Abstract
Purpose
Vertebral column resection (VCR) is a technique performed for short, angular spinal deformities. Several studies have reported good radiographic results with VCR regarding curve correction. However, only a few studies have reported the impact of this technique on the health-related quality-of-life measures (HRQoL).
Methods
A single surgeon series of 27 consecutive children (mean age at surgery 12.3 years, range 1.1–20.7 years) undergoing posterior VCR with a minimum of 2-year follow-up. The comparison was made to age- and gender-matched healthy controls. Outcome measures included Scoliosis Research Society (SRS) questionnaire both pre- and postoperatively, radiographic outcomes, and complications.
Results
The average major curve correction was 60.3% in the VCR patients. Complications were noted in 12 out of 27 (44%) of the VCR patients but all patients recovered fully during follow-up. The SRS pain domain scores improved significantly after VCR (p = 0.0002). The SRS total and domain scores were significantly lower than in the healthy controls especially in the self-image and function domains, but the pain and activity domains improved from preoperative to similar level than in the control group.
Conclusions
HRQoL showed significant improvement in pain scores despite 44% risk of transient complications after VCR in pediatric patients. This health-related quality-of-life improvement remained at a significantly lower level than in the healthy control group.
Level of Evidence
Therapeutic Level III.
Similar content being viewed by others
Introduction
Vertebral column resection (VCR) is defined as a resection of the dorsal components and at least one vertebral body with the caudal and cranial intervertebral disks. Typical indications in the pediatric age group include short angular and/or severe spinal deformities [1, 2]. An untreated severe scoliosis sometimes needs apical VCR to allow adequate correction [1, 3]. VCR was originally performed using an anteroposterior approach [4], but more recently it has been performed using a posterior only approach (PVCR) [1, 5, 6].
Several studies have reported good radiographic results, but the risk of spinal cord and/or neural element deficits appears to be higher than in typical pedicle screw instrumentation [1, 3, 5,6,7]. Lenke et al. published the first series of PVCR to pediatric patients and reported no spinal cord-related complications [1]. Curve correction of approximately 60% can be achieved with PVCR [3, 8].
To the best of our knowledge, data on the health-related quality of life (HRQoL) after PVCR in pediatric patients are limited [3, 8] and no comparisons of HRQoL at the end of follow-up to healthy controls have been published. In the series of Helenius et al., most patients reported high satisfaction in Scoliosis Research Society (SRS)-24 scores [3]. One long-term study reporting HRQoL measures in a combined series of pediatric and adult patients exists [8].
We aimed to compare HRQoL in pediatric patients with congenital or idiopathic scoliosis undergoing PVCR with healthy controls. We hypothesized that PVCR would improve HRQoL, but the quality of life would still remain at lower level than in healthy controls.
Methods
This was a retrospective study using a prospectively collected data on consecutive children undergoing PVCR by a single orthopedic spine surgeon. All consecutive PVCR procedures from January 2007 to January 2018 were evaluated for eligibility. Exclusion criteria included associated neurological or syndromic condition preventing assessment of HRQoL. Results were compared with age and sex matched healthy controls. Age matching was performed based on the age at final follow-up.
Twenty-seven otherwise healthy children (mean age 12.3 years, range 1.1 to 20.5) with minimum 2 years follow-up underwent PVCR for short angular congenital scoliosis or kyphosis or severe scoliosis (from January 2007 to January 2018 (mean follow-up 4.0 years, range 2 to 11 years). The indications included congenital kyphosis (n = 7), congenital scoliosis (n = 6), congenital kyphoscoliosis (n = 8), global kyphosis (n = 2), metatropic dysplasia and thoracic kyphosis (n = 1) and congenital dislocation of vertebral column (n = 1). This cohort did not include single posterolateral hemivertebra resections. The study received approval from the Ethics Committee of the Hospital District (Tables 1 and 2).
Perioperative data were recorded, as well as radiographic outcomes (Table 3) and SRS-24 scores preoperatively and at follow-up visits. HRQoL questionnaires were filled by the patient or parents depending on the age of the patient. Typically, children below 10 years of age were assisted by their parents/caregivers to fill out the questionnaires. Patients were examined before and after surgery for their lower limb neurological function, walking ability, sitting, and standing balance. Preoperatively full spinal magnetic resonance imaging (MRI) and CT were taken in all patients. Children with congenital deformities underwent preoperative renal and cardiac ultrasound.
Surgical technique
PVCR was performed as described by Lenke et al. [1]. The posterior elements of the spine and one-third of the posterior part of the rib at the area of VCR were exposed. The pedicle screws were inserted [9]. Multiaxial reduction screws were used at the apical concave side and just below the resection level and radiographs were obtained to confirm their position (CD Legacy or Solera 5.5/6.0, Medtronic Spinal and Biologics, Memphis, Tennessee, USA). 5 cm of the medial rib head on both sides was resected and an extra pleural plane around the thoracic spine was created, with preservation of the segmental vessels and nerve roots (Pedicle Subtraction Osteotomy (PSO) Tool Set; Medtronic Spinal and Biologics, Memphis, Tennessee). The vertebral body and the disk above and below were identified and then resected up to the concave side. The resection was completed with removal of the concave-side pedicle. The posterior vertebral body wall was removed (a posterior vertebral wall impactor (PSO Tool Set)). Epidural bleeding was controlled by bipolar cauterization and human thrombin with gelatin matrix (FloSeal; Baxter US, Deerfield, Illinois). Final correction was obtained with exchange of the final long rod along with in situ bending in the coronal, and in the sagittal plane.
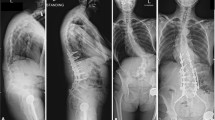
If spinal cord monitoring demonstrated normal motor evoked potential (MEP) and sensory evoked potential (SEP) with shortening of the spinal column and the remaining defect after correction between endplates was < 5 mm, no cage was inserted and the gap was filled with cancellous bone chips (Fig. 1) A cage was used in cases where the defect after deformity correction remained more than 5 mm to expedite spinal fusion (Fig. 2) [5]. Five (18.5%) patients required a cage. Local bone graft taken from the wedge resection and the ribs was applied circumferentially.
Perioperative management
Spinal cord monitoring was performed. Postoperatively patients were monitored in the pediatric intensive care unit and mean arterial pressure was maintained between 65 and 75 mmHg (24 h). All patients received intravenous prophylactic cefuroxime and vancomycin 30 min before incision; cefuroxime was continued for 72 h postoperatively. Thirteen patients (48.1%) were immobilized using a rigid thoracolumbosacral orthosis (TLSO) for 4 months.
Radiographic parameters
The proximal thoracic, main thoracic, and thoracolumbar/lumbar curves were measured from anteroposterior radiographs and thoracic kyphosis (T5–T12), lumbar lordosis (T12–S1), and segmental kyphosis or lordosis were measured from the lateral radiographs using the Cobb technique [10, 11].
SRS-24 questionnaire
SRS-24 -questionnaire [12] was filled out by the VCR patients preoperatively and at follow-up visits. The questionnaire has 7 domains: pain, general self-image, function from back condition, general level of activity, postoperative self-image, postoperative function, and satisfaction. A score < 4 in the SRS-24 pain domain (1 = severe pain and 5 = pain free) is considered clinically relevant [13].
Healthy controls
Rather than the SRS-24, the healthy control groups filled out the SRS-22r, which is an improved and modified version of the original SRS-24 [12, 14]. Data for healthy control subjects were obtained from our previous study [15]. Two-hundred and seventy-two healthy controls were selected from a population register and were invited to complete and return the SRS-22r questionnaire [12, 14] between January 2012 and December 2015 [15]. Two healthy controls were matched for sex and age at final follow-up for each PVCR patient.
To compare PVCR patients with controls, we used the first 15 questions of the preoperative SRS-24 outcomes. Questions 1 through 15 of the SRS-24 correspond with questions 1, 2, 4, 5, 6, 8, 9, 11, 12, 14, 15, and 17 through 20 of the SRS-22r. These questions were used as the basis for 4 domains of comparison between preoperative SRS-24 scores for the PVCR treatment group and the healthy control groups: pain (SRS-24: 1, 2, 3, 6, 8, and 11; SRS-22r: 1, 2, 4, 8, 11, and 14), general self-image (SRS-24: 5, 14, and 15; SRS-22r: 6, 19, and 20), general function (SRS-24: 7, 12, and 13; SRS-22r: 9, 15, and 18), and general activity (SRS-24: 4, 9, and 10; SRS-22r: 5, 12, and 17) [12].
Statistical analysis
Mean changes between baseline and 2 years were compared between the groups with linear mixed models for repeated measurements. Model included time as within factor and group as between factor, and also group x time interaction was included in the model. Assumptions were checked with studentized residuals. Results for VCR operated patients at 2 years after operation and control subjects were compared with Wilcoxon rank sum test. p values less than 0.05 (two-sided) were considered as statistically significant. The data analysis was generated using SAS software, Version 9.4 of the SAS System for Windows (SAS Institute Inc., Cary, NC, USA).
Results
Twenty-seven patients underwent posterior vertebral column resection (Table 1). PVCR was performed as a primary surgery in 25 (92.6%) and as a revision surgery in two (7.4%) patients. Preoperative halo-gravity traction was used in two children (7.4%) (3 months). The mean intraoperative blood loss was 1015 ml (range 120–3500 ml) and operative time 4.7 h (range 3.1–6.5 h) (Table 2).
The mean coronal curve correction was 62.9% (range, 0–100%) and the mean lateral curve correction was 53.6% (range, 5.6–100%) at final follow-up.
Complications
Complications were noticed in 12/27 patients (44%) in the VCR cohort. These included four cerebrospinal fluid leakages requiring suture of the leak and three pleural lesions requiring a chest drain. One patient developed pneumonia. One superficial wound infection was noticed. One patient had skin erosion over proximal thoracic pedicle screws (2 years after the PVCR) and needed revision surgery (unilateral removal of prominent screws and wound revision). One patient presented with one-sided lower instrumentation partial pedicle screw pull-out. The patient was asymptomatic and during the 2-year radiographic follow-up remained stable suggesting spinal union. Two patients developed junctional kyphosis and one of them needed revision and extension of instrumentation. Intraoperative neurological events (transient losses of intraoperative neurophysiologic monitoring) were observed in ten cases (37.0%), but these resolved in eight patients with additional circumferential decompression of the spinal cord and with reducing deformity correction intraoperatively. Postoperative neurological deficits were encountered in two patients (2/27, 7.4%). One patient had L5 nerve root deficit (ankle dorsiflexion) postoperatively, which resolved within 10 days. Another was iatrogenic medullar contusion and right-sided paraplegia postoperatively. This neural deficit resolved fully in 6 months (Table 3).
Health-related quality of life
In VCR group pain, self-image, and general activity improved during the 2-year follow-up, but the pain score was the only with statistically significant change (p = 0.0002). Compared to healthy controls, the VCR group had significantly lower total, self-image, and function scores (p < 0.05), but similar pain and activity scores at final follow-up (Table 5).
Preoperatively as well as at 2-year follow-up, one VCR patient reported moderate to severe pain during the last 6 months with use of question #1 in SRS questionnaire. However, five patients scored < 4 in the preoperative SRS-24 pain domain. The number of patients scoring < 4 was two at 2 years follow-up (p = 0.195).
Patients with surgical complications had similar SRS-24 total score as well SRS-24 domains at final follow-up. Age at surgery, type of deformity (scoliosis vs. kyphosis), number of fusion levels, primary vs. revision surgery did not affect SRS-24 total scores or majority of domain scores. However, self-image domain scores were better in younger age group (p = 0.04) and in scoliosis group (p = 0.04) preoperatively and postoperatively in younger age group (p = 0.02).
Comparison with healthy controls
The mean pain domain scores and scores in general activity did not differ between the VCR patients and the healthy controls. The SRS pain domain score averaged 4.66 (2.33–5.00) in VCR group and 4.72 (2.83–5.00) in healthy control group (p = 0.65). The mean scores in function and self-image domains were significantly better in the healthy control group as compared with the VCR group (p < 0.05) (Table 4).
Discussion
Posterior vertebral column resection provided satisfactory correction of angular and/or severe pediatric spine deformities. Children with PVCR showed improvement in HRQoL but remained at significantly lower level than age- and gender-matched healthy controls at 2-year follow-up. The overall risk of complications, 44%, is significant and although transient in all patients this information should be given to families.
Strengths and limitations
The strength of this study is that VCR procedures were performed by a single surgeon using standardized technique and prospective data collection. The control group allowed comparison with healthy controls. HRQOL assessment was possible as only patients with normal intelligence were included. However, the study is limited by small sample size and retrospective design.
One limitation of this study was the somewhat different questionnaires used (the SRS-24 and SRS-22r); however, we chose to keep the same original SRS-24 questionnaire in the surgical treatment group to provide data from preoperatively to final follow-up postoperatively. To provide comparable questionnaires, we used the 15 most similar preoperative questions from the SRS-24 and SRS-22r, including 8 questions that were exactly the same, to form the pain, activity, self-image, and function domains. For the 7 questions that were not an exact match, the scoring was not identical, but close enough to make a valid comparison.
Comparison with previous data
In our series, over 50% curve correction rate was achieved with 44% complication rate. Intraoperative neurological events were monitored in 37%, and in two patients also postoperatively, but during follow-up, these resolved fully. Suk et al. were the first to report results using PVCR in adult patients [5, 6]. In their series, complications occurred in 24/70 (34%) and 4/16 (25%) patients, including three (3/86, 3.5%) complete spinal cord injuries which were not transient. Lenke et al. reported PVCR for 35 consecutive pediatric spinal deformities, with no spinal cord-related complications and with 60% correction of the scoliosis [1]. Spiro et al. evaluated 10 children undergoing PVCR for congenital kyphosis with two patients requiring revision surgery for junctional kyphosis and with two intraoperative neuromonitoring changes without postoperative neural deficits [2]. In a multicenter cohort of 147 pediatric patients undergoing PVCR, Lenke et al. reported a 59% complication rate, as well as a 27% rate of intraoperative neurological events [16], none of the patients had permanent paraplegia. Hence, our results on curve correction and complication rate were comparable with previous reports.
Studies evaluating the HRQoL in VCR patients are sparse. Recently, Riley et al. evaluated HRQoL in a group of 54 patients (31 children) after minimum 5-year follow-up [8]. Of the 54 patients, 30 (55.6%) sustained complications and seven (13.0%) required a revision. Intraoperative neurological events occurred in 12.9% (16.1% pediatric), and 12.9% of pediatric patients had postoperative neurological deficits. Despite the high risk of complications, significant improvements were observed in pediatric group in the SRS self-image (0.9 points) and in the SRS satisfaction (1.8) at 5-year follow-up. They suggested that patients appreciate HRQoL improvement after the surgical procedure, despite high complication rates. Our findings showed significant improvement in the SRS-24 pain domain after PVCR. The minimal clinically important difference for SRS-22r pain domain scores in adolescents has been reported at 0.20 [17]. Data regarding the minimal clinically important values for the SRS-24 are lacking. In the present study, the mean pain domain score improved by 0.72 (95% CI, 0.38 to 1.06) in the PVCR patients. There was a relatively large standard deviation in the SRS-24 scores of the VCR group resulting into smaller statistical power to detect statistical difference between the study groups. At the end of follow-up, the SRS total score, self-image, function domains were at a lower level in the VCR group than in the healthy controls, but the pain and activity domains improved from preoperative to similar level than in the control group. Despite improvement in the radiographic parameters, the children undergoing PVCR had a significantly lower self-image score than the healthy controls.
The pediatric patients undergoing VCR for severe and angular spinal deformities rarely present with existing myelopathy and the indication to osteotomy is to prevent myelopathy and spinal cord dysfunction [18, 19]. Even if the patient receives a major improvement in the spinal deformity, it may not be quite clear to the families that without apical VCR there would remain a relatively high risk of future deterioration in the spinal cord. It remains unclear if the families understand the risks of this procedure and even though all complications in the current series were transient this information is important to be delivered into the decision-making process. The length of instrumentation and spinal fusion required to prevent further adding on or junctional issues are relatively long resulting into lower score of the SRS function domain.
Conclusion
Health-related quality of life showed significant improvement in pain scores despite 44% risk of transient complications after PVCR. This HRQoL improvement remained at a significantly lower level than matched healthy control group.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
SAS software, Version 9.4 of the SAS System for Windows (SAS Institute Inc., Cary, NC, USA).
References
Lenke LG, O’Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM (2009) Posterior vertebral column resection for severe pediatric deformity: minimum two-year follow-up of thirty-five consecutive patients. Spine 34:2213–2221. https://doi.org/10.1097/BRS.0b013e3181b53cba (Phila Pa 1976)
Spiro AS, Rupprecht M, Stenger P, Hoffman M, Kunkel P, Kolb JP, Rueger JM, Stuecker R (2013) Surgical treatment of severe congenital thoracolumbar kyphosis through a single posterior approach. Bone Jt J 95:1527–1532. https://doi.org/10.1302/0301-620X.95B11.31376
Helenius I, Serlo J, Pajulo O (2012) The incidence and outcomes of vertebral column resection in paediatric patients: a population-based, multicentre, follow-up study. J Bone Jt Surg Br 94:950–955. https://doi.org/10.1302/0301-620X.94B7.28545
Leatherman KD, Dickson RA (1979) Two-stage corrective surgery for congenital deformities of the spine. J Bone Jt Surg Br 61:324–328
Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK (2005) Posterior vertebral column resection for severe rigid scoliosis. Spine 30:1682–1687. https://doi.org/10.1097/01.brs.0000170590.21071.c1 (Phila Pa 1976)
Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH (2002) Posterior vertebral column resection for severe spinal deformities. Spine 27:2374–2382. https://doi.org/10.1097/00007632-200211010-00012 (Phila Pa 1976)
Lenke LG, Sides BA, Koester LA, Hensley M, Blanke KM (2010) Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res 468:687–699. https://doi.org/10.1007/s11999-009-1037-x
Riley MS, Lenke LG, Chapman TM Jr, Sides BA, Blanke KM, Kelly MP (2018) Clinical and radiographic outcomes after posterior vertebral column resection for severe spinal deformity with five-year follow-up. J Bone Jt Surg Am 100:396–405. https://doi.org/10.2106/JBJS.17.00597
Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 29:333–342. https://doi.org/10.1097/01.brs.0000109983.12113.9b (Phila Pa 1976)
Cobb JR (1948) Outline for the study of scoliosis. AAOS Instr Course Lect 5:261–275
O’Brien MF, Kuklo TR, Blanke KM, Lenke LG (2004) Radiographic measurement manual. Medtronic Sofamor Danek Inc, Memphis
Haher TR, Gorup JM, Shin TM, Homel P, Merola AA, Grogan DP, Pugh L, Lowe TG, Murray M (1999) Results of the scoliosis research society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine 24:1435–1440. https://doi.org/10.1097/00007632-199907150-00008 (Phila Pa 1976)
Djurasovic M, Glassman SD, Sucato DJ, Lenke LG, Crawford CH 3rd, Carreon LY (2018) Improvement in scoliosis research society-22r pain scores after surgery for adolescent idiopathic scoliosis. Spine 43:127–132. https://doi.org/10.1097/BRS.0000000000001978 (Phila Pa 1976)
Asher M, Min Lai S, Burton D, Manna B (2003) The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine 28:63–69. https://doi.org/10.1097/00007632-200301010-00015 (Phila Pa 1976)
Diarbakerli E, Grauers A, Gerdhem P (2017) Population-based normative data for the scoliosis research society 22r questionnaire in adolescents and adults, including a comparison with EQ-5D. Eur Spine J 26:1631–1637. https://doi.org/10.1007/s00586-016-4854-0
Lenke LG, Newton PO, Sucato DJ, Shufflebarger HL, Emans JB, Sponseller PD, Shah SA, Sides BA, Blanke KM (2013) Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine 38:119–132. https://doi.org/10.1097/BRS.0b013e318269fab1 (Phila Pa 1976)
Carreon LY, Sanders JO, Diab M, Sucato DJ, Sturm PF, Glassman SD, Grp SDS (2010) The minimum clinically important difference in scoliosis research society-22 appearance, activity, and pain domains after surgical correction of adolescent idiopathic scoliosis. Spine 35:2079–2083. https://doi.org/10.1097/BRS.0b013e3181c61fd7 (Phila Pa 1976)
Marks DS, Qaimkhani SA (2009) The natural history of congenital scoliosis and kyphosis. Spine 34:1751–1755. https://doi.org/10.1097/BRS.0b013e3181af1caf (Phila Pa 1976)
Winter RB, Moe JH, Wang JF (1973) Congenital kyphosis. Its natural history and treatment as observed in a study of one hundred and thirty patients. J Bone Joint Surg Am 55:223–256
Funding
Open access funding provided by University of Turku (UTU) including Turku University Central Hospital. The sampling of control data was financially supported by funds from Karolinska Institutet, the Swedish Research Council grant numbers 2012-02275 and 2017-01639, and by grants provided by Region Stockholm (ALF project).
Author information
Authors and Affiliations
Contributions
JS, LH, and IH designed the study. JS, PG, and ED acquired data. JS, LH, AR, and IH analyzed and interpreted the data. JS and IH wrote the original manuscript and all authors actively involved in the drafting and critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Paul Gerdhem was supported by Region Stockholm (clinical research appointment) and CIMED. Arimatias Raitio has received research grants from Emil Aaltonen Foundation, Turku University Foundation and Clinical Research Institute HUCH. Johanna Syvänen has received research grants from Clinical Research Institute HUCH. Ilkka Helenius received scientific funding from industry (Medtronic, Stryker Spine) outside the submitted manuscript. The funding source did not play any role in the investigation. Other authors have no conflicts of interest to declare that are relevant to the content of this article.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors have seen the final version of the manuscript and approved the submission.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Syvänen, J., Helenius, L., Raitio, A. et al. Health-related quality of life after posterior vertebral column resection in children: comparison with healthy controls. Eur J Orthop Surg Traumatol 32, 899–907 (2022). https://doi.org/10.1007/s00590-021-03064-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03064-3