Abstract
This commentary describes the transition to remote delivery of cognitive-behavioral therapy (CBT) for anxiety in children with autism spectrum disorder (ASD) who participates in a clinical trial during the COVID-19 pandemic. The effects of COVID-19 on children’s anxiety and on the family functioning are discussed. Modifications to CBT necessitated by telehealth delivery were aimed at maximizing engagement of children and their parents while maintaining treatment fidelity and adhering to the research protocol. Treatment targets were updated to address new sources of anxiety and CBT exposure exercises were modified to accommodate the new reality of quarantine restrictions. If the COVID-19 pandemic continues to affect treatment delivery it may require a widespread utilization of telehealth for treating anxiety in children with ASD.
Similar content being viewed by others
Introduction
The 2020 novel coronavirus (COVID-19) pandemic has disrupted routines and added stress to the lives of children and families across the globe. In the months since the outbreak of COVID-19, rates of mental health concerns have precipitously risen in youth, with up to 80% of youth with histories of mental health needs reporting a worsening of symptoms (YoungMinds 2020). While sobering, these results are unsurprising given the numerous stressors that the pandemic has introduced to the daily lives of families, including anxiety about infection, school closures, reduced access to social and community supports, economic recession, and a continued sense of uncertainty, as plans, policies, and projections change almost daily.
Families of children with disabilities may experience additional challenges as a result of the pandemic. In this paper, we focus on children with autism spectrum disorder (ASD) and co-occurring anxiety disorders. Pervasive uncertainty and disruption of routines may be particularly distressing for a child with ASD leading to exacerbation of existing anxiety or newly emerging anxiety symptoms (Fegert et al. 2020; Lee 2020; SPARK 2020). In addition, school closures have reduced access to important school-based supports for children with ASD, such as speech therapy, occupational therapy, and social skills groups (Aman and Pearson 2020; Fegert et al. 2020; Lee 2020). Reflecting the impact of these added stressors, in a survey of 8000 US-based caregivers of children with ASD, 95% of caregivers reported that COVID-related disruptions in services or therapies had negatively affected their child with ASD, and 97% of caregivers reported feeling stressed or overwhelmed as a result of these disruptions (SPARK 2020).
In response to the pandemic, clinical psychologists and psychiatrists world-wide have transitioned to telehealth, here defined as the remote, synchronous delivery of psychotherapy via telephone or videoconferencing platforms (Jurcik et al. 2020; Perrin et al. 2020; Sharma et al. 2020). The transition to telehealth has altered the implementation of therapy and required considerable flexibility on the part of clinicians and patients. Almost overnight, clinicians had to develop proficiency with unfamiliar technologies and help patients to do the same (Sharma et al. 2020). Telehealth presented a number of new challenges, such as finding private, distraction-free locations at home (Payne et al. 2020; Perrin et al. 2020) with adequate internet connections; and accurately communicating and interpreting intent and meaning in the absence of usual non-verbal cues (Payne et al. 2020). These latter challenges were uniquely difficult for children with ASD and required clinicians to make appropriate modifications.
Rationale for This Commentary
Approximately 40% of children with ASD meet criteria for co-occurring anxiety disorders (Lai et al. 2019), and cognitive behavioral therapy (CBT) for anxiety in ASD has been shown to be an effective treatment (Perihan et al. 2020). In this paper, we address how COVID-19 impacted the delivery of this treatment conducted in the context of a randomized controlled trial of CBT versus psychoeducation supportive therapy (PST) in 8–14 year-old children with ASD and anxiety (Sukhodolsky 2020). In this commentary, we discuss: (1) COVID-19’s effect on children’s symptomology and family functioning, (2) our implementation and adaptation of therapy to address these concerns, (3) the effect of the transition to telehealth in response to COVID-19 on treatment implementation, and (4) how our treatment modifications maximized benefits and reduced the challenges associated with telehealth for our patients.
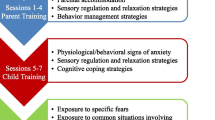
The CBT administered in the current randomized trial utilized a treatment approach developed by Jeffrey Wood and colleagues, Behavioral Intervention for Anxiety in Children with Autism (BIACA) (Wood et al. 2009, 2020). It includes 16 weekly sessions in which the clinician meets with the child and parent separately, although joint meetings are conducted when useful. Treatment focuses on identifying anxious feelings, recognizing anxiety-provoking thoughts, developing coping skills, and engaging in exposure exercises. Sessions are conducted in a modular format to allow for personalization of treatment, with several modules focused on social challenges and other issues relevant to ASD. We reasoned that our experience of conducting CBT during the COVID-19 pandemic could be informative to those who work with children with ASD complicated by anxiety either in clinical or research settings.
Prior to treatment, all children are comprehensively evaluated with regard to ASD and co-occurring anxiety, using the Anxiety Disorders Interview Schedule (ADIS) (Silverman and Albano 1996) and the Pediatric Anxiety Rating Scale (PARS) (RUPP Anxiety Study Group 2002). Based on this evaluation, two to three primary target symptoms are identified for treatment for each child. Importantly, following the onset of COVID-19, many of the children in our study experienced a wide variety of notable changes in their anxiety symptomology and psychological functioning.
In March 2020, following the COVID-19 outbreak and state and local stay-at-home directives, eight subjects were in the active phase of the study (four in CBT and four in PST) and were either receiving treatment or about to begin treatment. We proceeded with delivering therapy via telehealth to these subjects, and, thus the transition to telehealth occurred during the course of treatment for some families and at the outset of treatment for others. Below, we describe the changes to treatment delivery we made in response to the new set of realities and challenges conferred by COVID-19 while remaining adherent to the core principles and elements of CBT and to the study protocol.
Impact of COVID-19 on Study Participants and Their Anxiety Symptoms
The COVID-19 pandemic impacted the daily lives of children and their families in significant ways. For all the children in our study, schools were physically closed, and academic curricula were transitioned to online platforms with varying degrees of success across districts. Similarly, most parents experienced changes in their work situation, and many transitioned to working from home. All families adhered to stay-at-home and social distancing directives, including limiting trips outside the home to essential excursions, such as grocery shopping, and restricting in-person contact with people outside the home. Lastly, for many families, staying safe and avoiding contracting COVID-19 surfaced as a new set of serious concerns.
As might be expected, several children reported increases in anxiety symptoms, including new fears of contracting COVID-19. This tendency to experience elevated anxiety regarding COVID-19 was especially prominent for two children with a diagnosis of generalized anxiety disorder and pronounced worries surrounding hygiene, health, and safety. One child with pervasive worry about his family’s well-being experienced a sharp increase in anxiety symptoms focused on the health and safety of himself and his family. In addition to daily perseveration on the spread of COVD-19 and persistent worries about how others could inadvertently infect him and his family, he also became preoccupied with checking himself and his family members for symptoms by taking temperatures multiple times per day and constantly asking his parents how they were feeling. Similarly, the other child with intense fear of COVID-19 took excessive precautions to avoid contracting the virus, including refusing to leave his home or even to step into his backyard. For both of these children, their anxiety related to COVID-19, while situational, was excessive in comparison to same-aged children or peers with ASD.
In contrast, reduced demands on social participation brought on by COVID-19 temporarily reduced the frequency of social anxiety symptoms. Most notably, for two children with social anxiety disorder, the transition to online school meant the cessation of anxiety-provoking in-person interactions with peers at school. Activities that typically triggered anxiety, such as answering questions in class, walking in the hallway, navigating social interactions at lunch and recess, and engaging in extracurricular activities were no longer part of their daily experience. As such, the lack of exposure to these situations resulted in a reduced frequency of anxiety symptoms for these children, and they commented that they were “glad” not to have to go to school. The parents were more concerned (than their children) about the effects of school closures on the loss of daily structure, special education services and socialization opportunities that are afforded by in-person schooling. In addition, anticipatory anxiety prior to attending school also markedly decreased, translating into reduced levels of anxiety at home. The reduction in social anxiety symptoms experienced by these two children is consistent with other research describing decreases in children’s social anxiety-related distress in response to social distancing practices associated with COVID-19 (Chen et al. 2020; Morrissette 2020).
Still, for most children in the study, their overall anxiety during the onset of COVID-19 did not clearly increase or decrease but instead changed qualitatively with regard to the content of anxious thoughts and antecedents of anxiety. For example, while two children with social anxiety welcomed the transition to online learning as a respite from daily in-person interactions with peers, others found the shift to online learning rife with new challenges. This was especially true for one child whose school utilized a “virtual classroom” platform, requiring children to engage with teachers and peers over videoconferencing. Following the transition to the virtual classroom, she displayed heightened anxiety both during the experience of online learning and in anticipation of it. Most mornings before starting school, she reported high levels of distress and discomfort, usually accompanied by panicked breathing, crying, or curling up on her bed or the couch. During these times, she often described feeling very “uncomfortable” and explicitly expressed unwillingness to attend online school. On some days, her parents could help her calm down enough to join the class virtually, while on other days, she was unable to calm down and avoided school all together. On the days that she attended online school, she disabled the video feature (so that others could not see her) and usually attended for short periods of time (up to 20 min) before becoming anxious, precipitating her signing off from the online platform.
Similarly, for children with anxiety surrounding separation from parents, the core features of separation anxiety remained but the frequency and specific manifestation of symptoms changed. For example, for two children with separation anxiety disorder, stay-at-home directives resulted in a situation in which they and their parents were at home together for most, if not all, of the day. As such, common triggers of separation anxiety (e.g., attending school and after-school activities, staying at home with a babysitter) virtually disappeared, and thus the frequency of expressed worry regarding separation decreased. However, for both children, when instances necessitating separation did arise, their experiences of separation anxiety remained comparable to, or even more intense than, their pre-pandemic levels. For example, for one of the children who also had fears of contracting COVID-19, every time his mother went to the grocery store, he became extremely anxious and worried that she would not return safely. As a result, he would repeatedly call her while she was at the store to check on her. If she did not respond right away, he would become increasingly distressed to the point that other family members in the home had to intervene to calm him down.
Addressing COVID-19 During CBT for Anxiety
In all CBT cases, the clinicians thoroughly reviewed current anxiety symptomatology at the outset of treatment and then, in collaboration with the children and their parents, they generated two to three treatment goals. For children starting treatment at the start of the COVID-19 outbreak, treatment goals were determined based on current anxiety symptoms, including those associated with COVID-19 (e.g., worries about family members contracting the virus, fear and avoidance of attending school online). For children who had started treatment prior to the onset of the pandemic, anxiety symptoms were re-evaluated and treatment goals were updated as necessary to address the children’s most salient and current anxiety concerns. For one child, for example, reduction of fear of heights had been one of the main treatment goals prior to COVID-19. This fear interfered with his ability to participate in leisure activities, such as using a slide at the playground or accompanying his family on hikes due to a chance that a trail might go over a bridge. Prior to COVID-19, treatment included a hierarchy of exposures to reduce fear of heights, including walking upstairs in the clinic, visiting a toy store on the second floor of the local mall, and using the largest slide at the local playground. For obvious reasons, most of these exposures could not be implemented during the pandemic. Thus, following the outbreak, the clinician and family shifted the treatment plan to focus on the child’s separation anxiety, which was becoming increasingly prominent and tied to COVID-19 related concerns. To this end, treatment consisted of a hierarchy of exposures: the child’s mother leaving the house for a 5-min errand, then a 30-min errand, and finally working up to a 30-min errand without responding to any of his calls or text messages during that time.
At the beginning of the pandemic, and subsequently as needed, treatment inevitably addressed how the COVID-19 outbreak was affecting a child and the family. This included a conversation with parents about the best way to discuss the pandemic with their children, how much information to provide and how to answer questions and concerns raised by the child. The clinicians encouraged parents to consider their children’s developmental level, including language and cognitive abilities, emotional maturity, level of anxiety surrounding COVID-19, and severity of ASD symptoms in preparation for discussing the pandemic with their children. Parents were advised to provide information using developmentally appropriate language and level of detail (e.g., “there is a virus, like the flu, that some people have, and we are staying away from other people so that we do not get it from them”) and to limit information that was too advanced, practically unnecessary, and/or would needlessly exacerbate anxiety (e.g., details regarding the impact of COVID-19 on the human body). For many families, this included limiting children’s exposure to news and media coverage of the pandemic. Parents were also encouraged to answer their children’s questions and provide information in a clear, developmentally appropriate way in order to help their children better understand and contextualize the changes in their daily lives (e.g., “since a person with the virus can give it to another person by getting their germs into the other person’s nose or mouth, we are going to wear masks when we go outside so no one’s germs get into our nose or mouth”). Lastly, parents were coached to provide reassuring information where possible (e.g., “we are doing our best to stay safe,” “lots of doctors and nurses are working hard to make people with the virus better and to figure out how to get rid of the virus”) to help their children maintain a resilient mindset in the face of uncertainty brought about by the pandemic. As the pandemic unfolded and information about COVID-19 and child behavioral health became available, we compiled the website resources that were helpful to us when working with children with ASD and their families (see Table in the “Supplementary material”).
COVID-19-related anxiety was also addressed by working directly with the child. The goals of this work included reducing anxiety about the virus and helping the child to engage in appropriate safety behaviors. This included adopting a more realistic perspective regarding risks and necessary precautions and limiting engagement in safety-taking behaviors to those consistent with standard medical guidelines. To this end, psychoeducation on COVID-19, including information on mode of transmission, relative levels of risk, and guidelines for prevention from authoritative medical institutions (e.g., Centers for Disease Control and Prevention) was provided and geared to the developmental level of the child. For example, for the child who refused to step out of the house and play in the backyard out of fear of contracting COVID-19, detailed information was provided on how the virus is spread (i.e., via person-to-person contact, transmission of water droplets), complete with illustrative diagrams. The clinician and child reviewed this information several times while also reviewing how this information contrasted with the child’s anxiety-provoking thoughts (e.g., “COVID is in the outside air, and if I step outside, I will catch it”). Next, the clinician helped the child to generate coping statements to remind himself of the newly-learned information and combat his anxious thoughts (e.g., “I cannot catch COVID-19 by simply going outside to play”). Following that, he and the clinician developed a fear hierarchy corresponding to situations involving him stepping outside of his home, ranging from mildly anxiety-provoking situations (e.g., taking one step outside and stepping back inside) to highly anxiety-provoking ones (e.g., going for a 15-min walk in his neighborhood, while wearing a facial mask and maintaining a six-foot distance from others). They also reviewed the fear hierarchy with the child’s mother, who subsequently helped him to carry out the exposure exercises in accordance with the hierarchy.
For children experiencing notable social and/or separation anxiety prior to the onset of COVID-19, treatment took a similar course. This included helping the child to identify thoughts and feelings associated with anxiety, generate and practice coping skills to manage anxiety, create a fear hierarchy, and engage in exposure exercises. In some cases, certain elements of treatment were emphasized over others. For example, for the child with social anxiety and pronounced distress over online learning, ASD-related social communication difficulties made it challenging for her to articulate specific thoughts and feelings associated with her distress. Still, she was able to associate online learning with having an “uncomfortable” feeling in her body, and thus relaxation exercises, such as deep breathing, proved to be a helpful strategy for reducing anxious feelings when they arose. Other key components of treatment included exposure exercises in which the amount of time in the virtual classroom was gradually increased (see “Adapting Exposures” section). Work with the child’s parents focused on helping them calmly respond to their child’s anxiety, as well as to use encouragement, praise, and planned rewards to promote her use of coping skills and engagement in exposures.
Developing and Conducting Exposure Exercises
The key component of CBT for anxiety, the exposure exercises, also had to be modified to fit the telehealth platform, as conducting these exposures in sessions with the therapist as a guide was often no longer feasible. The case of the girl with anxiety induced by attending online school provides a good example. At the outset of therapy, the child’s rate of online school attendance varied from 0 to 2 h per day, with an average of 30–45 min of attendance out of a 4-h school day. Whenever she attended, she disabled the video feature and never spoke without being called on by the teacher. To address this, exposures centered on increasing her attendance and participation (see Table 1).
While it would have been preferable for the child to engage in these exposures with the clinician’s active guidance, attending school online while simultaneously having a video session with the clinician was technologically infeasible. To compensate for the lack of clinician guidance during the exposures, the clinician and child created a detailed plan for the upcoming week’s exposures during each session. These plans included a specific outline for how the child would increase time spent in the virtual classroom, increase use of the video feature, and/or increase voluntary contributions to class discussion. Prior to the beginning of each week, the clinician emailed the family a copy of the plan, which also included strategies for dealing with potential challenges (e.g., coping statements and relaxation exercises to use if anxiety became harder to manage). The child was also advised to rate her subjective units of distress (SUDS) prior to, during, and after the exposure exercise, which she would then later share with the clinician. During online sessions, the clinician also met with the child’s parents individually to discuss with them how to encourage and support her throughout the exposures. With these supports, the child successfully navigated the exposure sequences, and by the end of treatment was attending school online for the entire day nearly every day (nine out of ten days) and utilizing the video feature for about half the length of the school day.
Exposures targeting social anxiety also had to be modified. Prior to COVID-19, in-person sessions regularly included social anxiety exposures, whereby the child and clinician would leave the office so that the child could practice engaging in social interactions with unfamiliar people (e.g., librarian). However, with the onset of COVID-19, not only could children no longer have this in-person guidance from the clinician, but due to social distancing practices, many of the exposures commonly conducted between sessions were not feasible. Typical exposure exercises for social anxiety, such as starting a conversation with a peer, ordering for one’s self in a restaurant and inviting a friend over for a playdate, were no longer possible. As such, exposures requiring children to engage in social interactions were adapted to keep with social distancing guidelines. For several children in our study, such exposures included answering the home telephone, making phone calls or video calls to family members and friends, and calling businesses to ask questions about products or place an order. In particular, for one child with social anxiety, exposure activities included connecting to peers through online video software or video games with a social component (e.g., chat function). In between sessions, the child engaged in these exposures with a variety of same-aged peers that were systematically increased in frequency each week.
Impact of COVID-19 on Daily Life and Family Functioning
In addition to its impact on anxiety, COVID-19 affected the daily functioning of children in ways that needed to be addressed in treatment. Most notably, the stay-at-home and social distancing directives imposed in response to the virus resulted in an enormous shift in everyday routines and family life, requiring children and families to adapt to a new set of life circumstances. Given that adjusting to changes in routine and adapting to novelty constitutes a core area of difficulty for children on the autism spectrum, this shift in everyday circumstances presented a great challenge for many children. For example, for one child who was living at home with his mother and father prior to COVID-19, the pandemic necessitated that his two older sisters move back home which meant more people sharing space and resources, less individualized time with parents, altered meal times to accommodate everyone’s schedules, and less alone/quiet time. In response to these disruptions, the child experienced heightened levels of irritability, verbal outbursts, and oppositional behavior. Relatedly, for most families, the transition from in-person to online schooling, lack of regularly scheduled extracurricular activities, reduced social engagements, and increased time at home meant a loss of structure and access to expected enjoyable activities, often resulting in boredom and frustration.
In response, treatment included working with families to generate strategies and create plans to address these challenges. For example, to help children acclimate to their new daily experiences and create a sense of structure and predictability, families were encouraged to set up a routine for weekdays and to outline a schedule for daily activities. Such schedules usually included designated times for waking up and going to bed, eating meals, doing schoolwork, taking breaks, and relaxing. To help break up the monotony of the school day and staying at home, families were advised to schedule in a variety of fun activities each day. They were also asked to find ways to add in physical activity whenever possible, ranging from five minutes of stretching before breakfast to an afternoon bike ride in a non-crowded area.
The transition to online schooling was also described as a major stressor by parents of children in the study. Regardless of the child’s specific academic programming or grade level, the transition to online schooling typically required children to complete a variety of assignments and activities throughout the day, often necessitating parental involvement. Further, when school went remote, many children in our study lost access to the school-based services they had been receiving (e.g., behavioral support plan, 1:1 aide), and online learning became even more challenging. Parents often had to fulfill the roles of teacher, academic support person, and behavioral specialist to help their children stay on task and complete their schoolwork each day. Additionally, most parents fulfilling these roles had to do so alongside many other competing demands, including carrying out a full day’s work from home, caring for other family members, and managing everyday household responsibilities.
To address the stress conferred by remote schooling, the clinicians and families worked together to make the school day more manageable for both parents and children. In addition to encouraging families to schedule breaks into the school day, the clinicians also helped families set realistic expectations and goals for schoolwork. Often, this included assessing what constituted a manageable amount of work and then communicating with teachers to modify the assignment schedule and/or increase remote supports (e.g., implementing a remote daily check-in with teachers to review and assist with planning of assignments). Parents were also encouraged to find ways to balance competing demands, prioritize the emotional well-being of themselves and their children, and focus on maintaining a calm and supportive family environment. Parents reported this psychological support to be of great value in their own stress reduction.
Lastly, for several children, the uncertainly associated with the future impact and duration of COVID-19 proved to be a significant concern. Questions such as “will anyone we know get sick?”, “when will we be able to see Grandma and Grandpa again?”, and “how long until I go to school again?” could rarely be answered definitively, often resulting in distress and continued questioning and perseveration on the topics. In response to children’s difficulty tolerating uncertainty associated with COVID-19 and its lasting effects on daily life, parents were advised to answer honestly and provide information about both the unknown and known (e.g., “Right now, no one knows when school is going to re-open, but your principal and teachers are trying to figure it out together. We do know that it will not be before September.”) Similarly, parents were advised to assure their children that they would pass on information as it becomes available (e.g., “As soon as the school gives us more information, I will let you know”).
Transition from In-Person to Telehealth Treatment Delivery
Prior to COVID-19, all CBT sessions were conducted in person in the format of weekly individual therapy sessions. Following the stay-at-home directives, treatment was transitioned to telehealth via Zoom, using the HIPAA-compliant version of this videoconferencing platform. This transition required ensuring adequate online security, acclimating children and families to Zoom, and modifying treatment components that required in-person interactions (e.g., therapist-guided exposures). Notably, key features of treatment, including session length and frequency and division of sessions into both child- and parent-focused components, were maintained to ensure comparability with in-person treatment delivery.
To ensure security of the videoconferencing platform used in our study, clinicians used a university-approved HIPAA-compliant version of Zoom, which was maintained and updated by the University IT services. Additional security features included requiring a password for each Zoom session and using a waiting room to screen and admit participants. Initial meetings prior to the first online session were conducted with parents via phone to discuss feasibility of online sessions (e.g., access to technology, availability of a quiet and private space for sessions). Following this phone call, all parents in our study agreed to participate in online treatment.
The first online session included an overview of treatment via telehealth including an explanation of Zoom functionality as needed and finding a private and convenient place at home for sessions so that confidentiality could be maintained. After presenting this information, the clinician gauged children’s and parents’ levels of comfort with using the platform and enabling the camera function during sessions. Questions and concerns were reviewed and discussed, following which all parents and children in the study agreed to participate in online treatment.
Challenges and Opportunities of Telehealth for Treatment of Anxiety in ASD
The transition from in-person treatment to telehealth was associated with both advantages and disadvantages, many of which differed among families. One key advantage was that children often appeared more comfortable engaging with clinicians from the familiarity of their home environment. Relatedly, while in their homes, children could more easily share aspects of their daily lives and interests by showing the clinicians different parts of their physical environment over video (e.g., favorite stuffed animal, personal artwork). Not only did such sharing allow children to feel more connected to the clinician and strengthen rapport, but children’s sharing of their physical environment also allowed the clinicians to learn more about the children and families than is often possible during in-person sessions. Another more pragmatic advantage of the transition from in-person treatment to telehealth was more flexibility in scheduling sessions. Not surprisingly, average weekly session attendance increased following the transition from in-person to remote delivery of treatment.
Conducting treatment via telehealth was also associated with a number of challenges that we had to learn to address. Despite the new opportunities for children to share aspects of their home life with clinicians, common rapport-building activities of child therapy, such as drawing or working on a puzzle, were not readily translatable to remote work. Instead, we asked children to talk about their favorite toys or apps as a way of facilitating interactions and building rapport. Relatedly, the clinicians were no longer able to use visual aids, such as handouts and worksheets, in the same way they could have during in-person sessions. However, given the utility and importance of visual aids in conducting CBT with children on the autism spectrum, the clinicians made use of session handouts either via the “screen sharing” feature on Zoom or by sending electronic copies of handouts to families so that they could follow along during sessions. In addition, at the end of sessions, clinicians emailed summaries of concepts and plans that had been discussed (steps for managing child anxiety, list of coping strategies), as well as any behavior tracking forms for children or parents to complete prior to the next session.
Another challenge associated with telehealth involved the often-distracting nature of the home environment. While asking a child about his or her favorite toy was often useful for starting a conversation, it sometimes resulted in the child becoming distracted from the session. For example, one child, after showing the clinician his favorite action figure, proceeded to step away from the video camera and search his house for all of his other action figures, despite efforts from the clinician to bring him back to the screen. Additional common distractors for both children and parents included other family members inadvertently walking in on sessions, noises from other parts of the house, and, especially for parents, the presence of competing demands (e.g., attending to siblings, checking on dinner). To address these challenges, families were asked to find a location for sessions that had fewer distractions and to remove distracting items (e.g., cell phones) from the room. In addition, a plan was discussed at the outset of each session, and, when necessary, this included placing a clear time limit on unstructured rapport building activities. Lastly, families were asked to schedule sessions at times which would minimize presence of competing demands.
Other challenges for online therapy were conferred by symptoms of autism. For example, one child with significant social communication impairments experienced much greater difficulty engaging in conversation on Zoom. He often seemed to forget that he was talking to the clinician and became fascinated by the video of himself that appeared in the corner of the Zoom screen. Whenever possible, his mother was present during the child portion of the sessions to scaffold his engagement with the clinician and redirect him back to the conversation. The child portions were also limited in length so as to not overburden him. Lastly, to keep him from getting distracted by the video of himself, his mother covered up the portion of the screen displaying his image so that he could shift his focus to the video of the clinician.
Two other children presented with clear deterioration in social reciprocity during video-sessions. Following the transition from in-person to online sessions, these children’s tendency to engage in one-sided conversations and talk over the clinician increased. For example, when one child with separation-related anxiety was asked how his exposure exercise the previous week had gone, the child provided a very brief description of the exposure and then proceeded to give the clinician a detailed description of his favorite video game while ignoring verbal and nonverbal cues from the clinician to redirect the conversation back to the exposure exercise. In this and other similar instances, the child seemed to respond to the video image of the clinician more as if it were a static image rather than a live feed of another person. To address this challenge, at the outset of each session, the clinician laid out clear steps for the back-and-forth communication that would happen during the video session, including giving examples of reciprocal conversation (e.g., “I will ask you if you are still worried about mom going to the grocery store without you. After you tell me about that, I will ask you how it was when she last went without you. After you tell me about that, I will ask you to show me the picture that your mother said you drew of her in the grocery store and ask you what you like the most about your picture”). Once again, the children’s parents were included in the child portion of the sessions in order to help facilitate the children’s ability to participate in a back-and-forth conversation with the clinician.
For one child with prominent social anxiety, anxiety surrounding the use of the video feature on Zoom interfered with his ability to engage with the clinician via telehealth. Prior to the onset of COVID-19 and the transition to telehealth, the child had participated in in-person sessions with the clinician for two months. While he was generally reserved during those sessions, he was able to engage with the clinician in person for about 15 min at a time. However, following the transition to telehealth, the child became exceedingly withdrawn and visibly nervous to talk to the clinician over video. During initial sessions, he was typically unable to engage for more than a few minutes before becoming anxious and leaving the room. To address this issue and increase his comfort with engaging via the online platform, the clinician advised him and his mother to practice using Zoom with other family members between sessions. In addition, since the child often became anxious because he did not “know what to say” during sessions, at the end of each session the clinician and he would discuss the topic of the next session so that he could prepare a few thoughts ahead of time.
Discussion
In this commentary, we have described our experience of transitioning to remote delivery of CBT for anxiety in autism for children who were enrolled in a clinical trial at the beginning of the COVID-19 pandemic. As we adapted and modified the delivery of CBT to the telehealth format, our patients' ASD characteristics required careful consideration. We were attentive to the unique challenges posed by children’s social communication deficits, in particular. We were also mindful that the anxieties associated with unprecedented stressors and changes brought about by the COVID-19 pandemic were experienced in various unique ways by our patients with ASD and their parents. Our clinicians were able to make use of the flexibility inherent in CBT to modify treatment goals to the emergence of new sources of anxiety for some children, such as contamination risk or virtual schooling, or to the sudden elimination of sources of pre-existing anxiety, such as separation anxiety or social anxiety with peers, for others. We also modified CBT exposure exercises as needed to accommodate the new reality of quarantine restrictions. In addition, we expanded the content of parent-focused components to include goals related to decreasing stresses inherent in working and schooling from home. Finally, our clinicians adapted the telehealth modality of treatment delivery to fit the new limitations imposed by remote videoconferencing. Despite considerable challenges in delivering CBT via telehealth, we had no attrition of patients. In fact, there were new opportunities for rapport building and parents found scheduling more convenient.
While telehealth interventions for children with ASD have been the subject of promising research before the pandemic occurred, most existing interventions have been delivered to only parents or teachers, and not directly to children with ASD (Knutsen et al. 2016; Sutherland et al. 2018). Only one study to date has investigated the remote delivery of a CBT intervention that includes direct online interaction with children with ASD. Hepburn et al. (2016) adapted a group-based CBT intervention to a videoconferencing platform, targeting anxiety symptoms in youth with comorbid ASD and anxiety disorders. Treatment was delivered to parent–child dyads, and pilot data showed high acceptability and promising preliminary efficacy results. Clinicians reported several challenges of remote delivery, including reduced opportunities for behavioral observation and reduced ability to support exposure activities. Given the reality that present or future circumstances may require the widespread utilization of telehealth for treating anxiety in children with ASD, we hope that this commentary can be informative for clinicians and researchers working with children on the autism spectrum in either clinical or research settings.
Ultimately, we believe that when approached with flexibility and fidelity, the delivery of CBT for anxiety in ASD via telehealth is not only possible but also presents unexpected opportunities and benefits for tailoring treatment to better serve the needs of children with ASD as we move forward beyond the COVID-19 Pandemic.
References
Aman, M. G., & Pearson, D. A. (2020). Challenges for child and adolescent psychiatric research in the era of COVID-19. Journal of Child and Adolescent Psychopharmacology, 30(5), 280–284. https://doi.org/10.1089/cap.2020.0081.
Chen, I. H., Chen, C.-Y., Pakpour, A. H., Griffiths, M. D., & Lin, C.-Y. (2020). Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. Journal of the American Academy of Child and Adolescent Psychiatry. https://doi.org/10.1016/j.jaac.2020.06.007.
Fegert, J. M., Vitiello, B., Plener, P. L., & Clemens, V. (2020). Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14, 20. https://doi.org/10.1186/s13034-020-00329-3.
Hepburn, S. L., Blakeley-Smith, A., Wolff, B., & Reaven, J. A. (2016). Telehealth delivery of cognitive-behavioral intervention to youth with autism spectrum disorder and anxiety: A pilot study. Autism, 20(2), 207–218. https://doi.org/10.1177/1362361315575164.
Jurcik, T., Jarvis, G. E., Zeleskov Doric, J., Krasavtseva, Y., Yaltonskaya, A., Ogiwara, K., et al. (2020). Adapting mental health services to the COVID-19 pandemic: Reflections from professionals in four countries. Counselling Psychology Quarterly. https://doi.org/10.1080/09515070.2020.1785846.
Knutsen, J., Wolfe, A., Burke, B. L., Hepburn, S., Lindgren, S., & Coury, D. (2016). A systematic review of telemedicine in autism. Review Journal of Autism and Developmental Disorders, 3(4), 330–344. https://doi.org/10.1007/s40489-016-0086-9.
Lai, M. C., Kassee, C., Besney, R., Bonato, S., Hull, L., Mandy, W., et al. (2019). Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. The Lancet Psychiatry, 6(10), 819–829. https://doi.org/10.1016/S2215-0366(19)30289-5.
Lee, J. (2020). Mental health effects of school closures during COVID-19. The Lancet Child and Adolescent Health, 4(6), 421. https://doi.org/10.1016/s2352-4642(20)30109-7.
Morrissette, M. (2020). School closures and social anxiety during the COVID-19 pandemic. Journal of the American Academy of Child and Adolescent Psychiatry. https://doi.org/10.1016/j.jaac.2020.08.436.
Payne, L., Flannery, H., Kambakara Gedara, C., Daniilidi, X., Hitchcock, M., Lambert, D., et al. (2020). Business as usual? Psychological support at a distance. Clinical Child Psychology and Psychiatry, 25(3), 672–686. https://doi.org/10.1177/1359104520937378.
Perihan, C., Burke, M., Bowman-Perrott, L., Bicer, A., Gallup, J., Thompson, J., & Sallese, M. (2020). Effects of cognitive behavioral therapy for reducing anxiety in children with high functioning ASD: A systematic review. Journal of Autism and Developmental Disorders, 50(6), 1958–1972. https://doi.org/10.1007/s10803-019-03949-7.
Perrin, P. B., Rybarczyk, B. D., Pierce, B. S., Jones, H. A., Shaffer, C., & Islam, L. (2020). Rapid telepsychology deployment during the COVID-19 pandemic: A special issue commentary and lessons from primary care psychology training. Journal of Clinical Psychology, 76(6), 1173–1185. https://doi.org/10.1002/jclp.22969.
RUPP Anxiety Study Group. (2002). The Pediatric Anxiety Rating Scale (PARS): Development and psychometric properties. Journal of the American Academy of Child and Adolescent Psychiatry, 41(9), 1061–1069.
Sharma, A., Sasser, T., Schoenfelder Gonzalez, E., Vander Stoep, A., & Myers, K. (2020). Implementation of home-based telemental health in a large child psychiatry department during the COVID-19 crisis. Journal of child and adolescent psychopharmacology. https://doi.org/10.1089/cap.2020.0062.
Silverman, W. K., & Albano, A. M. (1996). Anxiety disorders interview schedule for DSM-IV. Child Version: Oxford University Press.
SPARK. (2020). Impact of COVID-19 on families and children with autism. New York: Simons Foundation.
Sukhodolsky, D. G. (2020). CBT for anxiety in children with autism. Retrieved from https://www.clinicaltrials.gov/ct2/show/NCT02725619. Accessed 6 Oct 2020
Sutherland, R., Trembath, D., & Roberts, J. (2018). Telehealth and autism: A systematic search and review of the literature. International Journal of Speech-Language Pathology, 20(3), 324–336. https://doi.org/10.1080/17549507.2018.1465123.
Wood, J. J., Drahota, A., Sze, K., Har, K., Chiu, A., & Langer, D. A. (2009). Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 50(3), 224–234.
Wood, J. J., Kendall, P. C., Wood, K. S., Kerns, C. M., Seltzer, M., Small, B. J., et al. (2020). Cognitive behavioral treatments for anxiety in children with autism spectrum disorder: A randomized clinical trial. JAMA Psychiatry, 77(5), 473–484. https://doi.org/10.1001/jamapsychiatry.2019.4160.
YoungMinds. (2020). Coronavirus: Impact on young people with mental health needs; survey 2: summer 2020. London: YoungMinds.
Acknowledgments
Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Grant No. R01HD083881 (DGS). CBK and KI are Fellows of the Translational Developmental Neuroscience Training Program (National Institute of Mental Health, Grant No. T32 MH18268) directed by Dr. Michael Crowley.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception or design of the work; drafted the work or revised it critically for important intellectual content; and approved the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Sukhodolsky receives royalties from Guilford Press for a treatment manual on CBT for anger and aggression in children. Drs. Wood developed the CBT program for autism and anxiety discussed herein; this program is available free of charge on the internet and the authors have no financial conflict of interest associated with it. Other authors (CBK, RPJ, SNR, AW, and KI) have no biomedical financial interests or potential conflict of interest to declare related to this present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kalvin, C.B., Jordan, R.P., Rowley, S.N. et al. Conducting CBT for Anxiety in Children with Autism Spectrum Disorder During COVID-19 Pandemic. J Autism Dev Disord 51, 4239–4247 (2021). https://doi.org/10.1007/s10803-020-04845-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-020-04845-1