Abstract
Background
Internal carotid artery (ICA) is predominant localization of giant intracranial aneurysms (GIAs). The rupture of GIA is supposed to be related to higher risk of poor clinical outcome. Although endovascular techniques are still being developed, they seem to be unsatisfactory in the mean of GIAs.
Methods
Included in the retrospective analysis were 78 giant and 250 smaller surgically treated ICA aneurysms. Exclusion criteria were multiple and blood blister-like aneurysms. Neurological deficit on admission, clinical and radiological presentation, gender, age, segment of ICA, surgical methods, accessory techniques and complications were analyzed. Death rate and short- and long-term outcome of giant aneurysms were compared with smaller aneurysms and risk factors for mortality, unfavorable short- and long-term outcome were determined.
Results
There was no difference in general and surgical complications between ICA aneurysm size groups, as well as in occurrence of newly diagnosed neurological deficit after the operation. There were similar mortality rates, proportion of unfavorable outcome, and low health related quality of life for giant and smaller aneurysms. A 12.2% death rate for all ICA aneurysms was achieved. Trapping method as well as Fisher grades 3 and 4 increased mortality risk in the smaller aneurysm group. No significant factors were related to an unfavorable outcome in the ruptured giant aneurysm group. Patients older than 65, Hunt-Hess grades 4 and 5, Fisher grade 4, and newly diagnosed deficit after operation were connected with unfavorable outcome in the ruptured smaller aneurysm group. Newly diagnosed neurological deficit was also an unfavorable outcome risk factor in both giant and smaller ICA unruptured aneurysms. No difference was noted in long-term health-related quality of life between the giant and smaller ICA groups. Higher age and presence of concomitant disease were independent factors affecting quality of life, although obtained data were incomplete.
Conclusions
The study breaks the stereotype of unfavorable giant ICA aneurysms treatment results. Mortality rate, short- and long-term outcome after the operation of giant and smaller ICA aneurysms are similar. Higher age, patients’ condition at admission, and the amount of extravasated blood and trapping method are poor prognostic factors in patients with smaller ICA aneurysm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Localization of giant intracranial aneurysms (GIAs) (defined as a dimension exceeding 25 mm [18]) is different compared to smaller ones. Although 20–40% of GIAs are found in posterior circulation, the internal carotid artery (ICA) is the predominant localization of GIAs [16, 17]. Up to 67% of GIAs are localized on the ICA [17].
The etiology of GIAs is similar to the smaller ones [16]. However, apart from the enlargement of small aneurysms, de novo development of GIAs is described [2]. Krings et al. [14] indicate that the formation of GIAs (proximal ICA and vertebral artery) may differ from the others. Repeated subadventitial hemorrhages from the vasa vasorum play an important role in the pathogenesis of GIAs. Therefore, GIAs can be regarded as a “proliferative disease of the vessel wall induced by extravascular activity” [14].
Approximately two-thirds of GIAs are diagnosed before rupture, causing mass effect, while most of the patients with smaller aneurysms are admitted due to subarachnoid hemorrhage (SAH) [17]. Regardless of how thick the wall of the GIA is, rupture causes extravasation of a greater amount of blood than happens in smaller aneurysms [8, 16]. This may result in poor clinical presentation in patients with GIAs. The ISUIA study [29] showed a 40% risk of rupture in case of giant ICA aneurysms. Kassell [9] noticed that the large size of the aneurysm is one of the prognostic factors related to postoperative mortality. The two studies above [9, 29] warrant treatment of both ruptured and unruptured giant ICA aneurysms [4].
Endovascular and surgical techniques are the options considered in treatment of giant ICA aneurysms. Since the first attempt of excluding giant ICA aneurysms from circulatory system in 1885 [5], a great many surgical occlusion and accessory techniques have been developed and described [17]. Current endovascular techniques are regarded as having lower risks for the patient [28]. Despite the fact that these techniques are being constantly developed, in GIAs, these still seem to be unsatisfactory in terms of durability of aneurysm occlusion [24, 28]. Parkinson [23] suggests that the results of surgical techniques should be the “gold standard” with which other techniques, including endovascular treatment, are compared.
Untreated GIAs have a poor natural history, as the mortality rate after 2 years of observation can reach 100% [13, 20, 25]. Even treated, favorable results usually did not exceed 80% in previous series [3, 10, 13, 15, 25, 27].
Reviewing neurosurgical literature regarding methods used for measuring outcome, the Glasgow outcome scale (GOS) and Rankin scale are mostly mentioned. Kim also reported the application of quality-of-life scale SF-36 in the intracranial aneurysm group [12]. Doctor’s and patient’s evaluation of treatment may differ, thus patient’s self-assessment scale should be used [6].
There is not enough data in the literature describing the results of treatment and quality of life in patients with giant ICA in comparison to smaller ones. Surprisingly, factors influencing quality of life several years after operation have not been reported in the ICA aneurysm group. For this reason, the current study was performed to compare the prognosis after treatment of giant and smaller ICA aneurysms as well as to determine which factors influence postoperative mortality, early and long-term outcome separately in patients with giant and smaller type of aneurysm.
Materials and methods
Patient population and data collection
Between 1997 and 2006, 1,035 surgical intracranial saccular aneurysms securing procedures were performed in the Neurosurgery Department at the Medical University of Gdansk in Poland. Angiography and CT scans were analyzed, and surgical results, demographics, and other factors were evaluated retrospectively in 328 cases of saccular ICA aneurysms. The group was selected as 62 multiple and four blood blister-like aneurysms were excluded. GOS was used in patients’ evaluation on the day of discharge. Postoperative mortality (GOS 1) was divided into perioperative (before 48 h) and postoperative (after 48 h after surgery) [19]. In the study, postoperative mortality analysis referred only to the in-hospital period. Favorable short-term outcome was defined as GOS grade 4 and 5, and unfavorable if GOS was 1, 2, or 3. Long-term outcome was assessed using the quality-of-life SF-36 scale. The query was sent to the patients in 2008 or collected during visits. If total SF-36 scores were under 50 points, low health-related quality of life was established.
Patients’ characteristic and condition
The group consisted of 119 (36.28%) small, 81 (24.70%) medium, 50 (15.24%) large and 78 giant (23.78%) ICA aneurysms. For the statistics, small, medium, and large constituted one group of 250 smaller ICA aneurysms.
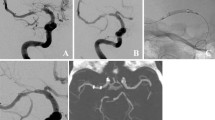
All of the giant aneurysms were operated on by senior author (SP). Over half (n = 42; 53.85%) of the giant ICA aneurysms were diagnosed based on mass effect signs, while 82.40% (n = 206) of the smaller aneurysms were operated on after rupture (p < 0.01) (Fig. 1).
Age of the treated patients ranged from 17 to 83, mean 51.20 (SD ± 12.73). No difference in age was noted between the groups, as for the giant, the mean was 50.53 (SD ± 10.12) and for the smaller ICA aneurysms 51.42 (SD ± 13.46). Female predomination was observed in both groups. There were significantly (p = 0.03) more females (85.90%) in the giant than in the smaller ICA aneurysm group (74.00%). Statistically, the proportion of education and habitation (village/town) was similar in both groups, as well as the percentage of concomitant diseases.
For 242 patients who presented SAH (36 giant and 206 smaller ICA aneurysms), Hunt-Hess, Fisher, GCS, WFNS grading and neurological deficit on admission was assessed. In these regards, the giant group did not differ from the smaller ICA aneurysm group.
In 86 patients with unruptured aneurysm (42 giant and 44 smaller aneurysms), neurological deficit was also assessed on admission. Third nerve paresis was diagnosed on admission in seven patients (15.91%) with smaller ICA aneurysm group. There were 13 smaller ICA aneurysm of PCoA origin, five of them (38.46%) presented oculomotor nerve paresis. All of patients with smaller intracavernous aneurysms (n = 2) had third nerve paresis (Table 1).
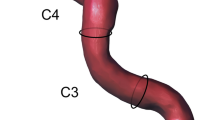
Most (85.71%) of the intracavernous aneurysms were giant, 11 unruptured (all patients were symptomatic) and 1 ruptured (clinical presentation was epistaxis). All smaller intracavernous aneurysms (n = 2) were unruptured. The posterior wall aneurysms (AChA, PCoA) were usually small. One-fourth of the ICA aneurysms were localized in the bifurcation segment. The different localizations of the giant and smaller aneurysms were significant (p < 0.01) (Fig. 2).
Treatment
The surgical methods and accessory techniques used in the treatment of the giant and smaller ICA aneurysms are shown in Table 2. The pterional approach was applied in all cases of giant and smaller, ruptured and unruptured ICA aneurysms. Extraduraly lesser wing of sphenoid bone partial removal and decompression of supraorbital fissure were performed in all cases of pterional craniotomy.
In both of the smaller and the one giant intracavernous aneurysm, direct clipping was performed in deep hypothermic circulatory arrest. In the remaining nine cases of intracavernous aneurysm, high-flow bypass was done.
For all clinoid and ophthalmic artery origin aneurysms, the additionally ipsilateral cervical carotid bifurcation exposure was prepared for proximal ICA control as well as intradural anterior clinoid process removal. When deemed necessary, optic strut removal was performed. In the four cases of clinoid giant aneurysms, retrograde suction was accessory. If the surgeon found that direct clipping impossible, bypass was offered afterwards. Unfortunately, in four cases, low-flow by-passes (STA-MCA and SThA-MCA) were found to be insufficient.
Direct surgical clipping was performed in the majority of supraclinoid aneurysms. If this method appeared difficult or insufficiently safe intraoperatively, then the wrapping or trapping technique was a possibility. For inoperable aneurysms, by-pass was the treatment option.
One temporary by-pass and one temporary balloon occlusion occurred to be invaluable accessory techniques in the authors’ opinion, and therefore neglected. Microvascular Doppler ultrasonography was regularly used intraoperatively.
During the study years (1997–2006), there were no endovascular procedures performed in either giant or smaller ICA aneurysms. Patients were offered only a surgical treatment option.
For ruptured aneurysms, timing of the surgery was not assessed in the study. The angiogram was performed on admission and the operation took place on the next day. It referred to the majority of the ruptured ICA aneurysm, including those patients in a worse condition (Hunt-Hess grade IV). Patients in grade V were operated on if a mass effect caused of aneurismal intracerebral hemorrhage was diagnosed (Table 2).
Only significant surgery complications were analyzed, and were divided into three types: general (pneumonia, pulmonary embolism, heart attack, etc.), surgical (infectious, hematoma, CSF leakage, etc.) and neurological (conscious deterioration, ischemia in CT, etc.).
Outcome risk factors
Patient characteristics, including gender, age, education, habitation, and concomitant diseases, were analyzed to determine the relationship to outcome. Localization of aneurysm, surgical method, accessory techniques, complications, and diagnosis of new neurological deficit were analyzed for both ruptured and unruptured aneurysms. In the case of patients who presented SAH, Fisher, WFNS, and Hunt–Hess grading were taken into consideration in predicting the outcome.
Statistical methods
For categorical values, Chi-square and its nonparametric equivalents, for numerical values t and Mann–Whitney U tests were applied. Multivariate analysis was performed by logistic regression. Probability values less than 0.05 were used to determine significance.
Results
Complications
General and surgical complications occurred in 8.23% (n = 27) of cases. Surgical complications referred to 4.40% (n = 11) and general ones to 3.60% (n = 9). After surgery, new neurological deficit was diagnosed in 8.54% of cases (n = 28) (Table 3). There was an insignificantly higher percentage of patients with new deficits in giant (10.26%; n = 8) in proportion to the smaller ICA aneurysm group (8.00%; n = 20). No difference between aneurysm size groups was observed in the means of general and surgical complications.
There was no rebleeding from treated or other aneurysm observed in our series
Postoperative mortality
No perioperative death was recorded. There were 40 postoperative deaths, resulting in a total mortality rate of 12.20% in the entire group of 328 patients. No significant difference was observed in mortality between groups (12.82% in giant and 12.00% in smaller aneurysm group). Gender, age, education, habitation, segment of ICA, presence of concomitant disease, and complications did not determine postoperative mortality in whole analyzed ICA aneurysm group. Patients who died after leaving the Neurosurgery Department were lost to follow-up, as there were no such data obtained in the queries sent to the patients.
Ruptured aneurysms
There were similar mortality rates for different sizes of ruptured ICA aneurysms. Death occurred in 16.67% (n = 6) and 14.56% (n = 30) of the giant and smaller ICA aneurysms, respectively. In the giant ICA group, only GCS was the mortality determining factor, thus multivariate analysis was not performed. Uni- and multivariate analyses of significant factors related to death were shown in Table 3. Multivariate analysis revealed that Fisher grade 3 and 4 increases mortality six times and the trapping method, 13 times (Table 4).
Unuptured aneurysms
The risks of mortality for unruptured giant and small aneurysms were statistically similar, although four of 42 patients (9.52%) with giant ICA aneurysm died and all with smaller unruptured aneurysm survived (n = 44). No factors related to death in the giant and smaller unruptured ICA aneurysms were found.
Short-term outcome
The analysis of short-term outcome, based on GOS, revealed that one-third (n = 218; 33.54%) of the patients has an unfavorable outcome. Gender, education, habitation, segment of ICA, surgical method, surgical complications and presence of concomitant disease had no influence on short-term outcome in ruptured and unruptured, and both giant and smaller ICA aneurysms.
Ruptured aneurysms
No statistical difference in short-term outcome rates between the giant and the smaller ICA aneurysm group was observed. 61.11% (n = 22) of the giant and 57.77% (n = 119) of the smaller ICA aneurysm cases had a favorable outcome (four and five in GOS).
Unruptured aneurysms
In the unruptured aneurysm group, unfavorable outcome rates between giant (n = 6; 14.29%) and small aneurysms (n = 3; 6.82%) did not statistically differ (p = 0.26). Newly diagnosed neurological deficit after surgery of giant or smaller ICA aneurysms (n = 8) was related to unfavorable outcome occurrence.
Uni- and multivariate analyses of factors related to unfavorable outcome in ruptured and unruptured, giant and smaller ICA aneurysms are shown in Table 4. Multivariate analyses revealed four independent factors related to an unfavorable outcome in smaller ICA aneurysm group: patients’ age over 65, Fisher grade 4, Hunt-Hess grades 4 and 5, and newly diagnosed neurological deficit after operation. A total of 63.33% (n = 19) of patients over 65 years old, while only 38.64% (n = 68) of younger patients had an unfavorable outcome in smaller ICA aneurysms group (Table 5).
Long-term outcome
In the group of patients with an unfavorable short-term outcome (GOS grades 2 or 3), the investigators encountered problems with collecting SF-36 queries (only 35.7% of response), although the quality of life was assessed in 73.5% of patients with favorable short-term outcome. Summarily, there were 206 of 288 patients evaluated (71.5%). The mean follow-up did not differ between aneurysm size groups and was over 6 years (76.3 months), ranging from 15 to 133 months. SF-36 summary components as well as subscale scores of the giant aneurysm group did not significantly differ from the smaller aneurysm group {(Fig. 3)
A total of 41.2% of patients with giant and 45.1% of patients with smaller ICA aneurysms showed high health-related quality of life (p = 0.62). The quality of life few years after the operation of giant or smaller ICA aneurysms, was not affected by gender, education, habitation, segment of ICA, method of operation, or complications. There was a significant influence of two factors: age and the presence of concomitant disease on the quality of life in the entire ICA aneurysm group. In the separate analysis of giant and smaller aneurysms, only the presence of concomitant disease was related to low health-related quality of life in the smaller ICA aneurysm group.
Ruptured aneurysms
No difference in the SF-36 scores between the aneurysm size groups was noted, although 27.3% of the giant and 45.2% of the smaller ICA aneurysm group had low health-related quality of life. In both groups, no correlation between functional status at admission (regarding Fisher, WFNS, and Hunt-Hess grading) and SF-36 scores was observed.
Unruptured aneurysms
A few years after surgical treatment of the unruptured smaller or giant ICA aneurysms, half of the patients had low health-related quality of life, namely 54.8% and 48.3% of giant and smaller aneurysm groups, respectively. No factors related to quality of life were found.
Discussion
The above study was based on a single-center and a single-surgeon series of surgically treated (both ruptured and unruptured) saccular ICA aneurysms. After excluding multiple and blood blister-like aneurysms, the analyzed group consisted of 23.78% giant aneurysms, a higher percentage than published [1, 11, 28]. This was due to the fact that some patients with diagnosed GIAs were admitted from other neurosurgical wards that do not have much experience in surgical treatment of GIAs. Since most of the smaller aneurysms were diagnosed after their rupture, giant causing mass effect or asymptomatically, thus separate comparisons of ruptured and unruptured ICA aneurysms were carried out.
Complications
An insignificantly higher percentage of newly diagnosed neurological deficits after operation was found in giant ICA aneurysm patients. The surgery of GIAs is supposed to be a more difficult and complicated entity than smaller aneurysms [28]. A thorough analysis of general and surgical complications was not the purpose of this study. Le Roux indicates that the complication rate can reach even up to 100%, depending on established criteria [17].
There was no rebleeding observed in the entire analyzed group. The risk of rupture from a secured aneurysm is low. In the ISAT study [22], 0.10% neurosurgically treated patients experienced rebleeding from the target aneurysm in 4 years of follow-up. On the other hand, in our series, rebleeding might not occur due to losing patients during the follow-up.
Postoperative mortality
Surgical mortality rates for GIAs may vary from 4 to 21%, with an average of 10% [27]. In the presented series of ICA aneurysms, similar death rates for giant and smaller were obtained, resulting in a 12% overall mortality rate. A considerable number of 328 patients enabled the analysis of multivariate factors which influence mortality, indicating that not aneurysm size, but the amount of blood (Fisher grade) and the trapping method were increasing the number of deaths. Kassell’s [9, 10] publications, based on large series, signified that aneurysm size is one of the death prognostic factors. He also indicated that level of consciousness and age was related to higher mortality rate, which our study did not confirm in the ruptured ICA aneurysm population. Consecutive improving of surgical techniques contributed to a significant decrease in the mortality and that was also confirmed by the authors in the present study.
Short-term outcome
In author’s opinion [9, 10], short-term outcome after surgical treatment of ruptured giant aneurysms is worse than smaller ones. Although the presented series partially confirmed the above opinion, it is worth mentioning that the difference was not significant. In giant unruptured aneurysms, the percentage of favorable short-term outcome was similar to smaller aneurysms. The surgical treatment of unruptured smaller ICA aneurysms revealed that up to 7% of patients may have an unfavorable short-term outcome, but natural history and consequences [29] of rupture excuse intervention. The analysis of factors influencing short-term outcome in the smaller aneurysm group confirmed well-known [8] unfavorable prognostic factors: Fisher grade 4, Hunt-Hess grades 4 and 5 and patients’ higher age. It also acknowledges current status, indicating the amount of blood as the strongest prognostic factor [8–10]. Newly diagnosed neurological deficit after the operation of both ruptured and unruptured smaller ICA aneurysms was connected to unfavorable outcomes. In giant aneurysms, conventional endovascular therapy or use of dimethyl sulfoxide (Onyx) is related to 8% morbidity [21].
Long-term outcome
In the authors’ opinion, the use of the SF-36 questionnaire in patients with unfavorable outcome on discharge (GOS grade 2 or 3) a few years after surgery is debatable. However, response rate can attain 100% in a similar group [26]. There are no published reports comparing quality of life between giant and smaller ICA aneurysms. The presented study revealed that the long-term outcome of different aneurysm size groups is similar. Moreover, in opposition to Scharbrodt’s publication [26], the quality of life does not depend on functional status at admission in the ruptured aneurysm group. Higher age and presence of concomitant disease were the only two factors related to low health-related quality of life a few years after the operation of giant or smaller ICA aneurysms. Despite the fact that age may influence the brain’s ability to recover [26], other factors (social, economic) determine age-related quality of life [7]. As a matter of fact, concomitant diseases may affect health-related quality of life, which has been acknowledged in the presented series.
In conclusion, the analysis of the surgically treated 78 giant and 250 smaller ICA suggests that mortality, morbidity, and short and long-term outcomes of these patients are similar. These novel results are at variance with some standard neurosurgical reports from highly experienced neurovascular surgeons worldwide [1, 15, 16, 25]. Most papers considering the outcomes of surgically treated giant ICA aneurysms are dated to the late 1980s and 1990s of the previous century [1, 9, 15–17, 23, 25, 28] and they rarely exceeded 80% of good results. A few successors, taught by the formers’ experience, showed that surgical treatment still remains a gold standard, publishing that outcome could be better. They achieved up to 90% good results [4, 27, 30]. Proper, individualized case selection and surgical strategy including accessory techniques, preoperative assessment of vascular anastomoses, temporary parent vessel occlusion, retrograde suction decompression, and microvascular Doppler ultrasonography can substantially improve microsurgical outcome [27, 30]. Therefore, we believe that our innovative conclusions could encourage other scientists to share their results and would open the discussion on this particularly interesting topic.
The unique peculiarity of giant ICA aneurysms requires extensive comprehension of the treatment strategies to achieve better results. An experienced neurovascular surgeon should be accustomed to all surgical techniques for giant ICA aneurysms [23].
References
Barrow DL, Alleyne C (1995) Natural history of giant intracranial aneurysms and indications for intervention. Clin Neurosurg 42:214–244
Barth A, de Tribolet N, Barth A, de Tribolet N (1994) Growth of small saccular aneurysms to giant aneurysms: presentation of three cases. Surg Neurol 41:277–280
Dolenc V (1999) Extradural approach to intracavernous ICA aneurysms. Acta Neurochir Suppl 72:89–106
Doormaal TP, Zwan A, Verweij BH, Langer DJ, Tulleken CA (2006) Treatment of giant and large internal carotid artery aneurysms with a high-flow replacement bypass using the excimer laser-assisted nonocclusive anastomosis technique. Neurosurgery 59 (4 Supl 2):328–334; discussion 334–335
Flamm ES (1997) Cerebral aneurysms and subarachnoid hemorrhage history of neurovascular surgery. In: Greenblatt S (ed) History of neurological surgery. AANS Publishers, Park Ridge
Janse AJ, Gemke RJ, Uiterwaal CS, van der Tweel I, Kimpen JL, Sinnema G (2004) Quality of life: patients and doctors don't always agree: a meta-analysis. J Clin Epidemiol 57:653–661
Jokela M, Singh-Manoux A, Ferrie JE, Gimeno D, Akbaraly TN, Shipley MJ, Head J, Elovainio M, Marmot MG, Kivimaki M (2010) The association of cognitive performance with mental health and physical functioning strengthens with age: the Whitehall II cohort study. Psychol Med 40(5):837–845
Juvela S, Siironen J, Varis J, Poussa K, Porras M (2005) Risk factors for ischemic lesions following aneurysmal subarachnoid hemorrhage. J Neurosurg 102(2):194–201
Kassell NF, Torner JC, Haley EC Jr, Jane JA, Adams HP, Kongable GL (1990) The International Cooperative Study on the Timing of Aneurysm Surgery. Part 1. Overall management results. J Neurosurg 73(1):18–36
Kassell NF, Torner JC, Jane JA, Haley EC Jr, Adams HP (1990) The International Cooperative Study on the Timing of Aneurysm Surgery. Part 2. Surgical results. J Neurosurg 73(1):37–47
Khurana VG, Piepgras DG, Whisnant JP (1998) Ruptured giant intracranial aneurysms: Part I - A study of rebleeding. J Neurosurg 88:425–429
Kim DH, Haney CL, Van Ginhoven G (2005) Utility of outcome measures after treatment for intracranial aneurysms: a prospective trial involving 520 patients. Stroke 36(4):792–6
Kodama N, Suzuki J (1982) Surgical treatment of giant aneurysms. Neurosurg Rev 5:155–160
Krings T, Piske RL, Lasjaunias PL (2005) Intracranial arterial aneurysm vasculopathies: targeting the outer vessel wall. Neuroradiology 47:931–937
Lawton MT, Spetzler RF (1995) Surgical management of giant intracranial aneurysms: experience with 171 patients. Clin Neurosurg 42:245–266
Lemole GM, Henn J, Spetzler RF, Riina HA (2000) Surgical management of giant aneurysms. Oper Tech Neurosurg 3(4):239–254
Le Roux PD (2004) Management of cerebral aneurysms. Saunders, Pennsylvania
Locksley HB (1966) Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations: based on 6368 cases in the cooperative study. J Neurosurg 25:219–239
Lokato EB, Gravenstein N, Kirby RR (2007) Complications in anesthesiology, ed.3. Wolters Kluwer Health. Lippincott Williams & Wilkins, p 4
Michel WF (1974) Posterior fossa aneurysms simulating tumours. J Neurol Neurosurg Psychiatry 37:218–223
Molyneux AJ, Cekirge S, Saatci I, Gal G (2004) Cerebral Aneurysm Multicenter European Onyx (CAMEO) trial: results of a prospective observational study in 20 European centers. AJNR Am J Neuroradiol 25:39–51
Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, Sandercock P (2005) International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 366(9488):809–17
Parkinson RJ, Eddleman CS, Batjer HH, Bendok BR (2006) Giant intracranial aneurysms: endovascular challenges. Neurosurgery 59(5 Suppl. 3):103–12; discussion 3–13
Pavlisa G, Ozretic D, Murselovic T, Pavlisa G, Rados M (2010) Sole stenting of large and giant intracranial aneurysms with self-expanding intracranial stents-limits and complications. Acta Neurochir (Wien) 152(5):763–9
Peerless SJ, Wallace MC, Drake CG (1990) Giant intracranial aneurysms. In: Youmans JR (ed) Neurological surgery: a comprehensive reference guide to the diagnosis and management of neurological problems. WB Saunders, Philadelphia, pp 1742–63
Scharbrodt W, Stein M, Schreiber V, Böker DK, Oertel MF (2009) The prediction of long-term outcome after subarachnoid hemorrhage as measured by the Short Form-36 Health Survey. J Clin Neurosci 16(11):1409–13
Sharma BS, Gupta A, Ahmad FU, Suri A, Mehta VS (2008) Surgical management of giant intracranial aneurysms. Clin Neurol Neurosurg 110(7):674–81
Wehman JC, Hanel RA, Levy EI, Hopkins LN (2006) Giant intracranial aneurysms: endovascular challenges. Neurosurgery 59(5 Suppl 3):125–138
Wiebers DO, Whisnant JP, Huston J, Meissner I, Brown RD Jr, Piepgras DG (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risk for surgical and endovascular treatment. (ISUIA). The Lancet 12:362,9378:103.
Xu BN, Sun ZH, Romani R, Jiang JL, Wu C, Zhou DB, Yu XG, Hernesniemi J, Li BM (2010) Microsurgical management of large and giant paraclinoid aneurysms. World Neurosurg 73(3):137–146
Acknowledgements
I thank my advisor and teacher Professor M.D. Pawel Sloniewski, the Head of Neurosurgery Department of Medical University of Gdansk in Poland, for his continuous support in the PhD program and great help in preparing this paper.
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
Somewhat surprisingly, this single-center series of 78 patients with giant and 250 with smaller ICA aneurysms operated on by a single surgeon had similar outcomes after surgery. However, the series was rather selective with a very short and incomplete follow-up. Even if there are some biases in the series, it still shows that microsurgical techniques are developing constantly, and in experienced hands, aneurysms can be safely operated on. This addresses the importance of patients being treated in dedicated neurovascular centers not forgetting the collaboration between microsurgical and endovascular surgeons.
Mika Niemelä
Hanna Lehto
Juha Hernesniemi
Helsinki, Finland
This study was approved by the Ethical Comity of the Medical University of Gdansk (No: NKEBN/209/2008).
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Szmuda, T., Sloniewski, P. Early and long-term outcome of surgically treated giant internal carotid artery aneurysms—comparison with smaller aneurysms. Acta Neurochir 153, 1611–1619 (2011). https://doi.org/10.1007/s00701-011-1021-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1021-6