Abstract
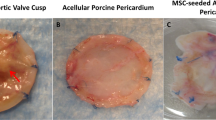
Tissue engineered heart valve is a promising alternative to current heart valve surgery, for its capability of growth, repair, and remodeling. However, extensive development is needed to ensure tissue compatibility, durability and antithrombotic potential. This study aims to investigate the biological effects of multi-signal composite material of polyethyl glycol-cross-linked decellularized valve on adhesion and proliferation of endothelial progenitor cells. Group A to E was decellularized valve leaflets, composite material of polyethyl glycol-cross-linked decellularized valves leaflets, vascular endothelial growth factor-composite materials, Arg-Gly-Asp peptide-composite materials and multi-signal modified materials of polyethyl glycol-cross-linked decellularized valve leaflets, respectively. The endothelial progenitor cells were seeded for each group, cell adhesion and proliferation were detected and neo-endothelium antithrombotic function of the multi-signal composite materials was evaluated. At 2, 4, and 8 h after the seeding, the cell numbers and 3H-TdR incorporation in group D were the highest. At 2, 4, and 8 days after the seeding, the cell numbers and 3H-TdR incorporation were significantly higher in groups C, D, and E compared with groups A and B (P < 0.05) and cell numbers and the expression of t-PA and eons in the neo-endothelium were quite similar to those in the human umbilical vein endothelial cells at 2, 4, and 8 days after the seeding. The Arg-Gly-Asp- peptides (a sequential peptide composed of arginine (Arg), glycine (Gly) and aspartic acid (Asp)) and VEGF-conjugated onto the composite material of PEG-crosslinked decellularized valve leaflets synergistically promoted the adhesion and proliferation of endothelial progenitor cells on the composite material, which may help in tissue engineering of heart valves.







Similar content being viewed by others
References
Mathew JG, Spyropoulos AC, Yusuf A, Vincent J, Eikelboom J, Shestakovska O, Fremes S, Noora J, Guo L, Peterson M, Pai M, Whitlock R. Efficacy and safety of early parenteral anticoagulation as a bridge to warfarin after mechanical valve replacement. Throm haemost. 2014;112(6):1120–8. doi:10.1160/th14-03-0284.
Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr., Bolger AF, Levison ME, Ferrieri P, Gerber MA, Tani LY, Gewitz MH, Tong DC, Steckelberg JM, Baltimore RS, Shulman ST, Burns JC, Falace DA, Newburger JW, Pallasch TJ, Takahashi M, Taubert KA. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation. 2005;111(23):e394–e434. doi:10.1161/circulationaha.105.165564.
Parvin Nejad S, Blaser MC, Santerre JP, Caldarone CA, Simmons CA. Biomechanical conditioning of tissue engineered heart valves: too much of a good thing?. Adv Drug deliv Rev. 2016;96:161–75. doi:10.1016/j.addr.2015.11.003.
Kasimir MT, Weigel G, Sharma J, Rieder E, Seebacher G, Wolner E, Simon P. The decellularized porcine heart valve matrix in tissue engineering: platelet adhesion and activation. Throm haemost. 2005;94(3):562–7. doi:10.1160/TH05-01-0025.
Breuer CK, Mettler BA, Anthony T, Sales VL, Schoen FJ, Mayer JE. Application of tissue-engineering principles toward the development of a semilunar heart valve substitute. Tissue Eng. 2004;10(11-12):1725–36. doi:10.1089/ten.2004.10.1725.
de Mel A, Jell G, Stevens MM, Seifalian AM. Biofunctionalization of biomaterials for accelerated in situ endothelialization: a review. Biomacromolecules. 2008;9(11):2969–79. doi:10.1021/bm800681k.
Hu XJ, Dong NG, Shi JW, Deng C, Li HD, Lu CF. Evaluation of a novel tetra-functional branched poly(ethylene glycol) crosslinker for manufacture of crosslinked, decellularized, porcine aortic valve leaflets. J Biomed Mater Res Part B Appl Biomater. 2014;102(2):322–36. doi:10.1002/jbm.b.33010.
Gloria A, Causa F, Russo T, Battista E, Della Moglie R, Zeppetelli S, De Santis R, Netti PA, Ambrosio L. Three-dimensional poly(ε-caprolactone) bioactive scaffolds with controlled structural and surface properties. Biomacromolecules. 2012;13(11):3510–21. doi:10.1021/bm300818y.
Lee J, Guarino V, Gloria A, Ambrosio L, Tae G, Kim YH, Jung Y, Kim SH, Kim SH. Regeneration of Achilles’ tendon: the role of dynamic stimulation for enhanced cell proliferation and mechanical properties. J Biomater Sci Polym Ed. 2010;21(8-9):1173–90. doi:10.1163/092050609X12471222313524.
Hu Y, Winn SR, Krajbich I, Hollinger JO. Porous polymer scaffolds surface-modified with arginine-glycine-aspartic acid enhance bone cell attachment and differentiation in vitro. J Biomed Mater Res Part A. 2003;64(3):583–90. doi:10.1002/jbm.a.10438.
Dong X, Wei X, Yi W, Gu C, Kang X, Liu Y, Li Q, Yi D. RGD-modified acellular bovine pericardium as a bioprosthetic scaffold for tissue engineering. J Mater Sci Mater Med. 2009;20(11):2327–36. doi:10.1007/s10856-009-3791-4.
Hersel U, Dahmen C, Kessler H. RGD modified polymers: biomaterials for stimulated cell adhesion and beyond. Biomaterials. 2003;24(24):4385–415.
Pallarola D, Bochen A, Boehm H, Rechenmacher F, Sobahi TR, Spatz JP, Kessler H. Interface immobilization chemistry of cRGD‐based peptides regulates integrin mediated cell adhesion. Adv Funct Mater. 2014;24(7):943–56.
Shachar M, Tsur-Gang O, Dvir T, Leor J, Cohen S. The effect of immobilized RGD peptide in alginate scaffolds on cardiac tissue engineering. Acta Biomater. 2011;7(1):152–62. doi:10.1016/j.actbio.2010.07.034.
Shi J, Dong N, Sun Z. Immobilization of decellularized valve scaffolds with Arg-Gly-Asp-containing peptide to promote myofibroblast adhesion. J Huazhong Univ Sci Technol Med Sci. 2009;29(4):503–7. doi:10.1007/s11596-009-0422-8.
Tran NQ, Joung YK, Lih E. RGD-conjugated in situ forming hydrogels as cell-adhesive injectable scaffolds. Macromol Res. 2011;19(3):300–6.
Wang H, Ma L, Yang S, Shao Z, Meng C, Duan D, Li Y. Effect of RGD-modified silk material on the adhesion and proliferation of bone marrow-derived mesenchymal stem cells. J Huazhong Univ Sci Technol Med Sci. 2009;29(1):80–3. doi:10.1007/s11596-009-0117-1.
Zhu J, He P, Lin L, Jones DR, Marchant RE. Biomimetic poly(ethylene glycol)-based hydrogels as scaffolds for inducing endothelial adhesion and capillary-like network formation. Biomacromolecules 2012;13(3):706–13. doi:10.1021/bm201596w.
Zhu J, Tang C, Kottke-Marchant K, Marchant RE. Design and synthesis of biomimetic hydrogel scaffolds with controlled organization of cyclic RGD peptides. Bioconjugate Chem. 2009;20(2):333–9. doi:10.1021/bc800441v.
Ferrara N, Houck K, Jakeman L, Leung DW. Molecular and biological properties of the vascular endothelial growth factor family of proteins. Endocr Rev. 1992;13(1):18–32. doi:10.1210/edrv-13-1-18.
Neufeld G, Cohen T, Gengrinovitch S, Poltorak Z. Vascular endothelial growth factor (VEGF) and its receptors. FASEB J. 1999;13(1):9–22.
Zisch AH, Lutolf MP, Ehrbar M, Raeber GP, Rizzi SC, Davies N, Schmokel H, Bezuidenhout D, Djonov V, Zilla P, Hubbell JA. Cell-demanded release of VEGF from synthetic, biointeractive cell ingrowth matrices for vascularized tissue growth. FASEB J. 2003;17(15):2260–2. doi:10.1096/fj.02-1041fje.
Knetsch ML, Koole LH. VEGF-E enhances endothelialization and inhibits thrombus formation on polymeric surfaces. J Biomed Mater Res Part A. 2010;93(1):77–85. doi:10.1002/jbm.a.32538.
Müller S, Koenig G, Charpiot A. VEGF-functionalized polyelectrolyte multilayers as proangiogenic prosthetic coatings. Adv Funct Mater. 2008;18(12):1767–75.
Shen YH, Shoichet MS, Radisic M. Vascular endothelial growth factor immobilized in collagen scaffold promotes penetration and proliferation of endothelial cells. Acta Biomater. 2008;4(3):477–89. doi:10.1016/j.actbio.2007.12.011.
Porter AM, Klinge CM, Gobin AS. Biomimetic hydrogels with VEGF induce angiogenic processes in both hUVEC and hMEC. Biomacromolecules. 2011;12(1):242–6. doi:10.1021/bm101220b.
Leslie-Barbick JE, Moon JJ, West JL. Covalently-immobilized vascular endothelial growth factor promotes endothelial cell tubulogenesis in poly(ethylene glycol) diacrylate hydrogels. J Biomater Sci Polym Ed. 2009;20(12):1763–79. doi:10.1163/156856208X386381.
Poh CK, Shi Z, Lim TY, Neoh KG, Wang W. The effect of VEGF functionalization of titanium on endothelial cells in vitro. Biomaterials. 2010;31(7):1578–85. doi:10.1016/j.biomaterials.2009.11.042.
Leach JK, Kaigler D, Wang Z, Krebsbach PH, Mooney DJ. Coating of VEGF-releasing scaffolds with bioactive glass for angiogenesis and bone regeneration. Biomaterials. 2006;27(17):3249–55. doi:10.1016/j.biomaterials.2006.01.033.
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275(5302):964–7.
Sales VL, Engelmayr GC Jr., Mettler BA, Johnson JA Jr., Sacks MS, Mayer JE Jr. Transforming growth factor-beta1 modulates extracellular matrix production, proliferation, and apoptosis of endothelial progenitor cells in tissue-engineering scaffolds. Circulation. 2006;114(1 Suppl):I193–9. doi:10.1161/circulationaha.105.001628.
Wu X, Rabkin-Aikawa E, Guleserian KJ, Perry TE, Masuda Y, Sutherland FW, Schoen FJ, Mayer JE Jr., Bischoff J. Tissue-engineered microvessels on three-dimensional biodegradable scaffolds using human endothelial progenitor cells. Am J Physiol Heart Circ Physiol. 2004;287(2):H480–H487. doi:10.1152/ajpheart.01232.2003.
Hristov M, Erl W, Weber PC. Endothelial progenitor cells: isolation and characterization. Trends Cardiovasc Med. 2003;13(5):201–6.
Chen JS, Noah EM, Pallua N, Steffens GC (2002) The use of bifunctional polyethyleneglycol derivatives for coupling of proteins to and cross-linking of collagen matrices. J Mater Sci Mater Med. 13 (11):1029–35.
Kalka C, Masuda H, Takahashi T, Kalka-Moll WM, Silver M, Kearney M, Li T, Isner JM, Asahara T. Transplantation of ex vivo expanded endothelial progenitor cells for therapeutic neovascularization. Proc Natl Acad Sci USA. 2000;97(7):3422–7. doi:10.1073/pnas.070046397.
Murohara T, Ikeda H, Duan J, Shintani S, Sasaki K, Eguchi H, Onitsuka I, Matsui K, Imaizumi T. Transplanted cord blood-derived endothelial precursor cells augment postnatal neovascularization. J Clin Invest. 2000;105(11):1527–36. doi:10.1172/JCI8296.
Zhang HR, Chen FL, Xu CP, Ping YF, Wang QL, Liang ZQ, Wang JM, Bian XW. Incorporation of endothelial progenitor cells into the neovasculature of malignant glioma xenograft. J Neurooncol. 2009;93(2):165–74. doi:10.1007/s11060-008-9757-4.
Casamassimi A, Balestrieri ML, Fiorito C, Schiano C, Maione C, Rossiello R, Grimaldi V, Del Giudice V, Balestrieri C, Farzati B, Sica V, Napoli C. Comparison between total endothelial progenitor cell isolation versus enriched Cd133+ culture. J Biochem. 2007;141(4):503–11. doi:10.1093/jb/mvm060.
Jaffe EA, Nachman RL, Becker CG, Minick CR. Culture of human endothelial cells derived from umbilical veins. Identification by morphologic and immunologic criteria. J Clin Invest. 1973;52(11):2745–56. doi:10.1172/JCI107470.
Park SJ, Baek SH, Oh MK, Choi SH, Park EH, Kim NH, Shin JC, Kim IS. Enhancement of angiogenic and vasculogenic potential of endothelial progenitor cells by haptoglobin. FEBS Lett. 2009;583(19):3235–40. doi:10.1016/j.febslet.2009.09.014.
Kasimir MT, Rieder E, Seebacher G, Nigisch A, Dekan B, Wolner E, Weigel G, Simon P. Decellularization does not eliminate thrombogenicity and inflammatory stimulation in tissue-engineered porcine heart valves. J Heart Valve Dis. 2006;15(2):278–86. discussion 286
Assmann A, Delfs C, Munakata H, Schiffer F, Horstkotter K, Huynh K, Barth M, Stoldt VR, Kamiya H, Boeken U, Lichtenberg A, Akhyari P. Acceleration of autologous in vivo recellularization of decellularized aortic conduits by fibronectin surface coating. Biomaterials. 2013;34(25):6015–26. doi:10.1016/j.biomaterials.2013.04.037.
Dohmen PM, Ozaki S, Nitsch R, Yperman J, Flameng W, Konertz W. A tissue engineered heart valve implanted in a juvenile sheep model. Med Sci Monitor Int Med J Exp Clin Res. 2003;9(4):BR97–BR104.
Zhou J, Fritze O, Schleicher M, Wendel HP, Schenke-Layland K, Harasztosi C, Hu S, Stock UA. Impact of heart valve decellularization on 3-D ultrastructure, immunogenicity and thrombogenicity. Biomaterials. 2010;31(9):2549–54. doi:10.1016/j.biomaterials.2009.11.088.
Lai Y, Xie C, Zhang Z, Lu W, Ding J. Design and synthesis of a potent peptide containing both specific and non-specific cell-adhesion motifs. Biomaterials. 2010;31(18):4809–17. doi:10.1016/j.biomaterials.2010.02.064.
Shinkai A, Ito M, Anazawa H, Yamaguchi S, Shitara K, Shibuya M. Mapping of the sites involved in ligand association and dissociation at the extracellular domain of the kinase insert domain-containing receptor for vascular endothelial growth factor. J Biol Chem. 1998;273(47):31283–8.
Shibuya M. Vascular endothelial growth factor receptor-2: its unique signaling and specific ligand, VEGF-E. Cancer Sci. 2003;94(9):751–6.
Holmes K, Roberts OL, Thomas AM, Cross MJ. Vascular endothelial growth factor receptor-2: structure, function, intracellular signalling and therapeutic inhibition. Cell Signal. 2007;19(10):2003–12. doi:10.1016/j.cellsig.2007.05.013.
Lutolf MP, Tirelli N, Cerritelli S, Cavalli L, Hubbell JA. Systematic modulation of Michael-type reactivity of thiols through the use of charged amino acids. Bioconjugate Chem. 2001;12(6):1051–6.
Lutolf MP, Hubbell JA. Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering. Nat Biotechnol. 2005;23(1):47–55. doi:10.1038/nbt1055
Dohmen PM, Lembcke A, Hotz H, Kivelitz D, Konertz WF. Ross operation with a tissue-engineered heart valve. Ann Thorac Surg. 2002;74(5):1438–42.
Peichev M, Naiyer AJ, Pereira D, Zhu Z, Lane WJ, Williams M, Oz MC, Hicklin DJ, Witte L, Moore MA, Rafii S. Expression of VEGFR-2 and AC133 by circulating human CD34(+) cells identifies a population of functional endothelial precursors. Blood. 2000;95(3):952–8.
Rocha V, Wagner JE Jr., Sobocinski KA, Klein JP, Zhang MJ, Horowitz MM, Gluckman E. Graft-versus-host disease in children who have received a cord-blood or bone marrow transplant from an HLA-identical sibling. Eurocord and International Bone Marrow Transplant Registry Working Committee on Alternative Donor and Stem Cell Sources. N Engl J Med. 2000;342(25):1846–54. doi:10.1056/NEJM200006223422501.
Schmidt D, Breymann C, Weber A, Guenter CI, Neuenschwander S, Zund G, Turina M, Hoerstrup SP. Umbilical cord blood derived endothelial progenitor cells for tissue engineering of vascular grafts. Ann Thorac Surg. 2004;78(6):2094–8. doi:10.1016/j.athoracsur.2004.06.052.
Avci-Adali M, Paul A, Ziemer G, Wendel HP. New strategies for in vivo tissue engineering by mimicry of homing factors for self-endothelialisation of blood contacting materials. Biomaterials. 2008;29(29):3936–45. doi:10.1016/j.biomaterials.2008.07.002.
Sales VL, Mettler BA, Engelmayr GC Jr., Aikawa E, Bischoff J, Martin DP, Exarhopoulos A, Moses MA, Schoen FJ, Sacks MS, Mayer JE Jr. Endothelial progenitor cells as a sole source for ex vivo seeding of tissue-engineered heart valves. Tissue Eng Part A. 2010;16(1):257–67. doi:10.1089/ten.TEA.2009.0424.
Yang HN, Park JS, Woo DG, Jeon SY, Park KH. Transfection of VEGF(165) genes into endothelial progenitor cells and in vivo imaging using quantum dots in an ischemia hind limb model. Biomaterials. 2012;33(33):8670–84. doi:10.1016/j.biomaterials.2012.08.012.
Ye X, Wang H, Zhou J, Li H, Liu J, Wang Z, Chen A, Zhao Q. The effect of Heparin-VEGF multilayer on the biocompatibility of decellularized aortic valve with platelet and endothelial progenitor cells. PloS One. 2013;8(1):e54622 doi:10.1371/journal.pone.0054622.
Suh W, Kim KL, Choi JH, Lee YS, Lee JY, Kim JM, Jang HS, Shin IS, Lee JS, Byun J, Jeon ES, Kim DK. C-reactive protein impairs angiogenic functions and decreases the secretion of arteriogenic chemo-cytokines in human endothelial progenitor cells. Biochem Biophys Res Commun. 2004;321(1):65–71. doi:10.1016/j.bbrc.2004.06.107.
Xing F, Jiang Y, Liu J, Zhao K, Mo Y, Qin Q, Wang J, Ouyang J, Zeng Y. Role of AP1 element in the activation of human eNOS promoter by lysophosphatidylcholine. J Cell Biochem. 2006;98(4):872–84. doi:10.1002/jcb.20739.
Yang Z, Tao J, Wang JM, Tu C, Xu MG, Wang Y, Pan SR. Shear stress contributes to t-PA mRNA expression in human endothelial progenitor cells and nonthrombogenic potential of small diameter artificial vessels. Biochem Biophys Res Commun. 2006;342(2):577–84. doi:10.1016/j.bbrc.2006.01.172.
Fang NT, Xie SZ, Wang SM, Gao HY, Wu CG, Pan LF. Construction of tissue-engineered heart valves by using decellularized scaffolds and endothelial progenitor cells. Chin Med J. 2007;120(8):696–702.
Kan WH, Hsu JT, Ba ZF, Schwacha MG, Chen J, Choudhry MA, Bland KI, Chaudry IH. p38 MAPK-dependent eNOS upregulation is critical for 17beta-estradiol-mediated cardioprotection following trauma-hemorrhage. Am J Physiol Heart Circ Physiol. 2008;294(6):H2627–H2636. doi:10.1152/ajpheart.91444.2007.
Sawada N, Salomone S, Kim HH, Kwiatkowski DJ, Liao JK. Regulation of endothelial nitric oxide synthase and postnatal angiogenesis by Rac1. Circ Res. 2008;103(4):360–8. doi:10.1161/CIRCRESAHA.108.178897.
Schoen FJ. Evolving concepts of cardiac valve dynamics: the continuum of development, functional structure, pathobiology, and tissue engineering. Circulation. 2008;118(18):1864–80. doi:10.1161/circulationaha.108.805911.
Acknowledgments
This study was funded by a grant from the National High-tech Research and Development Program (863 Program) of China (No. 2014AA020539), the National Natural Science Foundation of China (No. 81260047, No. 81270297, and No. 31330029), and the Youth Science Foundation of Jiangxi Province, China (20122BAB215016).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Jianliang Zhou and Jingli Ding contributed to equally to this work.
Rights and permissions
About this article
Cite this article
Zhou, J., Ding, J., Nie, B. et al. Promotion of adhesion and proliferation of endothelial progenitor cells on decellularized valves by covalent incorporation of RGD peptide and VEGF. J Mater Sci: Mater Med 27, 142 (2016). https://doi.org/10.1007/s10856-016-5750-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5750-1