Abstract
Introduction
Many intensive care patients experience sleep disruption potentially related tonoise, light and treatment interventions. The purpose of this study was tocharacterise, in terms of quantity and quality, the sleep of intensive carepatients, taking into account the impact of environmental factors.
Methods
This observational study was conducted in the adult ICU of a tertiary referralhospital in Australia, enrolling 57 patients. Polysomnography (PSG) was performedover a 24-hour period to assess the quantity (total sleep time: hh:mm) and quality(percentage per stage, duration of sleep episode) of patients' sleep while in ICU.Rechtschaffen and Kales criteria were used to categorise sleep. Interrater checkswere performed. Sound pressure and illuminance levels and care events weresimultaneously recorded. Patients reported on their sleep quality in ICU using theRichards Campbell Sleep Questionnaire and the Sleep in Intensive CareQuestionnaire. Data were summarised using frequencies and proportions or measuresof central tendency and dispersion as appropriate and Cohen's Kappa statistic wasused for interrater reliability of the sleep data analysis.
Results
Patients' median total sleep time was 05:00 (IQR: 02:52 to 07:14). The majority ofsleep was stage 1 and 2 (medians: 19 and 73%) with scant slow wave and REM sleep.The median duration of sleep without waking was 00:03. Sound levels were high(mean Leq 53.95 dB(A) during the day and 50.20 dB(A) at night) and illuminancelevels were appropriate at night (median <2 lux) but low during the day(median: 74.20 lux). There was a median 1.7 care events/h. Patients' meanself-reported sleep quality was poor. Interrater reliability of sleep staging washighest for slow wave sleep and lowest for stage 1 sleep.
Conclusions
The quantity and quality of sleep in intensive care patients are poor and may berelated to noise, critical illness itself and treatment events that disturb sleep.The study highlights the challenge of quantifying sleep in the critical caresetting and the need for alternative methods of measuring sleep. The resultssuggest that a sound reduction program is required and other interventions toimprove clinical practices to promote sleep in intensive care patients.
Trial registration
Australian New Zealand clinical trial registry(http://www.anzctr.org.au/): ACTRN12610000688088.
Similar content being viewed by others
Introduction
The role of good quality sleep in health is well known [1, 2]. However, many critically ill patients treated in the intensive care unit(ICU) experience sleep disruption [3–6]. Intensive care patients may experience normal or near-normal total sleeptime (TST) but have been reported to have reduced slow wave (SW) and rapid eye movement(REM) sleep, largely because of frequent arousals. The factors causing sleep disruptionin intensive care patients are not fully understood; many extrinsic and intrinsicfactors have been proposed, such as noise [7], light, inflammatory mediators [6], sedative and opioid medications [4] and mechanical ventilator settings [8]. Polysomnography (PSG) recording is supported by reports from ICU patients ontheir inability to sleep well in ICU [9, 10]. Patients often attribute disturbances to their sleep to noise levels [10].
Twenty-four hour PSG studies in ICU have been few and there are no recent studies; therehave been fewer studies still examining the prevalence of sleep disruptive factorssimultaneously with PSG or investigations of ICU patient perceptions of the quality ofsleep and sleep disruptions in conjunction with PSG recording. The primary aim of thisobservational study was to provide a current assessment of the quality and quantity ofcritically ill patients' sleep while they were treated in ICU. The secondary aims wereto explore the prevalence of the main factors that potentially affect sleep in ICU, thatis the environmental sound pressure and illuminance levels ICU patients are exposed to,and the frequency of treatment and care patients receive. We also assessed self-reportedsleep quality while patients were treated in ICU and the hospital ward and patients'perceptions of sleep disruptions in ICU.
Materials and methods
Study setting and sample
This study was conducted in a 36-bed adult general ICU in a 600-bed hospital inSydney, Australia. The ICU provided specialty services such as cardiac, spinal, burnsand renal and was a closed unit with an accredited intensivist responsible for themanagement of all patients. Ward rounds were conducted by the intensivist twice a daywhen treatment goals/plans were reviewed, for example sedation medicationprescriptions were adjusted according to the individual patient needs (routinely,calm and interactive). The registered nurse (RN) to patient ratio was 1:1 formechanically ventilated patients and 1:2 for patients requiring high dependency care.There was no distinct area for the care of high dependency level patients;mechanically ventilated patients were cared for alongside patients of lower acuity.The RN performed all the nursing care for the patient. The main practices associatedwith sleep promotion during the time in which the study was conducted were offering anight-time hypnotic (that is, temazepam) and earplugs/eye shades to the patients anddimming the main lights at night.
Patients were included if aged >16 years and likely to be treated in ICU for >24hours and able to give informed consent on their own behalf. The ability to provideconsent was assessed by the following means: i) subjective advice by the bedsidenurse; cognition was discussed including orientation to time and place and ability tofollow simple instructions; ii) the patient was approached and asked to state theirname (or mouth the words); if the patient was able to perform this instruction afurther check was made; iii) the patient's understanding and ability to followinstructions was checked by asking them to nod when the correct colour card was heldup from a selection of three. Exclusion criteria included a history of sleepdisorders, psychiatric illness requiring medication, a known diagnosis of dementia orcentral neurological impairment confirmed by radiological scan. Human Research EthicsCommittee approval for the study was provided by the Health Service and theUniversity of Technology Sydney. Patients provided informed consent with writtenconfirmation by their next of kin in cases where the patient was unable to sign theconsent form. Data were collected from January to December, 2009 and September 2010to April 2011. Screening for eligibility was performed on weekdays.
Data collection
On enrolment, patients rated their sleep quality prior to hospitalization using a 1to 10 scale (10 = excellent) and patients or their proxy completed the InsomniaSeverity Index (ISI) [11]. The ISI comprises seven items based on the symptoms and severity of sleepdisturbance; each item is scored from 0 (not at all) to 4 (extremely). The total ISIscore ranges from 0 to 28 with a cutoff for clinical insomnia of 15. Concurrentvalidity with a sleep diary has been reported at r = 0.65 [11].
Patients were monitored for one 24-hour period using a portable PSG device, eitherPS-2™ (Compumedics, Melbourne, Australia) or ALICE LE™ (PhilipsRespironics, Amsterdam, Netherlands). Recording began and finished between 1000 and1700 hours. Electroencephalograph (EEG) (O1/M2, C4/M1), electromyograph (EMG),electrooculograph (EOG) (right and left) and electrocardiograph (ECG) (lead II) wererecorded. Patients' skin was prepared according to standard techniques. Gold cup EEGelectrodes were placed at O1/M2 and C4/M1 according to the International 10-20 System [12]. Two EOG electrodes were used for right and left eye movements. The EMGelectrodes were located over the right and left masseter (facial) muscles. Electrodeapplication was performed by the authors (RE and MF) who were both trained in thetechnique. Electrode impedance was maintained <9,000 ohms. Visual checks wereperformed hourly and electrodes were replaced if impedance values approached 9,000ohms or when the patient was disturbed for routine repositioning.
Sound and illuminance levels were recorded simultaneously with PSG using theintegrated sound pressure level meter (model 2250, Brüel and Kjaer™,Nærum, Denmark) and illuminance level meter (T-10, Konica Minolta™, Osaka,Japan). Continuous equivalent sound pressure levels (Leq) in 'A' weighted decibelsand peak sound pressure levels (Lpeak) in 'C' weighted decibels were logged everysecond. More detailed information about the protocol for sound pressure levelrecording and configuration of patient rooms is reported elsewhere [13]. Illuminance level (in lux) was recorded, using a sensor placed close tothe patient's head, once per minute. The bedside nurse was requested to log an eventwhenever the patient received treatment or care using a specially designed MicrosoftAccess™ (Microsoft, Redmond, WA, USA) form listing a number of events on acomputer located within reach. The event log contained the following items: clinicalassessment; tracheal suctioning; pressure area care; physiotherapy; mouth/eye care;blood test (sampling); wash; non-invasive blood pressure; eating and drinking;dressing; pain; line insertion; X-ray; clinical crisis; agitation/anxiety/confusion;electrode replacement and other (for example placing an extra blanket on thepatient).
On completion of PSG recording patients rated their previous night's sleep using theRichards Campbell Sleep Questionnaire (RCSQ) [14]. The RCSQ contains five 100mm visual analogue scales (VAS): sleep depth,latency, awakenings, time awake and quality of sleep (higher scores indicate bettersleep). The RCSQ was pilot tested in a medical ICU [15] and validated with overnight PSG in medical ICU patients [14]. In our study, patients who were unable to write were assisted; thepatient used their current communication strategy to indicate where the investigatorshould mark the VAS.
One to two nights after transfer to the ward, patients rated their sleep on the wardusing the RCSQ and reported on sleep-disturbing factors in ICU using the Sleep inIntensive Care Questionnaire (SICQ) [10]. The SICQ was developed to determine the perceived effect of the ICUenvironment on sleep. It contains seven questions (rated 1 to 10), including overallsleep quality at home, sources of perceived sleep disruption and sources ofnoise.
Demographic and clinical data were collected from the patient's record. The AcutePhysiology and Chronic Health Evaluation (APACHE) III modified diagnostic codes [16] were used to classify diagnoses. The APACHE II severity of illness scoreon admission and the Modified Sequential Organ Failure Assessment (SOFA) [17] at the time of enrolment were calculated to assess severity ofillness.
Data analysis
Polysomnography recordings were scored manually in 30-second epochs, by threequalified sleep technologists using standard Rechtschaffen and Kales [18] (R and K) criteria. TST was defined as the time spent in all sleep stages.The percentage of time in each sleep stage and sleep during the day (0600 to 2100hours) was calculated. Arousals were defined using American Academy of Sleep Medicinecriteria [19] and the number per hour of sleep (arousal index) reported. Morphineequivalent doses of opioid medications [20] and midazolam equivalent doses of benzodiazepine [21] were calculated to summarise the doses of opioid and sedative medicationsadministered.
The software packages PASW™ (version 18; SPSS Inc, Chicago, IL, USA) andMicrosoft Excel (2007) were used to analyse the data. Means and medians were used todescribe continuous data and frequencies and percentages were used for categoricaldata. Interrater reliability for scoring the PSG data by sleep technologists wasperformed on 16 (30%) recordings using Cohen's Kappa statistic. The Mann-Whitney Utest was used to detect differences between the TST and arousal indices for patientswho received mechanical ventilation during PSG and those who did not and to comparearousal indices for patients who received benzodiazepine medications or propofol andthose who did not. The correlation between arousal indices and peak sounds (>80dB(A)) was explored using Pearson's r. Wilcoxon signed ranks test was used to comparepatients' self-reported quality of sleep in ICU and the ward.
Results
Sample characteristics
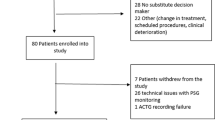
During the study twenty-four hour PSG data were analysed for 53 patients and 47patients were followed up on the ward. Of 266 eligible patients 57 were enrolled; ofthose not enrolled 74 declined participation and 135 were transferred to the wardbefore they could be invited to participate. Two patients requested removal of PSGafter recording began, palliation was initiated for another and data for another wasunable to be analysed. Figure 1 provides a flow diagram of thenumber of eligible patients and the number invited to participate and enrolled. Thecharacteristics of patients enrolled in the study are provided in Table 1. Admission diagnoses were mostly non-operative (66%), meanAPACHE II score was 18.70 (SD: 8.23) and the mean SOFA score was 4.04 (SD: 2.53).Patients were interactive and calm (mean Vancouver Interaction Scale (VICS) [22] score: 27.06 (SD: 3.80) (equivalent to 0 or -1 on the Richmond AgitationSedation Scale (RASS) [23]).
Prevalence of eligible patients. Number of patients admitted toICU during the time period in which the study was conducted, eligible for thestudy, enrolled and completing 24-hour polysomnography (PSG) monitoring andsleep questionnaires on the hospital ward. aEnrolment ofeligible patients was limited by the availability of only one PSG and oneresearcher for the entire 24-hour recording period.
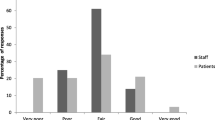
Twenty-one percent of patients reported a pre-hospital ISI score of ≥15,indicating moderate to severe clinical insomnia, however, median pre-hospitalisationsleep quality on the SICQ was 8.00 out of 10.00. There was no difference between themean RCSQ score in ICU and on the ward (P = 0.61). Noise was rated thehighest sleep-disturbing factor (Table 2).
Sleep, sound and light
Median TST was five hours (Figure 2). The median duration ofsleep without waking was 00:03 (hh:mm). Unusual sleep stage transitions were noted(for example progression from stage 1 to REM sleep). Daytime sleep comprised 41% ofTST and EEG delta wave activity was observed when patients were interactive andapparently awake. The majority of sleep was stages 1 and 2 (19 and 73 %,respectively). SW and REM sleep was scant (median (IQR) 0 (0 to 1) and 0 (0 to 6)respectively). Arousals were frequent (median arousal index: 27) (Table 3). Interrater reliability of the sleep technologists' PSGanalysis for sleep/awake was 0.58 to 0.68 (Table 4).
Sound pressure levels were high (mean Leq 53.95 (SD: 2.33) dB(A) during the day and50.20 (SD: 3.21) dB(A) at night). There were a median 416/h sound peaks >80 dB(C)during the day and 90/h at night. The correlation between arousal indices and numberof sound peaks >80 dB(A) was weak during the day (r = 0.13) and night (r = 0.19);neither was statistically significant. Median illuminance levels were lower at night(1.74 lux) than during the day (74.20 lux). The average number of care events was1.74/h; the lowest was between 0200 and 0500 hours (<1.00/h). No patients wore earplugs or eye shades during sleep monitoring.
Sleep mechanical ventilation and medications
Pressure support was the ventilation mode used for 26 patients (six patients receivedpressure control ventilation (PCV) for periods during pressure support), one patientreceived synchronised intermittent ventilation (SIMV) and another patient receivedPCV. Twelve patients were extubated (that is, had their endotracheal tube removed)during PSG monitoring. The median TST of patients who received mechanical ventilationduring PSG recording and those who did not was 05:14 (IQR: 03:36 to 07:57) vs. 03:57(IQR: 01:39 vs. 06:47; P = 0.049) and median arousal indices (20.50 IQR:11.50 to 32.5 vs. 29.50 IQR: 22.00 to 40.87, P = 0.018). The differences forother sleep parameters did not reach statistical significance for patients whoreceived mechanical ventilation during PSG recording and those who did not (forexample, stage 1: 22.87 (24.13) vs. 27.54 (19.85) %, stage 2: 69.99 (24.02) vs. 67.30(20.17) % and REM: 4.47 (5.90) vs. 2.38 (4.91) %).
The mean equivalent dose of morphine was 12.46 (SD: 24.42) mcg/kg/h and equivalentdose of midazolam was 2.26 (SD: 11.60) mcg/kg/h. Six patients received temazepam(four received 20mg and two 10mg) for night sedation. There was a difference in themedian arousal indices for patients who received benzodiazepine medication/propofoland those who did not (22.00 IQR: 11.25 to 31.75 vs. 30.00 IQR: 20.75 to 40.75; P = 0.019). The differences for other sleep parameters did not reach statisticalsignificance for patients who received benzodiazepine medication/propofol and thosewho did not (for example, stage 1: 26.41 (20.74) vs. 23.71 (23.75) %, stage 2: 67.42(19.38) vs. 69.97 (24.74) % and REM: 2.85 (4.76) vs. 4.14 (6.16) %).
Discussion
This study provides a current characterisation of the quality and quantity of sleep inintensive care patients, together with factors that potentially affect the sleep ofpatients in ICU. Sleep quality was poor; over 90% of patients' sleep was stage 1 and 2and TST was below that experienced by healthy adults. These results indicate that therehas been no improvement since studies published between 1976 and 2003 [3, 5, 24–26], despite improvements in ICU design, technology and health care personneltraining. Sleep fragmentation and unconventional architecture was evident with multipleshort, non-contiguous sleep periods and numerous arousals. Arousals were frequent, aswell as non-sequential stage changes [4, 27]. A large percentage of TST was during daytime hours
Sound levels were elevated and exceeded World Health Organization (WHO) standards forhospitals, that is Leq should not >35 dB(A) in patient areas [28]. In our study, Leq was >49 dB(A). Continuous equivalent sound pressure levelswere 10 dB(A) lower than in many studies in ICU [5, 29, 30] but similar to others [26, 31]. The frequency of sound peaks >80 dB(C) was notable (range: 31 to 1,436/h)and high in comparison with other studies. Kahn et al. [32] reported a mean of 56/h before a noise reduction program and 40/h afterwards,while the mean reported by Meyer et al. [33] was 60/h. It is somewhat surprising that there was no correlation betweenarousal indices and the number of sound peaks >80 dB(A), although it is possible thatpatients had become accustomed to high sound levels. Illuminance levels were appropriateat night (median <2 lux). However, daytime illuminance levels (74 lux) may have beentoo low to encourage a 24-hour circadian rhythm. Study of endogenous melatonin secretionin healthy participants indicates that illuminance levels of <100 lux may not besufficiently bright to suppress melatonin secretion in some individuals [34]. Thus patients in our study may have had high melatonin levels during the daythat contributed to the proportion of daytime sleep. The mean number of treatment/careevents was 40 (1.7/h). This contrasts with hourly rates reported by others (for example3, 7 and 6/h) [6, 25, 26]. Under-recording by the bedside nurses may have occurred in our study. Whilean attempt was made to record care events/treatment in a synchronous manner, this proveddifficult in practice. Hence we are unable to draw conclusions about the relationshipbetween such events and arousals.
Medications administered and considered to potentially affect sleep noted during PSGrecording were mainly opioids and sedative medications. A large proportion (60%) ofpatients received opioid medications, potentially affecting their sleep. SWS has beenfound to be reduced by opioids, with a concomitant increase in stage 2 sleep [35]. A large percentage of patients in our study received benzodiazepines orpropofol (53%) (however, only lightly sedated patients were enrolled; the mean VICSscore was 27.06 (SD: 3.80)). This may also have contributed to the high proportion ofstage 2 and lack of REM sleep [36]. However, it is notable that patients who received benzodiazepine medicationor propofol had fewer arousals than patients who did not. Despite the apparentsuppression of SWS and REM, sleep may have been more consolidated when sedativemedications were administered. The somewhat surprising findings that TST was higher andthere were fewer arousal indices in patients who received mechanical ventilation duringPSG recording may be partly attributable to the larger sedative medication doses theyreceived (mean: 3.49 (SD: 15.64) vs. 0.40 (SD: 0.75) mcg/kg/h).
Patients' self-reports of sleep quality in ICU were poor but comparable to previousstudies. The mean RCSQ score from patients ready for transfer to the ward in the sameICU (n = 222) was 47.18 mm [37]. In a study investigating the utility of the RCSQ and concordance of nurseand patient sleep assessment in ICU, the mean RCSQ score was 45.50 mm [38].
Patient perceptions of sources of sleep disruption were similar to previous studies.Noise was rated the most disruptive, as has been reported elsewhere [26]. In the development of the SICQ, ratings of disruptive activities were lowerand noise (4.5) was less disruptive than vital signs (5.5) and phlebotomy (5.5) [10]. However, the SICQ was first reported in 1999; non-invasive vital signsmonitoring and blood sampling in the current study would be expected to be lessdisruptive than techniques in use in the 1990s.
Study strengths and limitations
This study is the largest of its kind to be conducted using PSG with simultaneousdata collection for factors known to affect sleep in ICU and is the first to presentdata from the Australian context. In addition, other investigators have rarelycollected data on the patients' perception of sleep quality and potentialsleep-disrupting factors in conjunction with PSG recording. This subjectiveinformation is vital in corroborating objective data, particularly as sleep is asubjective experience.
A limitation that became evident during the study was the difficulty in interpretingthe PSG data using conventional R and K analysis. One patient's EEG waveform wasaffected with 'alpha intrusion' (alpha wave activity superimposed on delta waves),which made analysis impossible (the likely explanation being the administration ofantipsychotic medications after enrolment/PSG recording began). Observation of EEGdelta wave activity in some patients who appeared to be awake has been noted in otherstudies [4, 5, 39]. Challenges in scoring ICU patients' sleep data were recently reported byDrouot et al. [39] in their analysis of PSG data from two studies conducted previously. Theinvestigators noted the presence of EEG delta wave activity during apparentwakefulness (the presence of EMG, EOG and limb activity) and a lack of K complexesand sleep spindles preventing classification of stage 2. However, interrater andintrarater scorer reliability checks were not performed in that study.
Another limitation is the effect of benzodiazepine medications on the interpretationof sleep parameters. It is known that benzodiazepine medication increases EEG betawave activity and reduces EEG delta wave activity [40]. Benzodiazepine medication also increases EEG spindle activity [41] (though this appears not to have been the case in our study). The combinedeffect of the opioids and sedative medication on EEG activity likely affected theresults. However, since these medications are essential adjuncts in the treatment andcomfort of many ICU patients, excluding patients who received them would haveseverely limited recruitment and the generalisability of our results. Otherlimitations were the presence of factors such as the use of different modes ofmechanical ventilation and health conditions such as systemic inflammatory response,but such factors are common in ICU patients and their exclusion would also limit theapplicability of the results to the ICU patient population.
Patient enrolment was limited by a number of factors. The availability of PSGmonitoring equipment and the principal researcher were the primary factors forpatients being discharged before they were approached to participate. For this study,we had access to only two people trained in sleep recordings (RE and MF) and oneportable sleep-monitoring device, creating practical limitations to the number andfrequency of studies performed. In addition, there was often limited opportunity inwhich patients were cognitively able to agree to participate before they weredischarged to the hospital ward. A large proportion of patients approached about thestudy declined to participate; many considered the application of monitoring as aset-back in their condition regardless of the reason for it. This may limit thegeneralisability of the results to a sub-set of patients treated in the studyICU.
Interrater reliability of the R and K analysis was moderate, 0.56 for sleeptechnologists one and two and 0.51 for sleep technologists two and three but lowerthan Kappa values for sleep technologists in sleep investigation units (for example0.72 [42]). Interrater reliability for each stage was also lower than in sleeplaboratory studies. The reliability of PSG analysis in ICU patients has beeninfrequently reported. In one study of critically ill, non-ventilated traumapatients' night-time sleep, interrater reliability for one overnight recording, wasreported as Kappa = 0.82 [43]. However, in a comparison by Ambrogio et al. of four methods ofanalysing ICU patients' PSG data, interrater reliability was considerably lower thanin the present study (Kappa = 0.19) [44].
Conclusions
The quantity and quality of patients' sleep while in this ICU using both objective andsubjective assessment methods were found to be poor. Given the similarity between thesleep outcomes and prevalence of potential sleep-disturbing factors in our study andprevious studies, sleep disruption clearly remains a substantial problem for many ICUpatients. Importantly, the current study has added to evolving knowledge of thechallenges of using PSG in ICU and analysing the data. An alternative objective sleepassessment method is required for ICU patients in order to further our understanding ofsleep disruption in this vulnerable patient population and to test clinicalinterventions for their well-being and recovery.
Key messages
·Sleep in ICU patients is highly fragmented with concomitant deficiencies in SW andREM sleep.
·Use of PSG in ICU patients and analysing the data are challenging.
·There is a need to develop alternative methods to conventional PSG staging tomeasure sleep in ICU patients and develop interventions which will improve sleep.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- ECG:
-
electrocardiograph
- EEG:
-
electroencephalograph
- EMG:
-
electromyograph
- EOG:
-
electrooculograph
- ICU:
-
intensive careunit
- ISI:
-
Insomnia Severity Index
- Leq:
-
equivalent sound pressure levels
- Lpeak:
-
peaksound pressure levels
- PCV:
-
pressure control ventilation
- PSG:
-
polysomnography
- R and K:
-
Rechtschaffen and Kales
- RASS:
-
Richmond Agitation Sedation Scale
- RCSQ:
-
Richards-Campbell Sleep Questionnaire
- REM:
-
rapid eye movement
- RN:
-
registered nurse
- SICQ:
-
Sleep in Intensive Care Questionnaire
- SIMV:
-
synchronised intermittentventilation
- SOFA:
-
Sequential Organ Failure Assessment
- SWS:
-
slow wave sleep
- TST:
-
totalsleep time
- VAS:
-
visual analogue scale
- VICS:
-
Vancouver Interaction Scale.
References
Gallicchio L, Kalesan : Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 2009, 18: 148-158. Epub 2009 Aug 4 10.1111/j.1365-2869.2008.00732.x
Grandner MA, Hale L, Moore M, Patel NP: Mortality associated with short sleep duration: the evidence, the possiblemechanisms, and the future. Sleep Med Rev 2010, 14: 191-203. Epub 2009 Nov 26 10.1016/j.smrv.2009.07.006
Aurell J, Elmqvist D: Sleep in the surgical intensive care unit: continuous polygraphic recording ofsleep in nine patients receiving postoperative care. Br Med J (Clin Res Ed) 1985, 290: 1029-1032. Epub 1985 Apr 6 10.1136/bmj.290.6474.1029
Cooper AB, Thornley KS, Young GB, Slutsky AS, Stewart TE, Hanly PJ: Sleep in critically ill patients requiring mechanical ventilation. Chest 2000, 117: 809-818. Epub 2000 Mar 14 10.1378/chest.117.3.809
Freedman NS, Gazendam J, Levan L, Pack AI, Schwab RJ: Abnormal sleep/wake cycles and the effect of environmental noise on sleepdisruption in the intensive care unit. Am J Respir Crit Care Med 2001, 163: 451-457. Epub 2001 Feb 17 10.1164/ajrccm.163.2.9912128
Hardin KA, Seyal M, Stewart T, Bonekat HW: Sleep in critically ill chemically paralyzed patients requiring mechanicalventilation. Chest 2006, 129: 1468-1477. Epub 2006 June 17 10.1378/chest.129.6.1468
Aaron JN, Carlisle CC, Carskadon MA, Meyer TJ, Hill NS, Millman RP: Environmental noise as a cause of sleep disruption in an intermediate respiratorycare unit. Sleep 1996, 19: 707-710.
Bosma K, Ferreyra G, Ambrogio C, Pasero D, Mirabella L, Braghiroli A, Appendini L, Mascia L, Ranieri VM: Patient-ventilator interaction and sleep in mechanically ventilated patients:pressure support versus proportional assist ventilation. Crit Care Med 2007, 35: 1048-54. Epub 2007 March 6 10.1097/01.CCM.0000260055.64235.7C
Nicolas A, Aizpitarte E, Iruarrizaga A, Vazquez M, Margall A, Asiain C: Perception of night-time sleep by surgical patients in an intensive care unit. Nurs Crit Care 2008, 13: 25-33. Epub 2008 Jan 30 10.1111/j.1478-5153.2007.00255.x
Freedman NS, Kotzer N, Schwab RJ: Patient perception of sleep quality and etiology of sleep disruption in theintensive care unit. Am J Respir Crit Care Med 1999, 159: 1155-1162. Epub 1999 Apr 8 10.1164/ajrccm.159.4.9806141
Bastien CH, Vallieres A, Morin CM: Validation of the Insomnia Severity Index as an outcome measure for insomniaresearch. Sleep Med 2001, 2: 297-307. Epub 2001 July 5 10.1016/S1389-9457(00)00065-4
Jasper HH: Report of the committee on methods of clinical examination inelectroencephalography: 1957. Electroencephalogr Clin Neurophysiol 1958, 10: 370-375.
Elliott RM, McKinley SM, Eager D: A pilot study of sound levels in an Australian adult general intensive careunit. Noise Health 2010, 12: 26-36. Epub 2010 Feb 18 10.4103/1463-1741.59997
Richards KC, O'Sullivan PS, Phillips RL: Measurement of sleep in critically ill patients. J Nurs Meas 2000, 8: 131-144. Epub 2001 Mar 3
Richards KC, Bairnsfather L: A description of night sleep patterns in the critical care unit. Heart Lung 1988, 17: 35-42. Epub 1988 Jan 1
Australian and New Zealand Intensive Care Society: Appendix C: ICU Diagnosis APACHE III. ANZICS Adult patient database data dictionary 2004, 95-97.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG: The SOFA (Sepsis-related Organ Failure Assessment) score to describe organdysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems ofthe European Society of Intensive Care Medicine. Intensive Care Med 1996, 22: 707-710. Epub 1996 July 1 10.1007/BF01709751
Rechtschaffen A, Kales A: A manual of standardized terminology: techniques and scoring system for sleepstages of human subjects. Los Angeles: UCLA Brain Information Service/Brain ResearchInstitute; 1968.
Iber C, Ancoli-Israel S, Chesson A, Quan SF: AASM manual for the scoring of sleep and associated events: rules, terminologyand technical specification. 1st edition. Edited by: Iber C, Ancoli-Israel S, Chesson A, Quan SF. Westchester: American Academy of Sleep Medicine; 2007.
Ballantyne J, Bonica JJ, Fishman S: Bonica's management of pain. 4th edition. Edited by: Fishman SM, Ballantyne JC, Rathmell JP. Philadelphia: Lippincott Williams & Wilkins; 2009.
Ashton CH: Guidelines for the rational use of benzodiazepines. Drugs 1994, 48: 25-40. 10.2165/00003495-199448010-00004
de Lemos J, Tweeddale M, Chittock D: Measuring quality of sedation in adult mechanically ventilated critically illpatients: the Vancouver Interaction and Calmness Scale. J Clin Epidemiol 2000, 53: 908-919. 10.1016/S0895-4356(00)00208-0
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK: The Richmond Agitation-Sedation Scale: validity and reliability in adult intensivecare unit patients. Am J Respir Crit Care Med 2002, 166: 1338-1344. Epub 2002 Nov 15 10.1164/rccm.2107138
Edell-Gustafsson UM, Hetta JE, Aren CB: Sleep and quality of life assessment in patients undergoing coronary artery bypassgrafting. J Adv Nurs 1999, 29: 1213-1220. Epub 1999 May 13 10.1046/j.1365-2648.1999.01006.x
Hilton BA: Quantity and quality of patients' sleep and sleep-disturbing factors in arespiratory intensive care unit. J Adv Nurs 1976, 1: 453-468. Epub 1976 Nov 1 10.1111/j.1365-2648.1976.tb00932.x
Gabor JY, Cooper AB, Crombach SA, Lee B, Kadikar N, Bettger HE, Hanly PJ: Contribution of the intensive care unit environment to sleep disruption inmechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med 2003, 167: 708-715. Epub 2003 Feb 25 10.1164/rccm.2201090
Friese RS, Diaz-Arrastia R, McBride D, Frankel H, Gentilello LM: Quantity and quality of sleep in the surgical intensive care unit: are ourpatients sleeping? J Trauma 2007, 63: 1210-1214. Epub 2008 Jan 24 10.1097/TA.0b013e31815b83d7
Berglund B, Lindvall T: Guidelines for community noise. Geneva, Switzerland: World Health Organization; 1999.
Wallace CJ, Robins J, Alvord LS, Walker JM: The effect of earplugs on sleep measures during exposure to simulated intensivecare unit noise. Am J Crit Care 1999, 8: 210-219. Epub 1999 July 7
Hilton BA: Noise in acute patient care areas. Res Nurs Health 1985, 8: 283-291. Epub 1985 Sept 1 10.1002/nur.4770080311
Blomkvist V, Eriksen CA, Theorell T, Ulrich R, Rasmanis G: Acoustics and psychosocial environment in intensive coronary care. Occup Environ Med 2005, 62: e1. Epub 2005 Feb 23 10.1136/oem.2004.017632
Kahn DM, Cook TE, Carlisle CC, Nelson DL, Kramer NR, Millman RP: Identification and modification of environmental noise in an ICU setting. Chest 1998, 114: 535-540. Epub 1998 Sept 3 10.1378/chest.114.2.535
Meyer TJ, Eveloff SE, Bauer MS, Schwartz WA, Hill NS, Millman RP: Adverse environmental conditions in the respiratory and medical ICU settings. Chest 1994, 105: 1211-1216. Epub 1994 Apr 01 10.1378/chest.105.4.1211
Gronfier C, Wright KP Jr, Kronauer RE, Czeisler CA: Entrainment of the human circadian pacemaker to longer-than-24-h days. Proc Natl Acad Sci U S A 2007, 104: 9081-9086. Epub 2007 May 16 10.1073/pnas.0702835104
Dimsdale JE, Norman D, DeJardin D, Wallace MS: The effect of opioids on sleep architecture. J Clin Sleep Med 2007, 3: 33-36. Epub 2007 June 15
Monti MJ, Monti D: Overview of currently available benzodiazepine and nonbenzodiazepine hypnotics. In Clinical Pharmacology of Sleep. Edited by: Pandi-Perumal SR, Monti JM. Basel, Switzerland: Birkhauser Verlag; 2006:207-223.
McKinley S, Elliott R, Elliott D, Fien M (Eds): Intensive care patients report that their sleep is poor In In Proceedings of the 36th Australian and New Zealand Intensive Care Society andAustralian College of Critical Care Nurses Annual Scientific Meeting (ASM) onIntensive Care. Brisbane, Australia; 2011.
Frisk U, Nordstrom G: Patients' sleep in an intensive care unit - patients' and nurses' perception. Intensive Crit Care Nurs 2003, 19: 342-349. Epub 2003 Nov 26 10.1016/S0964-3397(03)00076-4
Drouot X, Roche-Campo F, Thille AW, Cabello B, Galia F, Margarit L, d'Ortho MP, Brochard L: A new classification for sleep analysis in critically ill patients. Sleep Med 2012, 13: 7-14. Epub 2011 Dec 14 10.1016/j.sleep.2011.07.012
Bastien CH, LeBlanc M, Carrier J, Morin CM: Sleep EEG power spectra, insomnia, and chronic use of benzodiazepines. Sleep 2003, 26: 313-317. Epub 2003 May 17
Aeschbach D, Dijk DJ, Trachsel L, Brunner DP, Borbely AA: Dynamics of slow-wave activity and spindle frequency activity in the human sleepEEG: effect of midazolam and zopiclone. Neuropsychopharmacology 1994, 11: 237-244. Epub 1994 Dec 1 10.1038/sj.npp.1380110
Danker-Hopfe H, Anderer P, Zeitlhofer J, Boeck M, Dorn H, Gruber G, Heller E, Loretz E, Moser D, Parapatics S, Saletu B, Schmidt A, Dorffner G: Interrater reliability for sleep scoring according to the Rechtschaffen &Kales and the new AASM standard. J Sleep Res 2009, 18: 74-84. Epub 2009 Mar 3 10.1111/j.1365-2869.2008.00700.x
Fontaine DK: Measurement of nocturnal sleep patterns in trauma patients. Heart Lung 1989, 18: 402-410. Epub 1989 July 1
Ambrogio C, Koebnick J, Quan SF, Ranieri M, Parthasarathy S: Assessment of sleep in ventilator-supported critically III patients. Sleep 2008, 31: 1559-1568. Epub 2008 Nov 19
Acknowledgements
The authors thank the Intensive Care Foundation, Australian College of Critical CareNurses, the Skipper family (Royal North Shore Hospital Nursing Research Scholarship),the Northcare Foundation, Pink Ladies Committee (Royal North Shore Hospital), Facultyof Engineering and Information Technology (University of Technology Sydney) and thepatients and health care personnel for their generous contributions to the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
RE conceived and developed the protocol and design, acquired and analysed the data,wrote the manuscript, SM and PC supervised RE, assisted with the development of thedesign, interpretation of the data and writing the manuscript and MF assisted withprotocol development, data acquisition and writing the manuscript. All the authors haveread and approved the manuscript for publication.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Elliott, R., McKinley, S., Cistulli, P. et al. Characterisation of sleep in intensive care using 24-hour polysomnography: anobservational study. Crit Care 17, R46 (2013). https://doi.org/10.1186/cc12565
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc12565