Abstract
Purpose
Free-hand pedicle screw insertion methods are widely used for screw insertion during scoliosis surgery. Preoperative knowledge about the pedicle size helps to maximize screw containment and minimize the risk of pedicle breach. Radiographs taken by a biplanar low-dose X-ray device (EOS) have no divergence in the vertical plane. The criterion validity and reliability of preoperative EOS images for pedicle size measurements in patients with idiopathic scoliosis (IS) was investigated in this study.
Methods
Sixteen patients who underwent surgical treatment for IS were prospectively included. Intra- and extracortical pedicle height and width measurements on EOS images were compared with reconstructed intra-operative 3D images of the isthmus of included pedicles. Secondly, intra- and interobserver reliability of pedicle size measurements on EOS images was determined.
Results
The total number of analyzed pedicles was 203. The correlation between the EOS and 3D scan measurements was very strong for the intra- and extracortical pedicle height and strong for the intra- and extracortical pedicle width. There are, however, significant, but likely clinically irrelevant differences (mean absolute differences < 0.43 mm) between the two measure methods for all four measurements except for extracortical pedicle height. For pedicles classified as Nash–Moe 0, no significant differences in intra- and extracortical pedicle width were observed. Both intra- and interobserver reliability was excellent for all pedicle size measurements on EOS images.
Conclusion
The results of this study indicate a good validity and reliability for pedicle size measurements on EOS radiographs. Therefore, EOS radiographs may be used for a preoperative estimation of pedicle size and subsequent screw diameter in patients with IS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Posterior spinal instrumentation and fusion with pedicle screws is a standard practice in the surgical treatment of severe idiopathic scoliosis (IS) [1,2,3]. It is regarded as a safe and effective procedure in the majority of the patients [4]. However, appropriate placement of well-sized pedicle screws can be challenging in scoliosis due to the different morphometric characteristics of the pedicle dimensions and vertebral rotation [2]. As shown in earlier CT studies, there is a wide variation in pedicle shapes and sizes in a scoliotic spine [5]. Consequently, screw misplacements and under- or oversizing are risks. This subsequently increases the risk of neurologic or vascular injury, pedicle fracture, and screw loosening [6, 7].
Free-hand pedicle screw insertion methods are widely used for screw insertion. Due to the variation in pedicle dimensions, it is not possible to use standardized screw diameters for each spinal levels. Previous studies showed that full containment of the screws within the cortical pedicle walls was achieved 69–94% with free-hand placement, and pedicle breach rates are reported at 9.7%–17.1% [6, 7]. Preoperative knowledge about the pedicle size helps to maximize screw containment and minimize the risk of pedicle breach. To accurately measure the pedicle sizes, a preoperative computed tomography (CT) scan is needed [8]. However, this is not done routinely in clinical practice due to the exposure of this young population to high levels of radiation. Plane radiographs as alternative have the disadvantage that there is divergence in both the horizontal and vertical planes.
The EOS imaging system can provide biplanar low-dose radiographs of the spine, which reduces the amount of radiation substantially in comparison with CT and conventional radiographs [9, 10]. Furthermore, images have no divergence in the vertical plane since the system uses a C-arm. Despite these advantages, the reliability of the EOS imaging system for pedicle size measurements has not been investigated.
The purpose of this study was to assess the validity and intra- and interobserver reliability of preoperative EOS images for measurements of the pedicle heights and widths in patients with IS.
Methods
Patients
This study was approved by the Medical Ethical Review Board (RR-Number: 201800917) and carried out in the University Medical Center Groningen (UMCG). After obtaining informed consent, patients were prospectively included from October 2018 to April 2019. Inclusion criteria were: (1) IS patients aged between 12 and 25 years with (2) a Cobb angle of the thoracic and/or lumbar curve of 50 degrees or more (3) undergoing surgical correction. Patients with spinal anomalies or previous spine operations were excluded.
Medical imaging
Routine biplanar low-dose radiographs of the spine were made preoperatively with the EOS system (EOS imaging, Paris, France). Patients were positioned on the EOS platform in standing position. Surgical treatment was performed using routine intra-operative 3D imaging (Siemens Arcadis Orbic 3D C-arm) and navigation system (Stryker). These intra-operative 3D images were used as “gold standard” in this study.
Method of measurements
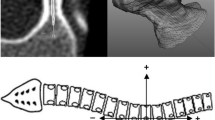
Two independent observers (CP and LH), residents from the department of orthopedic surgery and radiology, analyzed the pedicle sizes in the preoperative EOS images and intra-operative 3D images. Both observers were blinded for the scoring of the other observer. One observer (CP) performed all measurements twice with a week between the measurements. The pedicle sizes were measured with Advanced PACS Viewer. The standing AP view was used for measurements on the EOS images. For the intra-operative 3D scan, the vertical plane perpendicular on the lines of the transverse and sagittal pedicle angle was reconstructed at the narrowest part (isthmus) of each individual pedicle (Fig. 1). The analysis of each pedicle consisted of the largest intracortical and extracortical diameter of the height and width of the pedicle isthmus (Figs. 1, 2). The Nash and Moe method was used on the EOS AP view to determine the vertebral rotation [11]. Pedicles on the concave side with a Nash–Moe rotation score ≥ 2 were not measurable and therefore excluded from analysis.
Statistical analyses
Paired-sample T-tests were used to compare differences in the mean pedicle size measurements between EOS images and intra-operative 3D images measurements. Spearman’s rho correlation coefficients were calculated between intra- and extracortical pedicle height and width measurements on EOS and intra-operative 3D images. A Spearman’s rho of 0.90–1.00 indicates a very strong correlation, a rho of 0.70–0.89 indicates a strong correlation, 0.50–0.69 moderate, 0.26–0.49 weak, and < 0.25 indicates little if any correlation [12, 13]. Absolute agreement was evaluated with Bland–Altman plots [14]. If the 95% confidence interval (CI) of the mean difference between the two measurements contains zero, then no systematic bias is present between the measurements on EOS and intra-operative 3D images [15].
ANOVA with post hoc Tukey tests was used to assess the influence of Nash–Moe vertebral rotation score and spinal level on the mean differences between EOS and 3D pedicle size measurements. For this, the data were clustered in three Nash–Moe groups (0, 1, and 2–3) and four spinal level groups (T3-T5, T6-T9, T10-L1, and L2-L5). Since there were only few pedicles with a Nash–Moe score 3, they were clustered with Nash–Moe score 2 as one group.
The relative and absolute intra- and interobserver reliability was determined. The relative intra- and interobserver reliability was assessed by calculating the intraclass correlation coefficients (ICCs) (two-way random, absolute agreement) for each intra- and extracortical pedicle height and width measurements on the EOS radiographs [15]. ICC greater than 0.9 indicates excellent reliability, values of 0.75–0.9 indicate good reliability, values of 0.5–0.7 indicate moderate reliability, and ICCs less than 0.5 are considered to indicate poor reliability [16]. The Bland–Altman method was used to evaluate the absolute intra- and interobserver reliability [14]. IBM SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, NY, USA), was used for statistical analysis. A P-value < 0.05 was considered to be statistically significant.
Results
Patient inclusion and characteristics
Sixteen patients with a mean preoperative Cobb angle of 60 degrees (SD = 6.8) and a mean age of 16 years (SD = 2.6) were included in the study (Table 1). Fourteen patients (87.5%) were female. The total number of pedicles measurements for comparing EOS and 3D imaging was 203. Most patients (81%) had a right thoracic structural scoliosis. Sixty-one pedicles on the concave side with a Nash–Moe grade score ≥ 2 could not be measured.
Validity of EOS measurements
The correlation between the EOS and intra-operative 3D measurements was very strong for the intracortical pedicle height (Spearman’s rho = 0.93) and strong for the intracortical (Spearman’s rho = 0.85) and extracortical (Spearman’s rho = 0.87) pedicle width (Table 2). Significant differences in intracortical pedicle height, intracortical pedicle width, and extracortical pedicle width between EOS and intra-operative 3D measurements were established. The Bland–Altman plots showed a systematic bias in all three measurements. The intracortical pedicle height was systematically measured larger on EOS images (mean height: 9.01 vs. 8.64 mm for EOS and 3D run, respectively). The intra- and extracortical pedicle width was systematically measured smaller on the EOS images than on the intra-operative 3D images (Table 2).
There were no significant differences in extracortical pedicle height between the two measurement methods (Table 2). The Bland–Altman plot showed also no significant bias, and the correlation between the two measure methods was very strong (Spearman’s rho = 0.95). The mean difference of the pedicle size measurements between EOS and 3D varied between 0.06 and 0.43 mm.
Influence of Nash–Moe scores on mean differences between EOS and 3D
The comparisons of EOS and intra-operative 3D measurements of pedicles with a Nash–Moe score 0, 1, and 2–3 are presented in supplementary data 1 in the same way as Table 2. The mean difference of EOS and 3D intracortical pedicle width measurements was significantly larger for pedicles with Nash–Moe score 2–3 (mean difference: − 0.47 mm), compared to pedicles with Nash–Moe score 0 (mean difference: − 0.06, P = 0.03) or Nash–Moe score 1 (mean difference: − 0.16, P = 0.04). No other significant differences between the Nash–Moe groups were observed.
Influence of spinal level on mean differences between EOS and 3D
The mean absolute difference between EOS and 3D intracortical pedicle width measurements was significant smaller for the group pedicles from spinal levels T3–T5, compared to pedicles from spinal levels T10–L1 (mean difference: 0.13 vs. − 0.35 mm for T3–T5 and T10–L1, respectively, P = 0.04). Also for extracortical pedicle width significant smaller mean absolute differences were established for pedicles from spinal levels T3–T5 (mean difference = 0.02 mm) and T6–T9 (mean difference: − 0.29), compared to pedicles from spinal levels T10–L1 (mean difference: − 0.74 mm, P = < 0.01 and P = 0.01, respectively). No other significant differences were found between the different spinal level groups. Box plots of the EOS and intra-operative 3D pedicle size measurements for each spinal level are presented in supplementary data 2–5.
Intraobserver and interobserver reliability
Relative intra- and interobserver reliability was excellent for all pedicle size measurements on EOS (all ICC’s ≥ 0.94, see Tables 3, 4). The mean difference of the measurements varied between 0.02 and 0.37 mm. In the absolute intraobserver reliability analysis, there was no systematic bias between the two EOS intracortical pedicle height and width measurements. A systematic bias was observed in EOS extracortical pedicle height (95% CI = 0.03–0.23 mm) and width measurements (95% CI = 0.01–0.17 mm, see Table 3). Regarding interobserver reliability, there was no systematic bias between EOS intracortical pedicle width measurements. For the EOS intracortical (95% CI = 0.27–0.47 mm) and extracortical pedicle height (95% CI = 0.05–0.27 mm) and extracortical pedicle width (95% CI = 0.15–0.31 mm), a systematic bias was observed (Table 4).
Discussion
The results of this study show a very strong correlation between the EOS and intra-operative 3D measurements for the intra- and extracortical pedicle height and a strong correlation for the intra- and extracortical pedicle width, indicating a good validity of EOS measurements. The mean absolute differences of the measurements between the two methods were small (0.06 mm–0.43 mm), but a systematic bias existed in all measurements, except for the extracortical pedicle height. The correlation was weaker but still strong for pedicles with a Nash–Moe score 2–3, compared to pedicles of vertebral bodies with less rotation. The mean absolute differences were often smaller for pedicles from higher spinal levels, which could be explained by the generally smaller pedicle sizes. Both intra- and interobserver reliability was excellent for all pedicle size measurements on EOS images.
A stronger correlation between EOS and intra-operative 3D measurements was observed for pedicle height measurements (very strong correlation) compared to pedicle width measurements (strong correlation). In particularly, pedicles with a Nash–Moe score 2 or 3 showed weaker correlation for the intra- and extracortical pedicle width measurements. This was expected for two reasons. First, the EOS imaging system uses a C-arm with the result that there should be no divergence in the vertical plane, but there still is in the horizontal plane. Vertebral bodies with pedicles with Nash–Moe score 2 and 3 are generally positioned closer to the apex of the scoliosis curve and therefore wider from the C7 plumb line than vertebral bodies with less rotation. Consequently, these pedicles near the apex have theoretically a more adverse effect of the divergence in the horizontal plane. Since there was a systematically measured smaller intra- and extracortical pedicle width of Nash–Moe 2 and 3 pedicles (mean difference was − 0.47 mm and − 0.51 mm for intra- and extracortical pedicle width measurements, respectively) and no significant difference for pedicles classified as Nash–Moe 0 on the EOS images compared to intra-operative 3D images, the adverse effect of the divergence by the EOS imaging system was not regarded as a relevant factor and vertebral rotation is a more logic explanation for this systematic underestimation.
The transverse and sagittal pedicle axis lines have been described as the ideal pedicle screw trajectory in which each pedicle appeared largest, and are used for pedicle screw placements with intra-operative 3D imaging and navigation systems [5, 17, 18]. Therefore, the vertical plane perpendicular on these two lines was reconstructed at the isthmus of each pedicle for the pedicle size measurements on the intra-operative 3D scans. The isthmus is the smallest part of the pedicle through which a pedicle screw is mostly placed, so the strong correlation between the pedicle size measurements on this vertical plane and size measurements on EOS images found in this study is of great interest for providing a preoperative indication of needed pedicle screw diameters. Although a commonly accepted criterion for pedicle screw diameter selection has not yet been proposed in the literature, the systematic review of studies with recommendations by Solitro et al. (2019) reported a screw diameter ranging from 80% to a maximum value of 125% of the pedicle width [7, 19, 20]. The human cadaver study of Christodoulou et al. (2005) described that the outer screw diameter should match precisely the intracortical pedicle width without ever exceeding the extracortical pedicle width [21]. However, in pediatric populations, the recommendations for maximum screw diameter/pedicle width ratio ranged from 1.15 to 1.25 [7]. These higher values were explained by the relative plasticity of the pedicle cortex in the pediatric spine [20, 22].
Clinical implications
In daily practice, surgeons using free-hand pedicle screw insertion methods can preoperatively reliably measure intra- and extracortical pedicle widths on EOS radiographs for an indication of the needed pedicle screw diameters for those individual pedicles. They should, however, be aware of the small systematic underestimation of the pedicle width measurements on EOS images when measuring visible pedicles from rotated vertebrae. On the other hand, since pedicle screws generally differ 1 mm in diameter sizes, these small underestimations are likely clinically irrelevant. Surgeons performing scoliosis surgeries with intra-operative 3D imaging and a pedicle screw navigation system could also benefit from preoperative knowledge of pedicle sizes, as for determining the optimal screw trajectory less resolution and therefore less radiation is needed, further reducing the intra-operative dose.
Limitations
Intra-operative 3D images were used as a standard technique for pedicle size measurements in this study. Although a preoperative CT is regarded as the gold standard, the intra-operative 3D rotational X-ray technique has also shown an accurate correspondence with anatomic sections [23]. In addition, the intra- and interobserver reliability was excellent for all pedicle size measurements on intra-operative 3D images (ICCs > 0.95, see supplementary data 6, 7).
A limitation of measuring pedicle sizes on EOS radiographs is that not every pedicle of the scoliotic spine can be measured due to overprojection or vertebral rotation. Pedicles on the concave side with a Nash–Moe grade score ≥ 2, for example, cannot be measured. Unfortunately, the pedicle size of convex pedicle at this vertebra is not representative for the contralateral concave pedicle due to the asymmetry in IS [5, 24]. This pedicle asymmetry has also been found in this study when left- and right-sided pedicle sizes were compared on the intra-operative 3D scans (results not shown).
In conclusion, the results of this study indicate a good validity and reliability for pedicle size measurements on EOS radiographs. For pedicles classified as Nash–Moe 0, no significant differences in intra- and extracortical pedicle width were observed, but when measuring pedicles with a Nash–Moe score > 0 surgeons should be aware of a significant systematic small underestimation of the pedicle width measurements on EOS images. As a result, EOS radiographs may be used for a preoperative estimation of pedicle size and subsequent screw diameter in patients with IS.
References
McCormick J, Aebi M, Toby D et al (2013) Pedicle screw instrumentation and spinal deformities: have we gone too far? Eur Spine J 22(Suppl 2):S216–S224
Kotani T, Akazawa T, Sakuma T et al (2014) Accuracy of pedicle screw placement in scoliosis surgery: a comparison between conventional computed tomography-based and O-arm-based navigation techniques. Asian Spine J 8:331–338
Maruyama T, Takeshita K (2008) Surgical treatment of scoliosis: a review of techniques currently applied. Scoliosis 3:6
Stepanovich MMG, Yaszay B (2015) Complications of the treatment of adolescent idiopathic scoliosis. Semin Spine Surg 27:58–61
Brink RC, Schlosser TPC, Colo D et al (2017) Asymmetry of the vertebral body and pedicles in the true transverse plane in adolescent idiopathic scoliosis: a CT-based study. Spine Deform 5:37–45
Chan A, Parent E, Narvacan K et al (2017) Intraoperative image guidance compared with free-hand methods in adolescent idiopathic scoliosis posterior spinal surgery: a systematic review on screw-related complications and breach rates. Spine J 17:1215–1229
Solitro GF, Whitlock K, Amirouche F et al (2019) Currently adopted criteria for pedicle screw diameter selection. Int J Spine Surg 13:132–145
Belmont PJ Jr, Klemme WR, Dhawan A et al (2001) In vivo accuracy of thoracic pedicle screws. Spine 26:2340–2346
Somoskeoy S, Tunyogi-Csapo M, Bogyo C et al (2012) Accuracy and reliability of coronal and sagittal spinal curvature data based on patient-specific three-dimensional models created by the EOS 2D/3D imaging system. Spine J 12:1052–1059
Vidal C, Ilharreborde B, Azoulay R et al (2013) Reliability of cervical lordosis and global sagittal spinal balance measurements in adolescent idiopathic scoliosis. Eur Spine J 22:1362–1367
Lam GC, Hill DL, Le LH et al (2008) Vertebral rotation measurement: a summary and comparison of common radiographic and CT methods. Scoliosis 3:16
Meijer MF, Boerboom AL, Bulstra SK et al (2017) Do CAS measurements correlate with EOS 3D alignment measurements in primary TKA? Knee Surg Sports Traumatol Arthrosc 25:2894–2903
Domholdt E (2000) Physical therapy research: principles and applications. 2nd edn. WB Saunders Co., Philadelophia
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Rankin G, Stokes M (1998) Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clin Rehabil 12:187–199
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Lee DH, Lee SW, Kang SJ et al (2011) Optimal entry points and trajectories for cervical pedicle screw placement into subaxial cervical vertebrae. Eur Spine J 20:905–911
Lien SB, Liou NH, Wu SS (2007) Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J 16:1215–1222
Di Silvestre M, Parisini P, Lolli F et al (2007) Complications of thoracic pedicle screws in scoliosis treatment. Spine (Phila Pa 1976) 32:1655–61
Takeshita K, Maruyama T, Chikuda H et al (2009) Diameter, length, and direction of pedicle screws for scoliotic spine: analysis by multiplanar reconstruction of computed tomography. Spine (Phila Pa 1976) 34:798–803
Christodoulou AG, Apostolou T, Ploumis A et al (2005) Pedicle dimensions of the thoracic and lumbar vertebrae in the Greek population. Clin Anat 18:404–408
Suk SI, Kim WJ, Lee SM et al (2001) Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine (Phila Pa 1976) 26:2049–57
Verlaan JJ, van de Kraats EB, van Walsum T et al (2005) Three-dimensional rotational X-ray imaging for spine surgery: a quantitative validation study comparing reconstructed images with corresponding anatomical sections. Spine (Phila Pa 1976) 30:556–61
Kuraishi S, Takahashi J, Hirabayashi H et al (2013) Pedicle morphology using computed tomography-based navigation system in adolescent idiopathic scoliosis. J Spinal Disord Tech 26:22–28
Acknowledgements
All authors have made direct contributions to the intellectual content of the paper and have approved the final version of the paper. The material in this paper has not been previously published or submitted elsewhere for publication. Each author believes that the manuscript represents honest work. All authors have nothing to disclose. This study was approved by the Medical Ethical Review Board (RR-Number: 201800917). The manuscript submitted does not contain information about medical device(s)/drug(s).
Funding
The authors did not receive support from any organization for the submitted work. No funding was received to assist with the preparation of this manuscript. No funding was received for conducting this study. No funds, Grants, or other support was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peeters, C.M.M., van Houten, L., Kempen, D.H.R. et al. Assessment of pedicle size in patients with scoliosis using EOS 2D imaging: a validity and reliability study. Eur Spine J 30, 3473–3481 (2021). https://doi.org/10.1007/s00586-021-06839-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06839-8