Abstract
Introduction
Adequate sleep is fundamental to wellness and recovery from illnesses and lack thereof is associated with disease onset and progression resulting in adverse health outcomes. Measuring sleep quality and sleep apnea (SA) at the point of care utilizing data that is already collected is feasible and cost effective, using validated methods to unlock sleep information embedded in the data. The objective of this study is to determine the utility of automated analysis of a stored, robust signal widely collected in hospital and outpatient settings, a single lead electrocardiogram (ECG), using clinically validated algorithms, cardiopulmonary coupling (CPC), to objectively and accurately identify SA.
Methods
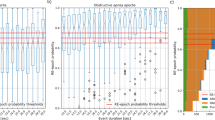
Retrospective analysis of de-identified PSG data with expert level scoring of Apnea Hypopnea Index (AHI) dividing the cohort into severe OSA (AHI > 30), moderate (AHI 15–30), mild (AHI 5–15), and no disease (AHI < 5) was compared with automated CPC analysis of a single lead ECG collected during sleep for each subject. Statistical analysis was used to compare the two methods.
Results
Sixty-eight ECG recordings were analyzed. CPC identified patients with moderate to severe SA with sensitivity of 100%, specificity of 81%, and agreement of 93%, LR+ (positive likelihood ratio) 5.20, LR− (negative likelihood ratio) 0.00 and kappa 0.85 compared with manual scoring of AHI.
Conclusion
The automated CPC analysis of stored single lead ECG data often collected during sleep in the clinical setting can accurately identify sleep apnea, providing medically actionable information that can aid clinical decisions.


Similar content being viewed by others
Abbreviations
- AASM:
-
American Academy of Sleep Medicine
- AHI:
-
Apnea Hypopnea Index
- CAP:
-
Cyclic alternating pattern
- CPC:
-
Cardiopulmonary coupling
- CPAP:
-
Continuous positive airway pressure
- CVD:
-
Cardiovascular disease
- CVHR:
-
Cyclic variation of heart rate
- EDR:
-
ECG-derived respiration
- ECG:
-
Electrocardiogram
- EEG:
-
Electroencephalogram
- eLFCBB :
-
Elevated low-frequency broad-band
- eLFCNB :
-
Elevated low-frequency narrow-band
- HRV:
-
Heart rate variability
- HFC:
-
High-frequency coupling
- LFC:
-
Low-frequency coupling
- NREM:
-
Non-rapid eye movement sleep
- non-CAP:
-
Non-cyclic alternating pattern
- PABAK:
-
Prevalence adjusted and bias adjusted kappa
- REM:
-
Rapid eye movement
- SAI:
-
Sleep Apnea Indicator
- SQI:
-
Sleep Quality Index
- VLFC:
-
Very low frequency coupling
References
Gallicchio L, Kalesan B (2009) Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 18:148–158. https://doi.org/10.1111/j.1365-2869.2008.00732.x2
Young T, Finn L, Peppard PE et al (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohorts. Sleep 31:1071–1078
Frost & Sullivan. Hidden Health Crisis Costing America Billions. American Academy of Sleep Medicine 2016 http://www.aasmnet.org/Resources/pdf/sleep-apnea-economic-crisis.pdf (assessed March 2017).
Peppard PE, Young TE, Barnet JH et al (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014. https://doi.org/10.1001/jama.2014.17822
Leung RS, Comodore VR, Ryan CM et al (2012) Mechanisms of sleep-disordered breathing: causes and consequences. Pflugers Arch 463(1):213–230. https://doi.org/10.1007/s00424-011-1055-x
Arnardottir ES, Bjornsdottir E, Olafsdottir KA, Benediktsdottir B, Gislason T (2016) Obstructive sleep apnea in the general population: highly prevalent but minimal symptoms. Eur Respir J 47(1):194–202. https://doi.org/10.1183/13993003.01148-2015
Beuters F, Reitzschel ER, Hertegonne KB, Chirinos JA (2016) The link between obstructive sleep apnea and cardiovascular disease. Curr Atheroscler Rep 18(1):1. https://doi.org/10.1007/s11883-015-0556-z
Khayat R, Pleister A (2016) Consequences of Obstructive Sleep Apnea: Cardiovascular Risk of Obstructive Sleep Apnea and Whether Continuous Positive Airway Pressure Reduces that Risk. Sleep Med Clin 11(3):273–286. https://doi.org/10.1016/j.jsmc.2016.05.002
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5(2):136–143. https://doi.org/10.1513/ats/200709-155MG.
Fu Y, X Xia Y, Yi H, Xu H, Guan J, Yin S (2017) Meta-analysis of all-cause and cardiovascular mortality in obstructive sleep apnea with or without continuous positive airway pressure treatment. Sleep Breath 21(1):181–189. https://doi.org/10.1007/s11325-016-1393-1
Peker Y, Glantz H, Eulenburg C, Wegscheider K, Herlitz J, Thunström E (2016) Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The RICCADSA randomized controlled trial. Am J Respir Crit Care Med 194(5):613–620. https://doi.org/10.1164/rccm.201601-0088OC
Costa SV, Ceolim MF (2013) Factors that affect inpatients’ quality of sleep. Rev esc enferm 47(1):46–52. https://doi.org/10.1590/S0080-62342013000100006
Elliott R, McKinley S, Cistulli P, Fien M (2013) Characterization of sleep in intensive care using 24-hour polysomnography: an observational study. Crit Care 17(2):R46. https://doi.org/10.1186/cc12565
Shear TC, Balachandran JS, Mokhlesi B, Spampinato LM, Knutson KL, Meltzer DO, Arora VM (2014) Risk of sleep apnea in hospitalized older patients. Journ Clin. Sleep Med 10(10):1061–1066. https://doi.org/10.5664/jcsm.4098
Lockhart EM, Willingham MD, Abdallah AB, Helsten DL, Bedair BA, Thomas J, Duntley S, Avidan MS (2013) Obstructive sleep apnea screening and postoperative mortality in a large surgical cohort. Sleep Med 14:407–415. https://doi.org/10.1016/j.sleep.2012.10.018
Mokhlesi B, Hovda MD, Vekhter B, Arora VM, Chung F, Meltzer DO (2013) Sleep disordered breathing and postoperative outcome after elective surgery: analysis of a nationwide inpatient sample. Chest 144:903–914. https://doi.org/10.1378/chest.12-2905
Kaula S, Keenan B, Goldberg L et al (2014) Diagnosis and treatment of sleep disordered breathing in hospitalized cardiac patients: a reduction in 30-day hospital readmission rates. Journ Clin. Sleep Med 10(10):1051–1059. https://doi.org/10.5664/jcsm.4096
Truong K, Jardin R, Massoudi N, Hashemzedeh M, Jafari B (2018) Nonadherence to CPAP associated with increased 30- day hospital readmissions. J Clin Sleep Med 14(2):1–7. https://doi.org/10.5664/jcsm.6928
Sharma S, Chowdhury A, Tang L, Willes L, Glynn B, Quan SF (2016) Hospitalized patients at high risk for obstructive sleep apnea have more rapid response system events and intervention is associated with reduced events. PLoS One 11:e0153790
Kapur VK, Auckley DH, Chowdhuri S (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of sleep medicine clinical practice guide. J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506
Chung F, Abdullah H, Liao P et al (2016) STOP-Bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest 149(3):631–638. https://doi.org/10.1378/chest.15-0903
Thomas RJ (2016) CardioPulmonary coupling sleep spectrograms. In: Kryger MH, Roth T, Dement WC (eds) Principles and practice of sleep medicine, 6th edn. Elsevier, Inc, Philadelphia, pp 1615–1623
Thomas RJ, Mietus JE, Peng CK, Guo D, Gozal D, Montgomery-Downs H, Gottlieb DJ, Wang CY, Goldberger AL (2014) Relationship between delta power and the electrocardiogram-derived cardiopulmonary spectrogram. Possible implications for assessing the effectiveness of sleep. Sleep Med 15(1):125–131. https://doi.org/10.1016/j.sleep.2013.10.002
Mietus JE, Peng CK, Ivanov PC, Goldberger AL (2000) Detection of obstructive sleep apnea from cardiac interbeat interval time series. Comput Cardiol 27:753–758. https://doi.org/10.1109/CIC200
Guilleminault C, Connolly S, Winkle R, Melvin K, Tilkian A (1984) Cyclical variation of the heart rate in sleep apnea syndrome: mechanisms, and usefulness of 24h electrocardiography as a screening technique. Lancet 1:126
Magnusdottir S, Hilmisson H (2017) Ambulatory screening tool for sleep apnea: analyzing a single-lead electrocardiogram (ECG). Sleep Breath; E-Pub September 22:421–429. https://doi.org/10.1007/s11325-017-1566-6
Lee WH, Hong SE, Kim HJ et al (2016) A Comparison of Different Success Definitions in Non-Continuous Positive Airway Pressure Treatment for Obstructive Sleep Apnea Using Cardiopulmonary Coupling. J Clin Sleep Med 1:35–41. https://doi.org/10.5664/jcsm.5388
Lee WH, Ahn JC, We J, Rhee CS, Lee CH, Yun PY, Yoon IY, Kim JW (2014) Cardiopulmonary coupling analysis: changes before and after treatment with mandibular advancement device. Sleep Breath 18(4):891–896. https://doi.org/10.1007/s11325-014-0961-5
Choi JH, Thomas RJ, Suh SY, Park IH, Kim TH, Lee SH, Lee HM, Yun CH, Lee SH (2015) Sleep quality changes after upper airway surgery in obstructive sleep apnea. Electrocardiogram-based cardiopulmonary coupling analysis. Laryngoscope 125(7):1737–1742. https://doi.org/10.1002/lary.25101
Schramm PJ, Thomas R, Feige B (2013) Et.al. Quantitative measurement of sleep quality using cardiopulmonary coupling analysis: a retrospective comparison of individuals with and without primary insomnia. Sleep Breath 17:713–721. https://doi.org/10.1007/s11325-012-0747-6
Thomas RJ, Wood C, Bianchi M (2018) Cardiopulmonary coupling spectrogram as an ambulatory clinical biomarker of sleep stability and quality in health, sleep apnea and insomnia. Sleep 41(2):1–11. https://doi.org/10.1093/sleep/zsx196
Goldberger AL, Amaral LAN, Glass L, Hausdorff JM, Ivanov PCH, Mark RG, Mietus JE, Moody GB, Penc CK, Stanley HE (2000) PhysioBank, PhysioToolkit and PhysioNet: components of a new research resource for complex physiologic signals. Circulation 101(23):e215–e220. https://doi.org/10.1161/01CIR10123.e215
Thomas RJ, Mietus JE, Peng CK et al (2007) Differentiation obstructive from central and complex sleep apnea using an automated electrocardiogram-based method. Sleep 30(12):1756–1759
Ancoli-Israel S (2009) Sleep and its disorders in aging populations. Sleep Med 10(Suppl 1):S7–S11. https://doi.org/10.1016/jsleep.2009.07.004
Thomas RJ, Weiss MD, Mietus JE et al (2009) Prevalent hypertension and stroke in the Sleep Heart Health Study: association with an ECG-derived spectrographic marker of cardiopulmonary coupling. Sleep 32(7):897–904
Pogach MS, Punjabi NM, Thomas N et al (2012) Electrocardiogram-based sleep spectrogram measures of sleep stability and glucose disposal in sleep-disordered breathing. Sleep 35:139–148. https://doi.org/10.5665/sleep.1604
Yang AC, Yang CH, Hong CJ et al (2011) Sleep state instabilities in major depressive disorder: Detection and quantification with electrocardiogram-based cardiopulmonary coupling analysis. Psychophysiology 48(2):285–291. https://doi.org/10.1111/j.1469-8986.2010.01060.x
Schramm PJ, Polland RE, Rao U et al (2014) Bupropion response on sleep quality in patients with depression: implications for increased cardiovascular disease risk. Eur Neuropsychopharmacol 24(2):207–214. https://doi.org/10.1016/j.euroneuro.2013.09.007
Yeh GY, Mietus JE, Peng CK et al (2008) Enhancement of sleep stability with Tai Chi exercise in chronic heart failure: preliminary findings using and ECG-based spectrogram method. Sleep Med 9(5):527–536. https://doi.org/10.1016/j.sleep.2007.06.003
Magalang UJ, Chen NH, Cistulli PA et al (2013) Agreement in the scoring of respiratory events and sleep among international sleep centers. Sleep 36:591–596. https://doi.org/10.5665/sleep.2552
Ho V, Crainiceanu C, Punjabi N et al (2015) Calibration model for apnea-hypopnea indices: impact of alternative criteria for hypopneas. Sleep 38(12):1887–1892. https://doi.org/10.5665/sleep.5234
Centers for Medicare and Medicate Services https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=227&ver=11&NcaName=Sleep+Testing+for+Obstructive+Sleep+Apnea+(OSA)&CoverageSelection=National&KeyWord=sleep+testing&KeyWordLookUp=Title&KeyWordSearchType=And&bc=gAAAACAAEAAA& (accessed Jan 2017)
StataCorp (2011) Stata statistical software: release 12. StataCorpLP, College Station
American Academy of sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22(5):667–689
Kapur V, Auckley D, Chowdhuri S et al (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506.
Penzel T, McNames J, Murray A et al (2002) Systematic comparison of different algorithms for apnoea detection based on electrocardiogram recordings. Med Biol Eng Comput 40(4):402–407
Varon C, Caicedo A, Testelmans D, Buyse B, van Huffel S (2015) A novel algorithm for the automatic detection of sleep apnea from single-lead ECG. IEEE Trans Biomed Eng 62(9):2269–2278. https://doi.org/10.1109/TBME.2015.2422378
Hayano J, Watanabe E, Saito Y, Sasaki F, Fujimoto K, Nomiyama T, Kawai K, Kodama I, Sakakibara H (2011) Screening for obstructive sleep apnea by cyclic variation of heart rate. Circ Arrythym Electrophysiol 4(1):64–72. https://doi.org/10.1161/CIRCEP.110.958009
Mendez MO, Cortbout J, van Huffel S, Matteucci M, Penzel T, Cerutti S, Bianchi AM (2010) Automatic screening of obstructive sleep apnea from the ECG based on empirical mode decomposition and wavelet analysis. Physiol Meas 31:273–289
Khandoker AH, Palaniswami M, Karmakar CK (2002) Support vector machines for automated recognition of obstructive sleep apnea syndrome from ECG recordings. Med Biol Eng Comput 40:402–407
Sforza E, Pichot V, Barthelemy JC, Haba-Rubio J, Roche F (2005) Cardiovascular variability during periodic leg movements: a spectral analysis approach. Clin Neurophysiol 116(5):1096–1104. https://doi.org/10.1016/j.clinph.2004.12.018
Gugisberg AG, Hess CW, Mathis J (2007) The significance of the sympathetic nervous system in the pathophysiology of periodic leg movements in sleep. Sleep 30:755–766. https://doi.org/10.1213/ane.0b013e318187c83a
McNicholas (2016) Continuous positive airway pressure therapy and cardiovascular outcomes in obstructive sleep apnoea syndrome: where are we now? J Thorac Dis 8(12):E1644–E1646. https://doi.org/10.21037/jtd.2016.12.36
Acknowledgements
Dr. Thomas Penzel of Philipps-University, Marburg, Germany who provided the data for this analysis, PhysioBank Database https://www.physionet.org/physiobank/database/apnea-ecg/(assessed November 2016).
Author information
Authors and Affiliations
Contributions
Neale Lange: Drafting and final approval of the manuscript.
Hugi Hilmisson: Analysis of data, initial drafting, and final approval of the manuscript.
Stephen P Duntley: Final approval of the manuscript.
Corresponding author
Ethics declarations
Formal consent was not required for this analysis, as the data had already been de-identified.
Conflict of interest
Lange, Neale, MD:
Assistant Clinical Professor of Medicine, University of Colorado Health Sciences Center, Denver, CO; Partner Critical Care Pulmonary and Sleep Associates.
Dr. Lange declares no conflict of interest.
Hilmisson, Hugi, MA works as a data Analyst, MyCardio LLC. SleepImage is the brand name of MyCardio LLC, a privately held entity. MyCardio LLC is a licensee of the CPC algorithm, a method using ECG recordings during sleep to phenotype sleep and sleep apnea, from the Beth Israel Deaconess Medical Center, Boston, MA, USA.
Stephen P Duntley, MD declares no conflict of interest.
Additional information
Data registry
The data is obtained from an open access research database https://physionet.org/physiobank/database/apnoea-ecg/ contributed by Dr. Thomas Penzel of Philipps-University, Marburg, Germany.
Rights and permissions
About this article
Cite this article
Hilmisson, H., Lange, N. & Duntley, S.P. Sleep apnea detection: accuracy of using automated ECG analysis compared to manually scored polysomnography (apnea hypopnea index). Sleep Breath 23, 125–133 (2019). https://doi.org/10.1007/s11325-018-1672-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1672-0