Abstract
Background
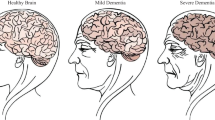
Alzheimer’s disease (AD) causes symptoms such as dementia, memory loss, disorientation, and even aggressiveness, and is more common in women than in men. AD may also manifest itself in changes in sleep patterns. However, the relationship between AD (in all stages) and bedtime behavior has not been thoroughly investigated.
Methods
In a prospective, cross-sectional survey, we evaluated 74 women categorized in two different stages of cognitive decline associated with AD (mild and severe) along with 37 women with no cognitive decline who served as controls. We obtained demographic and medical information such as age, health status, and medication, as well as psychiatrically confirmed staging of AD. We also collected actigraphy data for several nights in a row with a medical grade wristband using a 3-axis accelerometer and solid-state on-board memory. These data served as parameters for a clustering machine learning (ML) algorithm.
Results
The ML process was able to unsupervisedly identify 85% of the participants according to their pre-assigned degree of dementia. When the clustering was carried out in a binary fashion (i.e., only taking into account healthy members vs. severely affected AD patients), it was possible to correctly classify 91% of the cases.
Conclusions
This study revealed a strong connection between the severity of the intellectual decline and the features distilled from actigraphically derived sleep parameters.





Similar content being viewed by others
Data availability
We are in conversations with the National Sleep Research Resource (NSRR) to have our full dataset hosted in their repository. For now, data can be made available under demand by contacting the corresponding author of this paper.
References
Brown BM, Rainey-Smith SR, Villemagne VL, Weinborn M, Bucks RS, Sohrabi HR, Laws SM, Taddei K, Macaulay SL, Ames D et al (2016) The relationship between sleep quality and brain amyloid burden. Sleep 39(5):1063–1068
Buratti L, Viticchi G, Falsetti L, Cagnetti C, Luzzi S, Bartolini M, Provinciali L, Silvestrini M (2014) Vascular impairment in Alzheimer’s disease: the role of obstructive sleep apnea. J Alzheimers Dis 38(2):445–453
Kent BA, Mistlberger RE (2017) Sleep and hippocampal neurogenesis: implications for Alzheimer’s disease. Front Neuroendocrinol 45:35–52
Holth JK, Patel TK, Holtzman DM (2017) Sleep in Alzheimer’s disease–beyond amyloid. Neurobiol Sleep Circadian Rhythms 2:4–14
Winer JR, Mander BA (2018) Waking up to the importance of sleep in the pathogenesis of Alzheimer disease. JAMA Neurol 75(6):654–656
Irwin MR, Vitiello MV (2019) Implications of sleep disturbance and inflammation for Alzheimer’s disease dementia. Lancet Neurol 18(3):296–306
Sindi S, Kåreholt I., Johansson L, Skoog J, Sjöberg L, Wang H-X, Johansson B, Fratiglioni L, Soininen H, Solomon A et al (2018) Sleep disturbances and dementia risk: a multicenter study. Alzheimers Dement 14(10):1235–1242
FitzGerald JM, O’Regan N, Adamis D, Timmons S, Dunne CP, Trzepacz PT, Meagher DJ (2017) Sleep-wake cycle disturbances in elderly acute general medical inpatients: longitudinal relationship to delirium and dementia. Alzheimers Dement 7:61–68
Jung Y, Boot BP, Mielke MM, Ferman TJ, Geda YE, McDade E, Christianson TJ, Knopman DS, St Louis EK, Silber MH et al (2017) Phenoconversion from probable rapid eye movement sleep behavior disorder to mild cognitive impairment to dementia in a population-based sample. Alzheimers Dement 8(1):127–130
Benoit M, Berrut G, Doussaint J, Bakchine S, Bonin-Guillaume S, Frémont P, Gallarda T, Krolak-Salmon P, Marquet T, Mékiès C et al (2012) Apathy and depression in mild Alzheimer’s disease: a cross-sectional study using diagnostic criteria. J Alzheimers Dis 31(2):325–334
André C, Tomadesso C, de Flores R, Branger P, Rehel S, Mézenge F, Landeau B, de La Sayette V, Eustache F, Chételat G et al (2019) Brain and cognitive correlates of sleep fragmentation in elderly subjects with and without cognitive deficits. Alzheimers Dement 11:142–150
Rocca WA, Hofman A, Brayne C, Breteler MM, Clarke M, Copeland JR, Dartigues J-F, Engedal K, Hagnell O, Heeren TJ et al (1991) Frequency and distribution of Alzheimer’s disease in Europe: a collaborative study of 1980–1990 prevalence findings. Ann Neurol 30(3):381–390
Sierra-Sosa D, Arcila-Moreno J, Garcia-Zapirain B, Castillo-Olea C, Elmaghraby A Dementia prediction applying variational quantum classifier. arXiv:2007.08653
Reisberg B, Ferris S, de Leon MJ, Crook T The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry
Reisberg B, Jamil IA, Khan S, Monteiro I, Torossian C, Ferris S, Sabbagh M, Gauthier S, Auer S, Shulman MB et al (2011) Staging dementia. Principles and practice of geriatric psychiatry 3:162–169
Hebert LE, Scherr PA, Beckett LA, Albert MS, Pilgrim DM, Chown MJ, Funkenstein HH, Evans DA (1995) Age-specific incidence of Alzheimer’s disease in a community population. JAMA 273(17):1354–1359
Ferre A, Ribó M, Rodríguez-Luna D, Romero O, Sampol G, Molina C, Álvarez-Sabin J (2013) Strokes and their relationship with sleep and sleep disorders. Neurologí,a (English Edition) 28(2):103–118
Wei L, Wen Y-T, Thompson HJ, Liu C-Y, Su Y-K, Chen P-Y, Chen C-Y, Chuang Y-H, Lin Y-J, Chen C-T, Chen C-C, Chiu H-T, Chiu H-Y Sleep disturbances following traumatic brain injury in older adults: a comparison study. J Head Trauma Rehabil 35(4)
Monti JM, Monti D (2005) Sleep disturbance in schizophrenia. Int Rev Psychiatry 17(4):247–253
Vandeputte M, de Weerd A (2003) Sleep disorders and depressive feelings: a global survey with the Beck depression scale. Sleep Med 4(4):343–345
Lin W-Y, Verma VK, Lee M-Y, Lai C-S (2018) Activity monitoring with a wrist-worn, accelerometer-based device. Micromachines 9(9):450
Doherty A, Jackson D, Hammerla N, Plötz T, Olivier P, Granat MH, White T, Van Hees VT, Trenell MI, Owen CG et al (2017) Large scale population assessment of physical activity using wrist worn accelerometers: the UK Biobank Study. PloS One 12(2):e0169649
Stewart T, Narayanan A, Hedayatrad L, Neville J, Mackay L, Duncan S (2018) A dual-accelerometer system for classifying physical activity in children and adults. Med Sci Sports Exerc 50(12):2595–2602
Lima GZdS, Lopes SR, Prado TL, Lobao-Soares B, do Nascimento GC, Fontenele-Araujo J, Corso G (2017) Predictability of arousal in mouse slow wave sleep by accelerometer data. PloS One 12(5):e0176761
Walch O, Huang Y, Forger D, Goldstein C (2019) Sleep stage prediction with raw acceleration and photoplethysmography heart rate data derived from a consumer wearable device. Sleep 42(12):zsz180
Borazio M, Berlin E, Kücükyildiz N, Scholl P, Van Laerhoven K (2014) Towards benchmarked sleep detection with wrist-worn sensing units. In: International conference on healthcare informatics. IEEE, pp 125–134
Moon TK (1996) The expectation-maximization algorithm. IEEE Signal Proc Mag 13(6):47–60
Sharma N, Bajpai A, Litoriya MR (2012) Comparison the various clustering algorithms of Weka tools. Int J Emerg Technol Adv Eng 4(7):78–80
Verma NK, Dwivedi S, Sevakula RK (2015) Expectation maximization algorithm made fast for large scale data. In: IEEE (ed) Workshop on computational intelligence: theories, applications and future directions (WCI), pp 1–7
Fahim M, Fatima I, Lee S, Park Y-T (2013) EFM: evolutionary fuzzy model for dynamic activities recognition using a smartphone accelerometer. Appl Intell 39(3):475–488
El-Manzalawy Y, Buxton O, Honavar V (2017) Sleep/wake state prediction and sleep parameter estimation using unsupervised classification via clustering. In: Conference on bioinformatics and biomedicine. IEEE, pp 718–723
Willetts M, Hollowell S, Aslett L, Holmes C, Doherty A (2018) Statistical machine learning of sleep and physical activity phenotypes from sensor data in 96,220 UK Biobank participants. Sci Rep 8 (1):1–10
Ronning M (2002) A historical overview of the ATC/DDD methodology. WHO Drug Inf 16 (3):233
Crivello A, Barsocchi P, Girolami M, Palumbo F (2019) The meaning of sleep quality: a survey of available technologies, vol 7, pp 167374–167390
Sharma J, Kaur S (2017) Gerontechnology—the study of alzheimer disease using cloud computing. In: 2017 International conference on energy, communication, data analytics and soft Computing (ICECDS). IEEE, 3726–3733
Adrian M, Cooper J (1995) Biomechanics of human movement. Brown & Benchmark, Madison
Khalifa S, Hassan M, Seneviratne A (2013) Human activity recognition for indoor positioning using smartphone accelerometer, Tech. rep., School of Computer Science and Engineering University of South Wales
Susi M, Renaudin V, Lachapelle G (2013) Motion mode recognition and step detection algorithms for mobile phone users. Sensors 13(2):1539–1562
Wu C, Zhang F, Wang B, Liu KR, Au OC-L (2020) Method, apparatus, and system for wireless object tracking. US Patent App 16(/798):343
Mashita T, Shimatani K, Iwata M, Miyamoto H, Komaki D, Hara T, Kiyokawa K, Takemura H, Nishio S (2012) Human activity recognition for a content search system considering situations of smartphone users. In: 2012 IEEE virtual reality workshops (VRW). IEEE, pp 1–2
Batal I, Hauskrecht M (2009) A supervised time series feature extraction technique using DCT and DWT. In: International conference on machine learning and applications. IEEE, pp 735–739
Camargos EF, Louzada FM, Nóbrega OT (2013) Wrist actigraphy for measuring sleep in intervention studies with Alzheimer’s disease patients: application, usefulness, and challenges. Sleep Med Rev 17 (6):475–488
Ramzan M (2016) Comparing and evaluating the performance of Weka classifiers on critical diseases. In: India international conference on information processing (IICIP). IEEE, pp 1–4
Shree SB, Sheshadri H (2018) Diagnosis of Alzheimer’s disease using naive Bayesian classifier. Neural Comput and Applic 29(1):123–132
Meila M, Heckerman D. An experimental comparison of several clustering and initialization methods. arXiv:1301.7401
Ju Y-ES, McLeland JS, Toedebusch CD, Xiong C, Fagan AM, Duntley SP, Morris JC, Holtzman DM (2013) Sleep quality and preclinical alzheimer disease. JAMA Neurol 70(5):587–593
Acknowledgements
The authors would like to sincerely thank the following organizations and people for their commitment to this research work and for their kind, firm and faithful support from day one: C. Gombao and AFA Elda-Petrer (including its profoundly hard-working board of directors and dedicated staff); V. Gossage and D. Jackson from Axivity Ltd.; F. Portillo, L. Alted, Q. Maestre and Petrer’s council corporation; Santa Cruz church community (Petrer); M. Erades and CaixaPetrer; J. Tatay and J. Cortell from Kanteron Systems; B. Martínez, R. Miralles, A. Mairena, P. Marín, M. Manrique, C. Belando, S. Tarí and R. González from DomusVi Nursing Home; P. Camacho and J. Rico from La Molineta Retirement Home (part of the Lares association); E. Guerrero, V. Baún, M. Montoliu, L. Escalza and O. Peña from La Saleta Welfare Services for Elderly People; G. Ramiro; V. Medrano M.D; I. Montero; R. Martínez and A. Barceló. Finally, the authors would love to express their sincerest and most respectful gratitude towards all the participants in the present study, their corresponding families and caretakers.
Funding
This research is partially funded by Universidad Internacional de la Rioja (UNIR) through the Research Institute for Innovation & Technology in Education (UNIR iTED).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the all the involved institutions (both national and local), including retirement homes and cognitive stimulation centres, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Corbi, A., Burgos, D. Connection between sleeping patterns and cognitive deterioration in women with Alzheimer’s disease. Sleep Breath 26, 361–371 (2022). https://doi.org/10.1007/s11325-021-02327-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02327-x