) in only 50-70% of the cases [11].
Computer-assisted surgery (CAS) may help surgeons in obtaining a better intra-operative accuracy for mechanical axis, but this technology is costly and associated to a long learning curve [12]. However, some studies reported on high rate of outliers also with CAS HTO, even if they were not associated to worse outcomes [13].
Recently 3D patient-specific cutting guides (PSCG) based on Computer Tomography (CT) scans were developed. Preliminary in vitro studies described very good accuracy for some PSCG systems on both the coronal and sagittal plane [14,15,16,17].
In this study, a new PSCG based on pre-operative CT scans for OWHTO was tested. The first aim of this study was to evaluate the accuracy of the system on both coronal and sagittal plane. Secondary aim of the study was to evaluate the number of complications related to the osteotomy (i.e. intra-articular fracture), which were supposed to be reduced with a PSCG.
Material and methods
Study design
Six frozen human cadavers were obtained from ScienceCare ®. Cadavers with previous surgery on the lower limb, or previous skeletal deformity, were excluded.
A total of 12 HTO were performed, 6 on the left and 6 on the right knees, by 3 experienced knee surgeons, with good experience in performing OWHTO (R.R., N.P., S.R.).
OWHTO pre-operative planning
All specimens were scanned pre- and post-operatively with the same CT scan protocol.
To be able to simulate the realignment osteotomy (tibia and/or femur) based on the mechanical leg axis, 3D models of the corresponding bone parts must be obtained. The proximal femur, the knee, and the ankle joints were acquired in a single CT scan to avoid specimen’s movements. Different points should be considered in both clinical and experimental setting to obtain a correct CT data, and they were respected in both pre and post-operative CT scan: 1) axial resolution of 1 mm, in-plane resolution <0.4 mm, peak kilovoltage 120 kvp and tube current 135 mA; 2) Field Of View maximum 200 mm; 3) Slice Thickness (Hip, knee and ankle) of 1 mm, with slice increment of 0-5 mm; 4) hip should be included from the proximal joint space to at least ¼ of the proximal femoral shaft, with the lower conical x-ray beam limit at the lesser trochanter; 5) knee should be included from 15 cm above to 20 cm below the joint line; 6) ankle should be included from 5 cm above the joint line to the center of calcaneus (including lateral and medial). All the DICOM images were imported in a dedicated software (MyOsteotomy®, Medacta, Switzerland), and a 3D geometrical model was created for pre-operative planning. Preoperative Mechanical Proximal Tibial Angle (MPTA) and Posterior Tibial Slope (PTS) were measured to evaluate coronal and sagittal plane alignment, since an accuracy on both plane is mandatory to obtain good outcomes.
Since the specimens had no major deformities, a fixed correction of 6° on the left and 10° on the right legs were carried out to simulate different scenarios. The pre-operative planning was performed with Solidworks® using the registered MyKnee® procedure (Medacta, Switzerland), to calculate anatomical axes, planes and landmarks. The three involved surgeons were invited to complete the planning, checking both cutting plane position and results from OWHTO simulation. If surgeons were not satisfied from automated simulation, they could modify both planning and cutting plane position. The osteotomy was oriented in such a way that tibial slope was not affected (parallel to sagittal plane) and the hinge was planned passing through a ‘safe zone’ to avoid bone fracture propagation, identified by tibio-fibular joint area [18] (Fig. 1). The planning was then confirmed, and the surgeon received all the information to perform the osteotomy (including amount of opening, saw blade and chisel depth and number to avoid lateral hinge fracture, plate positioning and screws length) as well as the personalized cutting guide and relative proximal tibia model (Fig. 2).
Planning of the hinge passing through the ‘safe zone’ as described by Nakamura et al [18]. The red bar shows the hinge in the frontal, upper and lateral view
Definitive pre-operative planning of one of the cases. A Frontal and axial view of the plate and screws; B) Length and position of the alignment rod which will be reproduce intra-operatively to confirm the guide positioning; C) First chisel depth and number of chisels needed to obtain the planned gap opening; D) screw length and type
OWHTO surgical technique
A 5 cm incision on the anteromedial aspect of the tibia, extending from 1 cm below the medial joint line midway between the medial border of the tibial tubercle and the posteromedial border of the tibia was performed, as previously described [19]. The sartorius fascia, pes anserinus and Medial Collateral Ligament (MCL) were retracted. The personalized cutting guide was positioned on the antero-medial tibia, and the position was checked with the dedicated alignment rod (Figs. 3 and 4).
When the correct position is achieved, two 3.2 mm pins are inserted to fix the cutting guide, and the k-wires can be inserted into the dedicated holes in the cutting slot to check osteotomy orientation with fluoroscopy and the dedicated alignment rod. The bone cut was performed through the cutting slot with a 1 mm saw blade, the anterior pin was removed as well as the cutting guide, leaving only the posterior pin as a reference. The osteotomy was then performed with dedicated chisels in a standard manner, being careful not to damage the lateral hinge point and to avoid unexpected crack propagation. First chisel length was indicated in the pre-operative planning, as shown in Fig. 1. Chisels are consequently numbered to obtain the appropriate gap opening, depending on the number of chisels planned (Fig. 5). Once the osteotomy is opened and the gap is as planned, the toothed plate is positioned. The tooth is custom-made to the exact dimension and shape planned. The alignment was checked intra-operatively with fluoroscopy and the dedicated rod. Also, the position of the plate against the planned position are checked mechanically. Once the correct position of the plate is verified, the screws can be inserted, starting from the posterior distal (cortical screw) and the anterior proximal (cancellous screw). After checking that the inferior osteotomy plane is well in contact with the wedge of the plate, the last two screws can be inserted. Length and position of all the screws are reported in the planning. Figure 6 shows the result.
Registration process
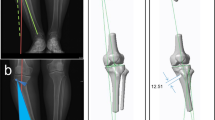
All the specimens underwent post-operative fluoroscopy and CT scan. To compare pre-operative and post-OWHTO CT scans, the images of the bones were aligned in the area of the tibial plateau that was not affected by the osteotomy using a best-fit algorithm in CASPA® software. With this strategy, all anatomical landmarks in the proximal tibia (e.g. tibia center, lateral and medial posterior walls, tibial lateral and medial points, anterior and posterior plateau points) were exactly coincident in all scenarios (pre-operative, planned OWHTO and post-operative), thus avoiding errors in plane and axes calculation that could originate from using different anatomical landmarks (Fig. 7).
MPTA angle and PTS were compared in planned-OWHTO and post-OWHTO scenarios to assess the precision and accuracy of the treatment.
Statistical analysis
Statistical analysis was performed between planned-OWHTO and post-OWHTO MPTA and PTS angles. Pearson’s correlation test was used to evaluate the accuracy of patient-specific cutting guide comparing planned and post-OWHTO MPTA and PTS. Significance was considered at p<0,05. Data were presented with mean, range, and standard deviation (SD), as well as Confidence Intervals (CI) if available. Considering a standard deviation of 1° and a clinically relevant difference of 1,5°, with α=0,05 and β=0,20, 7 samples were necessary to achieve statistical significance.
Results
The mean pre-operative MPTA was 87,9° (SD 1,8°) and the mean pre-operative PTS was 8° (SD 3°). A mean correction of 6,1° (SD 1,9°) was obtained in the coronal plane (MPTA) and 1,2° (SD 1°) in the sagittal plane (PTS).
For all the specimens, the cutting guide was positioned on the tibial bone as planned, with a good fit, so all the osteotomies were performed according to the planning.
The mean difference between the planned-OWHTO and post-OWHTO configuration was 1,2° (SD 0,6°) on the coronal plane (MPTA) and 1,2° (SD 1°) in the sagittal plane (PTS) (Table 1).
Pearson’s correlation coefficient was used to evaluate the association between planned-OWHTO and post-OWHTO values, demonstrating a strong correlation for both MPTA and PTS (MPTA r=0,95, 95%CI 0,83-0,98, p<0,001; PTS r=0,86, 95%CI 0,56-0,96, p=0,004, Table 2).
No complication related to the osteotomy, such as lateral hinge fractures, were detected at the post-operative CT scan. Furthermore, all the ostomies were performed at the planned level, confirming no tibial guide malposition.
Discussion
The most important finding of the present study is that this PSCG demonstrated good accuracy in both coronal and sagittal plane, with high correlation between planned and post-operative MPTA and PTS (respectively r=0,95 and r=0,86). The average difference between planned and post-operative MPTA was 1,2° (SD 0,6°), which can be considered acceptable. Similarly, the average difference between planned and post-OWHTO PTS was 1,2° (SD 1°), demonstrating a good control of the tibial slope, which is mandatory to achieve good outcomes after OWHTO. In all the cases the cutting guide was correctly positioned according to the digital pre-operative planning and the 3D-printed model.
OWHTO has been reported to offer good long-term outcomes if performed with correct indications and precise surgical technique [2, 20, 21]. Careful pre-operative planning, identification of the location of the deformity and accurate surgical technique are mandatory to obtain those good results. Unfortunately, previous studies demonstrated low accuracy for the targeted alignment in conventional OWHTO, with over 30% of outliers from the accuracy range [11]. Furthermore, the association between an over- or under-correction and poor long-term outcomes has been demonstrated [22], and the same has been reported for the modification of the tibial slope, which should be avoided [23]. For all these reasons, a more precise instrumentation, as the one proposed in this study, can be useful in OWHTO.
Some studies described the accuracy of other type of patient-specific instrumentations. Donnez et al evaluated the accuracy of the PSCG in 10 cadavers using a CT scan protocol like the one described in this study. The authors concluded about a high accuracy of the system, with Pearson’s correlation coefficient values similar to those obtained in this study [14]. Miao et al evaluated the accuracy of an angular spacer on 8 specimens, with no significant differences in planned and post-operative MPTA [17]. However, CT scan measurements were performed separately and not superimposed, which may induce doubts in the validity of the comparison. Thanks to the registration process performed in this study, all the measurements were aligned on the same axis, allowing the surgeons to evaluate only the real correction achieved.
There is a paucity of published clinical studies on PSCG’s outcomes [24, 25]. Particularly, Chaouche et al reported about the safety and accuracy of PSCG in 100 OWHTO. The authors concluded about high accuracy of the system also in vivo, with good positioning of the cutting guide in all cases, and an overall complication rate similar to the one reported with the conventional technique [26]. Oher authors similarly concluded on good outcomes and better accuracy of PSCG compared to conventional technique in OWHTO [27]. Finally, in a recent systematic review including 14 studies, Aman et al confirmed good in vivo accuracy with PSCG in both distal femoral and proximal tibia osteotomies, with an outlier rate from the target alignment ranging between 0% and 25% [28]. More recently different studies have been published on the accuracy of PSCG in more complex osteotomies (i.e. double level osteotomy), with good results [29,30,31]. However, Abdelhameed et al in their series of 91 osteotomies concluded that conventional technique are as accurate as PSCG if performed by an experienced surgeon [32].
Different intra-operative methods to control alignment correction during OWHTO have been proposed other than PSCG, including Computer Assisted Surgery (CAS). Some clinical studies confirmed a higher accuracy for computer navigated OWHTO compared to conventional technique, with still 22% of outliers to the target alignment [11, 33]. However, Hasegawa et al in their clinical study concluded that the Joint Line Convergence Angle (JLCA) was significantly higher in the outlier group, thus underlying a possible defect in pre-operative planning. Furthermore, the same authors concluded that despite the high rate of outliers to the target coronal alignment (18%), mid-term outcomes were still excellent in computer-assisted OWHTO [13].
Another possible problem the surgeons may face during an OWHTO is the hinge fracture, which occurs in 20-30% of the cases, and it is strictly associated to the amount of gap opening [18]. No lateral hinge fractures were detected in this study at the post-operative CT scan, despite the poor bone quality of specimens compared to healthy, vital bone. A careful preoperative planning and surgical technique are surely key factors to reduce the rate of hinge fractures. The PSCG, together with the 3D pre-operative planning, may help surgeons in reducing the rate of hinge fracture, because the position of the hinge and the depth of the osteotomy are carefully assessed during preoperative planning and then reproduced in vivo with the support of the PSC guides.
One of the disadvantages of PSCG is the need for a pre-operative CT scan, which is not performed routinely. However, this technique may reduce the number of intra-operative fluoroscopic images required. Jacquet et al in their clinical study underlined that the average number of fluoroscopic images in OWHTO assisted with a PSCG is around 4 after a learning curve of 9 cases [26].
This study has some limitations. First the small number of specimen and surgeries (6 specimens, 12 cases), even if the power analysis demonstrated that 7 cases were enough to demonstrate statistically significant differences. Furthermore, the specimens did not have a significant varus deformity of the proximal tibia to be considered candidate for an OWHTO. However, two different amounts of deformity correction were simulated (6° and 10°) to be consistent with the clinical practice, and the aim of the study was to assess the accuracy of the system independently from the type of deformity to be corrected. Another limitation is that the pre-operative CT scan is performed in a not weight-bearing situation, which is very different from the “standard” clinical setting, with the planning performed on long-leg, weight-bearing X-rays. Considering the nature of this study (cadaveric study), simulating a weight-bearing condition was not possible. However, in the clinical setting a long-leg, weight-bearing x-rays can be added to the CT scan for a more precise pre-operative planning. Lastly, the reverse engineering process may be limited by the lack of screws, which may influence the precision of the personalized guide.
Conclusion
OWHTO is a widely performed procedure, with good outcomes if a careful pre-operative planning and accurate surgery are performed. Particularly, high accuracy on both coronal and sagittal plane are mandatory to achieve good outcomes. This study shows good accuracy for 3D pre-operative planning and PSCG in OWHTO, on both coronal and sagittal plane.
Availability of data and materials
Data are available at the corresponding author.
References
Amendola A, Bonasia DE (2010) Results of high tibial osteotomy: review of the literature. Int Orthop 34(2):155–160
Rosso F, Rossi R, Cantivalli A, Pilone C, Bonasia DE (2022) Joint Line Obliquity Does Not Affect the Outcomes of Opening Wedge High Tibial Osteotomy at an Average 10-Year Follow-up. Am J Sports Med 50(2):461–470
Noyes FR, Goebel SX, West J (2005) Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med 33(3):378–387
Nakayama H, Schröter S, Yamamoto C, Iseki T, Kanto R, Kurosaka K, Kambara S, Yoshiya S, Higa M (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 26(6):1873–1878
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 10(3):585–608
Martay JL, Palmer AJ, Bangerter NK, Clare S, Monk AP, Brown CP, Price AJ (2018) A preliminary modeling investigation into the safe correction zone for high tibial osteotomy. Knee 25(2):286–295
Elson DW, Petheram TG, Dawson MJ (2015) High reliability in digital planning of medial opening wedge high tibial osteotomy, using Miniaci’s method. Knee Surg Sports Traumatol Arthrosc 23(7):2041–2048
Sivertsen EA, Vik J, Meland ASV, Nerhus TK (2021) The Dugdale planning method for high tibial osteotomies underestimates the correction angle compared to the Miniaci method. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06663-z
El-Azab HM, Morgenstern M, Ahrens P, Schuster T, Imhoff AB, Lorenz SGF (2011) Limb alignment after open-wedge high tibial osteotomy and its effect on the clinical outcome. Orthopedics 34(10):e622-628
Kim MK, Ko BS, Park JH (2019) The proper correction of the mechanical axis in high tibial osteotomy with concomitant cartilage procedures—a retrospective comparative study. J Orthop Surg Res 14(1):281
Van den Bempt M, Van Genechten W, Claes T, Claes S (2016) How accurately does high tibial osteotomy correct the mechanical axis of an arthritic varus knee? A systematic review. Knee 23:925–935
Kim HJ, Yoon J-R, Choi GW, Yang J-H (2016) Imageless Navigation Versus Conventional Open Wedge High Tibial Osteotomy: A Meta-Analysis of Comparative Studies. Knee Surg Relat Res 28(1):16–26
Hasegawa M, Naito Y, Tone S, Sudo A (2021) High rates of outliers in computer-assisted high tibial osteotomy with excellent mid-term outcomes. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06788-1
Donnez M, Ollivier M, Munier M, Berton P, Podgorski J-P, Chabrand P, Parratte S (2018) Are three-dimensional patient-specific cutting guides for open wedge high tibial osteotomy accurate? An in vitro study. J Orthop Surg Res 13(1):171
Fucentese SF, Meier P, Jud L, Köchli G-L, Aichmair A, Vlachopoulos L, Fürnstahl P (2020) Accuracy of 3D-planned patient specific instrumentation in high tibial open wedge valgisation osteotomy. J Exp Orthop 7(1):7
Jud L, Fürnstahl P, Vlachopoulos L, Götschi T, Leoty LC, Fucentese SF (2020) Malpositioning of patient-specific instruments within the possible degrees of freedom in high-tibial osteotomy has no considerable influence on mechanical leg axis correction. Knee Surg Sports Traumatol Arthrosc 28(5):1356–1364
Miao Z, Li S, Luo D, Lu Q, Liu P (2022) The validity and accuracy of 3D-printed patient-specific instruments for high tibial osteotomy: a cadaveric study. J Orthop Surg Res 17(1):62
Nakamura R, Komatsu N, Fujita K, Kuroda K, Takahashi M, Omi R, Katsuki Y, Tsuchiya H (2017) Appropriate hinge position for prevention of unstable lateral hinge fracture in open wedge high tibial osteotomy. Bone Joint J 99-B(10):1313–1318
Rossi R, Bonasia DE, Amendola A (2011) The role of high tibial osteotomy in the varus knee. J Am Acad Orthop Surg 19(10):590–599
Murray R, Winkler PW, Shaikh HS, Musahl V (2021) High Tibial Osteotomy for Varus Deformity of the Knee. J Am Acad Orthop Surg Glob Res Rev 5(7):e21.00141
Ollivier B, Berger P, Depuydt C, Vandenneucker H (2021) Good long-term survival and patient-reported outcomes after high tibial osteotomy for medial compartment osteoarthritis. Knee Surg Sports Traumatol Arthrosc 29(11):3569–3584
Lee S-S, Kim JH, Kim S, Jung EY, Ryu DJ, Lee DK, Wang JH (2022) Avoiding Overcorrection to Increase Patient Satisfaction After Open Wedge High Tibial Osteotomy. Am J Sports Med 50(9):2453–2461
Marti CB, Gautier E, Wachtl SW, Jakob RP (2004) Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy 20(4):366–372
Jeong SH, Samuel LT, Acuña AJ, Kamath AF (2022) Patient-specific high tibial osteotomy for varus malalignment: 3D-printed plating technique and review of the literature. Eur J Orthop Surg Traumatol 32(5):845–855
Jones GG, Jaere M, Clarke S, Cobb J (2018) 3D printing and high tibial osteotomy. EFORT Open Reviews 3(5):254–259
Chaouche S, Jacquet C, Fabre-Aubrespy M, Sharma A, Argenson J-N, Parratte S, Ollivier M (2019) Patient-specific cutting guides for open-wedge high tibial osteotomy: safety and accuracy analysis of a hundred patients continuous cohort. Int Orthop 43(12):2757–2765
Mao Y, Xiong Y, Li Q, Chen G, Fu W, Tang X, Yang L, Li J (2020) 3D-Printed Patient-Specific Instrumentation Technique Vs. Conventional Technique in Medial Open Wedge High Tibial Osteotomy: A Prospective Comparative Study. Biomed Res Int 2020:1923172
Aman ZS, DePhillipo NN, Peebles LA, Familiari F, LaPrade RF, Dekker TJ (2022) Improved Accuracy of Coronal Alignment Can Be Attained Using 3D-Printed Patient-Specific Instrumentation for Knee Osteotomies: A Systematic Review of Level III and IV Studies. Arthroscopy 38(9):2741–2758
Grasso F, Martz P, Micicoi G, Khakha R, Kley K, Hanak L, Ollivier M, Jacquet C (2022) Double level knee osteotomy using patient-specific cutting guides is accurate and provides satisfactory clinical results: a prospective analysis of a cohort of twenty-two continuous patients. International Orthopaedics (SICOT) 46(3):473–479
Micicoi G, Corin B, Argenson J-N, Jacquet C, Khakha R, Martz P, Ollivier M (2022) Patient specific instrumentation allow precise derotational correction of femoral and tibial torsional deformities. The Knee 38:153–163
Pioger C, Mabrouk A, Siboni R, Jacquet C, Seil R, Ollivier M (2023) Double-level knee osteotomy accurately corrects lower limb deformity and provides satisfactory functional outcomes in bifocal (femur and tibia) valgus malaligned knees. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-023-07325-y
Abdelhameed MA, Yang CZ, AlMaeen BN, Jacquet C, Ollivier M (2022) No benefits of knee osteotomy patient’s specific instrumentation in experienced surgeon hands. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07288-6
Saragaglia D, Chedal-Bornu B, Rouchy RC, Rubens-Duval B, Mader R, Pailhé R (2016) Role of computer-assisted surgery in osteotomies around the knee. Knee Surg Sports Traumatol Arthrosc 24(11):3387–3395
Acknowledgements
Nothing.
Funding
The study was funded by Medacta International SA who provided the specimens, technology and implants.
Author information
Authors and Affiliations
Contributions
Conceptualization: Federica Rosso, Roberto Rossi. Methodology: Federica Rosso, Davide Edoardo Bonasia. Writing - original draft preparation: Federica Rosso, Davide Edoardo Bonasia. Writing - review and editing: Roberto Rossi, Sandro Fucentese, Philippe Neyret, Robert Śmigielski, Jacques Menetrey. Supervision: Sandro Fucentese.
Corresponding author
Ethics declarations
Declarations
Ethics approval and consent to participate
No ethical approval or informed consent was required.
Competing interest
• Roberto Rossi, MD is Payed teaching consultant for Arthrex, Zimmer-Biomet, Lima, Medacta, Smith and Nephew, De Puy.
• Davide Edoardo Bonasia, MD is a payed teaching consultant for Arthrex and Zimmer-Biomet, received editorial royalties for Elsevier and Springer and he is part of the editorial board “The Knee” journal, Elsevier.
• Philippe Neyret: consultant to Medacta, United Europe; founder of Surgical Training Program.
• Sandro Fucentese: Consultant Medacta, Storz, ZimmerBiomet.
• Federica Rosso received fees as consultant for manuscript writing from Medacta ®.
• The other authors have no financial or no-financial conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rosso, F., Rossi, R., Neyret, P. et al. A new three-dimensional patient-specific cutting guide for opening wedge high tibial osteotomy based on ct scan: preliminary in vitro results. J EXP ORTOP 10, 80 (2023). https://doi.org/10.1186/s40634-023-00647-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00647-3