Abstract
Objectives
To evaluate the effect of Nd:YAG laser irradiation as a prior desensitizing strategy on immediate and medium-term microtensile bond strength (µTBS) to simulated hypersensitive dentin.
Materials and methods
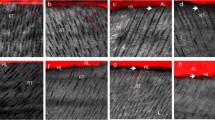
Flat mid-coronal dentin was obtained from third molars and submitted to a 600-grit SiC paper (1 min; N: normal dentin) or subsequently challenged with citric acid (6%, 1 min; H: simulated hypersensitive dentin). Afterwards, dentin was or was not (C: control; HC, NC — each n = 7) irradiated with Nd:YAG laser (L: laser; 1.0 W/10 Hz/100 mJ/4 irradiations of 50-60 s; HL, NL — each n = 7). A 2-step self-etch adhesive (Clearfil SE Bond) was applied and composite (Filtek Z350) buildups were constructed. After 24-h (distilled water/37 °C) storage, specimens were sectioned into beams and tested (µTBS; 0.5 mm/min) immediately or after 6-month aging. Three-way ANOVA and Tukey tests were applied (α = 0.05). Qualitative evaluation of the adhesive interface (n = 1 extra tooth per group) was performed by Confocal Laser Scanning Microscopy.
Results
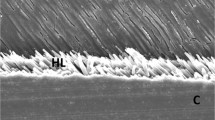
Substrate condition (p < 0.001), laser irradiation (p < 0.001), and aging (p = 0.002) influenced the results. Furthermore, there was interaction between substrate and irradiation (p < 0.001). Laser irradiation favored µTBS exclusively to hypersensitive dentin immediately and after aging. µTBS to hypersensitive dentin was higher than that to the normal substrate only when it was laser-irradiated. In any case, immediate µTBS was always higher than that after aging. CLSM revealed longer and more numerous resin tags for simulated hypersensitive dentin, and shorter and fewer resin tags for laser-irradiated dentin. No differences were observed in the hybrid layer itself.
Conclusion
Nd:YAG laser irradiation prior to restoration favored the µTBS of a self-etch adhesive and resin composite to hypersensitive dentin.
Clinical relevance
Desensitizing strategies are usually tried before performing restorative treatments in hypersensitive dentin; therefore, they may influence behavior of the adhesive interface established. However, instead of causing concern, Nd:YAG laser irradiation revealed a favorable effect on the aforementioned interface.

Similar content being viewed by others
References
Gillam DG (1995) Mechanisms of stimulus transmission across dentin–a review. J West Soc Periodontol Periodontal Abstr 43:53–65
Brannstrom M, Astrom A (1972) The hydrodynamics of the dentine; its possible relationship to dentinal pain. Int Dent J 22:219–227
Orchardson R, Gillam DG (2006) Managing dentin hypersensitivity. J Am Dent Assoc 137:990–998. https://doi.org/10.14219/jada.archive.2006.0321
Pashley DH (1986) Dentin permeability, dentin sensitivity, and treatment through tubule occlusion. J Endod 12:465–474. https://doi.org/10.1016/S0099-2399(86)80201-1
Duran I, Sengun A (2004) The long-term effectiveness of five current desensitizing products on cervical dentine sensitivity. J Oral Rehabil 31:351–356. https://doi.org/10.1046/j.1365-2842.2003.01241.x
Pamir T, Dalgar H, Onal B (2007) Clinical evaluation of three desensitizing agents in relieving dentin hypersensitivity. Oper Dent 32:544–548. https://doi.org/10.2341/07-5
Schmidlin PR, Sahrmann P (2013) Current management of dentin hypersensitivity. Clin Oral Investig 17:55–59. https://doi.org/10.1007/s00784-012-0912-0
Rezazadeh F, Dehghanian P, Jafarpour D (2018) Laser effects on the prevention and treatment of dentinal hypersensitivity: a systematic review. J Lasers Med Sci 10(1):11. https://doi.org/10.15171/jlms.2019.01
Xiao S, Liang K, Liu H et al (2017) Effect of water-cooled Nd:YAG laser on dentinal tubule occlusion in vitro. Photomed Laser Surg 35:98–104. https://doi.org/10.1089/pho.2016.4169
Kimura Y, Wilder-Smith P, Yonaga K et al (2000) Treatment of dentine hypersensitivity by lasers: a review. J Clin Periodontol 27:715–721. https://doi.org/10.1034/j.1600-051x.2000.027010715.x
Aranha ACC, Domingues FB, Franco VO et al (2005) Effects of Er:YAG and Nd:YAG lasers on dentin permeability in root surfaces: a preliminary in vitro study. Photomed Laser Surg 23:504–508. https://doi.org/10.1089/pho.2005.23.504
Gholami GA, Fekrazad R, Esmaiel-Nejad A et al (2011) An evaluation of the occluding effects of Er;Cr:YSGG, Nd:YAG, CO 2 and diode lasers on dentinal tubules: a scanning electron microscope in vitro study. Photomed Laser Surg 29:115–121. https://doi.org/10.1089/pho.2009.2628
Birang R, Poursamimi J, Gutknecht N et al (2007) Comparative evaluation of the effects of Nd:YAG and Er:YAG laser in dentin hypersensitivity treatment. Lasers Med Sci 22:21–24. https://doi.org/10.1007/s10103-006-0412-z
Kara C, Orbak R (2009) Comparative evaluation of Nd:YAG laser and fluoride varnish for the treatment of dentinal hypersensitivity. J Endod 35:971–974. https://doi.org/10.1016/j.joen.2009.04.004
Lopes AO, Aranha ACC (2013) Comparative evaluation of the effects of Nd:YAG laser and a desensitizer agent on the treatment of dentin hypersensitivity: a clinical study. Photomed Laser Surg 31:132–138. https://doi.org/10.1089/pho.2012.3386
George AA, Muruppel AM, Sudeep S et al (2019) A comparative evaluation of the effectiveness of three different modalities in occluding dentinal tubules: an in vitro study. J Contemp Dent Pract 20:454–459. https://doi.org/10.5005/jp-journals-10024-2538
Liu HC, Lin CP, Lan WH (1997) Sealing depth of Nd:YAG laser on human dentinal tubules. J Endod 23:691–693. https://doi.org/10.1016/S0099-2399(97)80403-7
Al-Sabbagh M, Brown A, Thomas MV (2009) In-office treatment of dentinal hypersensitivity. Dent Clin North Am 53:47–60. https://doi.org/10.1016/j.cden.2008.11.003
Ianzano JA, Gwinnett AJ, Westbay G (1993) Polymeric sealing of dentinal tubules to control sensitivity: preliminary observations. Periodontal Clin Investig 15:13–16
Schupbach P, Lutz F, Finger WJ (1997) Closing of dentinal tubules by Gluma desensitizer. Eur J Oral Sci 105:414–421. https://doi.org/10.1111/j.1600-0722.1997.tb02138.x
Kakaboura A, Rahiotis C, Thomaidis S et al (2005) Clinical effectiveness of two agents on the treatment of tooth cervical hypersensitivity. Am J Dent 18:291–295
Brahmbhatt N, Neeta B, Sahayata V et al (2012) A double blind controlled trial comparing three treatment modalities for dentin hypersensitivity. Med Oral Patol Oral Cir Bucal 17:e483–e490. https://doi.org/10.4317/medoral.17594
Pei D, Meng Y, Li Y et al (2019) Influence of nano-hydroxyapatite containing desensitizing toothpastes on the sealing ability of dentinal tubules and bonding performance of self-etch adhesives. J Mech Behav Biomed Mater 91:38–44. https://doi.org/10.1016/j.jmbbm.2018.11.021
Aranha ACC, Siqueira Junior ADS, Cavalcante LMA et al (2006) Microtensile bond strengths of composite to dentin treated with desensitizer products. J Adhes Dent 8:85–90
Kobler A, Schaller HG, Gernhardt CR (2008) Effects of the desensitizing agents Gluma and Hyposen on the tensile bond strength of dentin adhesives. Am J Dent 21:388–392
Sailer I, Tettamanti S, Stawarczyk B et al (2010) In vitro study of the influence of dentin desensitizing and sealing on the shear bond strength of two universal resin cements. J Adhes Dent 12:381–392. https://doi.org/10.3290/j.jad.a17714
Külünk Ş, Saraç D, Külünk T et al (2011) The effects of different desensitizing agents on the shear bond strength of adhesive resin cement to dentin. J Esthet Restor Dent 23:380–387. https://doi.org/10.1111/j.1708-8240.2011.00415.x
Ravikumar N, Shankar P, Indira R (2011) Shear bond strengths of two dentin bonding agents with two desensitizers: an in vitro study. J Conserv Dent 14:247–251. https://doi.org/10.4103/0972-0707.85802
Bhatia S, Krishnaswamy MM (2012) Effect of two different dentin desensitizers on shear bond strength of two different bonding agents to dentin: an in vitro study. Indian J Dent Res 23:703–708. https://doi.org/10.4103/0970-9290.111242
Sabatini C, Wu Z (2015) Effect of desensitizing agents on the bond strength of mild and strong self-etching adhesives. Oper Dent 40:548–557. https://doi.org/10.2341/14-190-L
Muñoz MA, Luque I, Hass V et al (2013) Immediate bonding properties of universal adhesives to dentine. J Dent 41:404–411. https://doi.org/10.1016/j.jdent.2013.03.001
Pereira JC, Segala AD, Gillam DG (2005) Effect of desensitizing agents on the hydraulic conductance of human dentin subjected to different surface pre-treatments–an in vitro study. Dent Mater 21:129–138. https://doi.org/10.1016/j.dental.2004.02.007
Shellis RP, Curtis AR (2010) A minimally destructive technique for removing the smear layer from dentine surfaces. J Dent 38:941–944. https://doi.org/10.1016/j.jdent.2010.07.009
Raafat Abdelaziz R, Mosallam RS, Yousry MM (2011) Tubular occlusion of simulated hypersensitive dentin by the combined use of ozone and desensitizing agents. Acta Odontol Scand 69:395–400. https://doi.org/10.3109/00016357.2011.572290
Lopes AO, de Paula EC, Aranha ACC (2017) Evaluation of different treatment protocols for dentin hypersensitivity: an 18-month randomized clinical trial. Lasers Med Sci 32:1023–1030. https://doi.org/10.1007/s10103-017-2203-0
Armstrong S, Breschi L, Özcan M et al (2017) Academy of Dental Materials guidance on in vitro testing of dental composite bonding effectiveness to dentin/enamel using micro-tensile bond strength (μTBS) approach. Dent Mater 33:133–143. https://doi.org/10.1016/j.dental.2016.11.015
Bim Júnior O, Cebim MA, Atta MT et al (2017) Determining optimal fluorescent agent concentrations in dental adhesive resins for imaging the tooth/restoration interface. Microsc Microanal 23:122–130. https://doi.org/10.1017/S143192761601271X
Matos AB, Oliveira DC, Kuramoto M et al (1999) Nd:YAG laser influence on sound dentin bond strength. J Clin Laser Med Surg 17:165–169. https://doi.org/10.1089/clm.1999.17.165
Anić I, Šegović S, Katanec D et al (1998) Scanning electron microscopic study of dentin lased with argon, CO2, and Nd:YAG laser. J Endod 24:77–81. https://doi.org/10.1016/S0099-2399(98)80081-2
Ariyaratnam MT, Wilson MA, Blinkhorn AS (1999) An analysis of surface roughness, surface morphology and composite/dentin bond strength of human dentin following the application of the Nd:YAG laser. Dent Mater 15:223–228. https://doi.org/10.1016/S0109-5641(99)00035-4
Lan WH, Chen KW, Jeng JH et al (2000) A comparison of the morphological changes after Nd-YAG and CO2 laser irradiation of dentin surfaces. J Endod 26:450–453. https://doi.org/10.1097/00004770-200008000-00005
Türkmen C, Günday M, Karaçorlu M et al (2000) Effect of CO2, Nd:YAG, and ArF excimer lasers on dentin morphology and pulp chamber temperature: an in vitro study. J Endod 26:644–648. https://doi.org/10.1097/00004770-200011000-00003
Sazak H, Türkmen C, Günday M (2001) Effects of Nd: YAG laser, air-abrasion and acid-etching on human enamel and dentin. Oper Dent 26:476–481
Ghiggi PC, Dall Agnol RJC, Burnett LH et al (2010) Effect of the Nd:YAG and the Er:YAG laser on the adhesive-dentin interface: a scanning electron microscopy study. Photomed Laser Surg 28:195–200. https://doi.org/10.1089/pho.2009.2530
Kurt S, Kırtıloğlu T, Yılmaz NA et al (2018) Evaluation of the effects of Er:YAG laser, Nd:YAG laser, and two different desensitizers on dentin permeability: in vitro study. Lasers Med Sci 33:1883–1890. https://doi.org/10.1007/s10103-018-2546-1
Resende RF, Arantes BF, Palma-Dibb RG et al (2019) Influence of Er, Cr:YSGG laser on dentin acid resistance after erosive challenge. Am J Dent 32:215–218
Paranhos MPG, Spohr AM, Marcondes M et al (2009) Influence of Nd:YAG laser irradiation on microtensile bond strength of adhesive systems to sound or carious dentin. Quintessence Int 40:145–153
Schaller H-G, Weihing TS Jr (1997) Permeability of dentine after Nd:YAG laser treatment: an in vitro study. J Oral Rehabil 24:274–281. https://doi.org/10.1046/j.1365-2842.1997.d01-290.x
Matos AB, Oliveira DC, Navarro RS et al (2000) Nd:YAG laser influence on tensile bond strength of self-etching adhesive systems. J Clin Laser Med Surg 18:253–257. https://doi.org/10.1089/clm.2000.18.253
Oda M, Oliveira DC, Liberti EA (2001) Morphologic evaluation of the bonding between adhesive/composite resin and dentin irradiated with Er:YAG and Nd:YAG lasers: comparative study using scanning microscopy. Pesqui Odontol Bras 15:283–289. https://doi.org/10.1590/S1517-74912001000400003
de Penha KJ, S, Torres CRG, Tavarez RRDJ, et al (2020) Interaction effect of Nd:YAG laser and universal adhesive system for dentin sealing. J Clin Exp Dent 12:e1124–e1130. https://doi.org/10.4317/jced.57306
Kobayashi C, Fujishima A, Miyazaki T et al (2003) Effect of Nd:YAG laser irradiation on shear bond strength of glass-ionomer luting cement to dentin surface. Int J Prosthodont 16:493–498
Lan WH, Lee BS, Liu HC et al (2004) Morphologic study of Nd:YAG laser usage in treatment of dentinal hypersensitivity. J Endod 30:131–134. https://doi.org/10.1097/00004770-200403000-00001
Sartori N, Peruchi LD, Phark JH et al (2016) The influence of intrinsic water permeation on different dentin bonded interfaces formation. J Dent 48:46–54. https://doi.org/10.1016/j.jdent.2016.03.005
Maximiano V, Machado AC, Lopes RM et al (2021) Association of Nd:YAG laser and calcium-phosphate desensitizing pastes on dentin permeability and tubule occlusion. J Appl Oral Sci 29:e20200736. https://doi.org/10.1590/1678-7757-2020-0736
Moriyama EH, Zângaro RA, Villaverde AB et al (2004) Dentin evaluation after Nd:YAG laser irradiation using short and long pulses. J Clin Laser Med Surg 22:43–50. https://doi.org/10.1089/104454704773660967
Maximiano V, Machado AC, Yoshida ML et al (2019) Nd:YAG laser and calcium sodium phosphosilicate prophylaxis paste in the treatment of dentin hypersensitivity: a double-blind randomized clinical study. Clin Oral Investig 23:3331–3338. https://doi.org/10.1007/S00784-018-2759-5
Yoshida Y, Nagakane K, Fukuda R et al (2004) Comparative study on adhesive performance of functional monomers. J Dent Res 83:454–458. https://doi.org/10.1177/154405910408300604
Sakano W, Nakajima M, Prasansuttiporn T et al (2013) Polymerization behavior within adhesive layer of one- and two-step self-etch adhesives: a micro-Raman spectroscopic study. Dent Mater J 32:992–998. https://doi.org/10.4012/dmj.2013-095
Benitez Sellan PL, Zanatta RF, Gomes Torres CR et al (2020) Effects of calcium-phosphate, laser and adhesive on dentin permeability and bond strength. Heliyon 6:e03925. https://doi.org/10.1016/j.heliyon.2020.e03925
Ladalardo TCCGP, Pinheiro A, Campos RADC et al (2004) Laser therapy in the treatment of dentine hypersensitivity. Braz Dent J 15:144–150. https://doi.org/10.1590/s0103-64402004000200011
Hossain M, Nakamura Y, Kimura Y et al (2001) Effect of pulsed Nd:YAG laser irradiation on acid demineralization of enamel and dentin. J Clin Laser Med Surg 19:105–108. https://doi.org/10.1089/104454701750285421
de Almeida L, de FD, Cavalcanti YW, (2015) Effect of collagen matrix saturation on the surface free energy of dentin using different agents. J Contemp Dent Pract 16:531–536. https://doi.org/10.5005/jp-journals-10024-1717
Breschi L, Mazzoni A, Nato F et al (2010) Chlorhexidine stabilizes the adhesive interface: a 2-year in vitro study. Dent Mater 26:320–325. https://doi.org/10.1016/j.dental.2009.11.153
Tabatabaei MH, Chiniforush N, Hashemi G et al (2018) Efficacy comparison of Nd:YAG laser, diode laser and dentine bonding agent in dentine hypersensitivity reduction: a clinical trial. Laser Ther 27:265–270. https://doi.org/10.5978/islsm.27_18-OR-24
Bellal S, El FR, Mehta A et al (2021) Efficacy of near infrared dental lasers on dentinal hypersensitivity: a meta-analysis of randomized controlled clinical trials. Lasers Med Sci. https://doi.org/10.1007/S10103-021-03391-1
Sano H, Chowdhury AFMA, Saikaew P et al (2020) The microtensile bond strength test: its historical background and application to bond testing. Jpn Dent Sci Rev 56:24–31. https://doi.org/10.1016/J.JDSR.2019.10.001
Acknowledgements
The authors thank Dr. Taís Scaramucci, of the Department of Operative Dentistry — School of Dentistry/University of São Paulo, and Mario Costa Cruz, of the Center for Research Support Facilities (CEFAP) — University of São Paulo, for their support with the statistical analysis and Confocal Laser Scanning Microscopy (CLSM) imaging, respectively.
Funding
This work was supported in part by the National Council for Scientific and Technological Development (CNPq), Brazil (USR Scholarship 152038/2015–9). Funding source had no involvement in study design; collection, analysis, and interpretation of data; writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Karin Landmayer contributed to conception, design, data acquisition, analysis, and interpretation. Juliana Costa Veiga da Silva and Brunna Haddad Anhesini contributed to conception, design, and mainly to data acquisition by working at the lab. Bruna de Oliveira Iatarola and Ana Cecília Correa Aranha contributed to conception and design. Finally, Luciana F. Francisconi-dos-Rios advised the first authors in conducting the entire project, being responsible for conception, design, data acquisition, analysis, and interpretation. All authors drafted and critically revised the manuscript, in addition to reading and approving the final version. All of them guarantee the accuracy and integrity of all parts of the work.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Ethics Committee on Research (with human beings) approved the study providing the following protocol and assent numbers (CAAE 44486815.3.0000.0075; research project approval: assent #1.070.764; final report/results approval: assent #3.141.302).
Consent to participate
For this type of study, individual formal consent is not required. The Coordinator of the Human Teeth Bank (Permanent Teeth Division) of the main author’s institution signed an applicable declaration of commitment to provide fifty healthy, extracted human third molars, for the purpose of conducting the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Landmayer, K., da Silva, J.C.V., Anhesini, B.H. et al. Effect of Nd:YAG laser irradiation, used as a desensitizing strategy, on bond strength to simulated hypersensitive dentin. Clin Oral Invest 26, 4109–4116 (2022). https://doi.org/10.1007/s00784-022-04380-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04380-6