Abstract
Purpose
Knowledge about spinal length and subsequently growth of each individual patient with adolescent idiopathic scoliosis (AIS) helps with accurate timing of both conservative and surgical treatment. Radiographs taken by a biplanar low-dose X-ray device (EOS) have no divergence in the vertical plane and can provide three-dimensional (3D) measurements. Therefore, this study investigated the criterion validity and reliability of EOS spinal length measurements in AIS patients.
Methods
Prior to routine EOS radiograph, a radiographic calibrated metal beads chain (MBC) was attached on the back of 120 patients with AIS to calibrate the images. Spinal lengths were measured from vertebra to vertebra on EOS anteroposterior (AP), lateral view and on the combined 3D EOS view (EOS 3D). These measurements were compared with MBC length measurements. Secondly, intra- and interobserver reliability of length measurements on EOS-images were determined.
Results
50 patients with accurately positioned MBC were included for analysis. The correlations between EOS and MBC were highest for the 3D length measurements. Compared to EOS 3D measurements, the total spinal length was systematically measured 4.3% (mean difference = 1.97 ± 1.12 cm) and 1.9% (mean difference = 0.86 ± 0.63 cm) smaller on individual EOS two-dimensional (2D) AP and lateral view images, respectively. Both intra- and interobserver reliability were excellent for all length measurements on EOS-images.
Conclusion
The results of this study indicate a good validity and reliability for spinal length measurements on EOS radiographs in AIS patients. EOS 3D length measure method is preferred above spinal length measurements on individual EOS AP or lateral view images.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Background
Adolescent idiopathic scoliosis (AIS) is a common, complex three-dimensional (3D) deformity of the spine with a prevalence of 2–3% [1, 2]. The deformity develops during childhood and progresses severely in 0.1–0.3% of the diagnosed adolescents [2]. High spinal growth velocity during early pubertal growth spurt is a predisposing factor for a rapid increase of the deformity [3,4,5]. Since the risk of progression is related to growth and the severity of the curve, knowledge about spinal growth in each patient can help guiding both conservative and surgical treatment in these children. So far, spinal length measurements are often done on coronal radiographs which has the disadvantage of X-ray beam divergence and not including deviations in the sagittal plane [6]. Due to the complex three-dimensionality of the deformity, this could influence the accuracy of growth measurements [6]. Routine computed tomography (CT) scans would allow 3D measurements. However, this is not an option due to the exposure of this young population to high levels of radiation and future risks of cancer [7]. The EOS® imaging system can provide biplanar low-dose radiographs of the whole spine at once, which reduces the amount of radiation substantially in comparison conventional radiographs [8, 9]. The system uses a C-arm so that images have no divergence in the vertical plane allowing more accurate 3D measurements. Despite these advantages, the reliability of EOS 3D measurements for spinal length assessment has not been investigated. Therefore, the aim of this study was to assess the validity and intra- and interobserver reliability of EOS spinal length measurements in patients with AIS.
Methods
Patients
This study was approved by the Medical Ethical Review Board (RR-number: 201800763) and executed in a tertiary care center for scoliosis. Patients were prospectively included from October 2018 to April 2020 after obtaining written informed consent. The inclusion criteria were: (1) patients aged between 12 and 30 years and (2) diagnosed with AIS with (3) a Cobb angle of the major thoracic or lumbar curve of 20 degrees or more. Patients with radiographs in brace, or previous spinal fusion surgery were excluded.
EOS imaging
Prior to the routine biplanar low-dose radiographs of the spine with the EOS system (EOS imaging, Paris, France), a radiographic calibrated chain with metal beads (5 mm in diameter) was taped to the skin on the spinous processes from vertebra C7 to L5 (Fig. 1) [8, 9]. The physician assistant (JB) placed the chain on the skin of all included patients by carefully palpating each individual spinous process to position the chain parallel to the curve before the patient was positioned on the EOS platform in standing position. Subsequently, the biplanar low-dose radiographs of the spine were conducted (Fig. 2).
Two observers (CP and FW) independently examined the EOS images for eligibility. Only radiographs with the metal beads chain (MBC) positioned accurately over the spinous processes in parallel to the spine were included for analysis. Any differences or uncertainty concerning the inclusion of the radiographs was solved in a consensus meeting.
Method of measurements
Two independent observers (CP and JB) analyzed the spine length from vertebra Th1 to L5 on the included EOS radiographs. Both observers were blinded for the scoring of the other observer. One observer (CP) performed all length measurements twice with at least a week between the measurements. For each segment, the distance between points was manually placed on the anteroposterior (AP) and lateral radiograph. For T12 till L5, points were positioned at the centre of each endplate on both the sagittal and coronal image. For levels T1 till T11, only the centre of the upper endplate was defined on both images. Since each point was placed in both projections using the EOS software, both two-dimensional (2D) and 3D spine height of the vertebral body (and intervertebral disc for T12 till L5) could be measured. The distance between all points was automatically measured by the software and the spinal length was defined by summing up all distances (Fig. 2). The spinal length was measured in 2D (AP and lateral) and 3D. Subsequently, the number of metal beads visible on the AP radiograph was counted twice from vertebra Th1 to L5 and multiplied by 5 mm. The metal beads were used to verify calibration of the distance on the X-ray and the sum of metal beads was used to compare the 2D and 3D total spine length in this study. The same measurement method was used for thoracic (lower edge T12 to upper edge T1) and lumbar (lower edge L5 to upper edge L1) spine length measurements to observe potential differences in accuracy between the thoracic and lumbar spine. Finally, MBC length calculations of spinal segments of at least 3 vertebrae with nearly perfect 3D parallel placement of the MBC were analyzed separately to obtain most reliable segmental spine length calibration.
Statistical analyses
Spearman’s rho correlation coefficients were calculated to determine the correlation between EOS 2D and 3D spine length measurements and spine length measurements obtained with the MBC. A Spearman’s rho of 0.90–1.00 is considered to represent a very strong correlation, a Spearman’s rho of 0.70–0.89 represents a strong correlation, 0.50–0.69 moderate, 0.26–0.49 weak, and < 0.25 represents little or negligible correlation [10,11,12]. Criterion validity of EOS was evaluated with the Bland–Altman method using MBC as reference standard [13]. The data were checked for normal distribution. There is no systematic bias if the mean difference between the EOS and MBC length measurements is not significantly different from zero as assessed with a paired-sample T-tests. One-way ANOVA tests were used to assess the influence of major curve Cobb angle on the mean differences between MBC and EOS length measurements. For this, the Cobb angle data were clustered in two groups (Cobb angle below or above 40 degrees).
The intra- and interobserver reliability and agreement were determined by calculating the intraclass correlation coefficients (ICCs) (two-way random, absolute agreement) and using the Bland–Altman method, respectively [13, 14]. For the intra- and interobserver reliability, an ICC greater than 0.9 is considered to represent excellent reliability, a value of 0.75–0.9 represents good reliability, 0.5–0.7 moderate, and an ICC less than 0.5 represents poor reliability [15]. IBM SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses. A P-value < 0.05 was considered to be statistically significant.
Results
Patient characteristics
Of the 120 patients fulfilling the inclusion criteria, 50 patients (41.7%) had good parallel placement of the MBC and were included for analysis. From one patient, only the thoracic length measurements were included, since the placement on the lumbar curve was not considered accurate enough. The mean age of the 50 included patients at time of inclusion was 17.6 years (SD = 3.3) with a range from 12 to 29 years. Forty-five patients (90%) were female. The mean Cobb angle of the major scoliosis curves was 35.7 degrees (SD = 10.2, range = 21.2–59.2). The mean Cobb angle of the thoracic scoliosis curves was 32.5 degrees (SD = 12.4, range = 9.8–59.2) and the mean Cobb angle of the lumbar curves was 24.1 degrees (SD = 9.5, range = 8.0–49.8).
Validity of EOS spine length measurements
The comparison of EOS (2D and 3D) and MBC spine length measurements is shown in Table 1 and Fig. 3. Regarding the spinal segments of at least three vertebrae with parallel placed MBC for the most reliable segmental spine length calibration, all three EOS measure methods showed a very strong correlation with the MBC (Spearman’s rho > 0.99). No significant difference in spinal segment length was observed between EOS 3D and MBC measure methods (mean difference = 0.03, 95% confidence interval = −0.03 to 0.10 cm, P = 0.35), but the spinal segments were systematically measured 3.1 and 1.1% smaller on EOS 2D AP and lateral view images, respectively, compared to MBC measurement (both P < 0.01, Table 1).
Box plots of the difference in length between the MBC measurements and the EOS 3D or EOS 2D (anteroposterior or lateral view) for the total, thoracic and lumbar spine, and for the 39 spinal segments. Spine length measurements are expressed in centimeters. Abbreviations: MBC, length measurements using metal beads chain; 3D, three-dimensional; 2D, two-dimensional; AP, anteroposterior
Regarding the total spine length measurements, a very strong correlation was observed between EOS 3D and MBC (Spearman’s rho = 0.95), and EOS 2D (AP) and MBC (Spearman’s rho = 0.90) length measurements (Table 1). Strong correlation was found between EOS 2D (lateral view) and MBC length measurements (Spearman’s rho = 0.89). Significant differences in length measurements and a systematic bias were observed between EOS 3D and MBC, and EOS 2D (AP) and MBC. The total spinal length was systematically measured 4.3% smaller with EOS 2D AP measurement method (mean difference = 1.97 ± 1.12 cm) compared to the EOS 3D measurement. The EOS 2D lateral measurements underestimated the spinal length with 0.86 ± 0.63 cm (1.9%) compared to the EOS 3D measurement.
When subdividing the data in thoracic and lumbar spine length measurements, very strong correlations were observed between thoracic spine MBC length measurements and all three EOS measurements, and strong correlations between lumbar spine MBC length measurements and all three EOS measurements (Table 1). Compared to EOS 3D measurements, the thoracic spine length was systematically measured 3.7% (mean difference = 1.03 ± 0.81 cm) and 2.1% (mean difference = 0.58 ± 0.53 cm) smaller with EOS 2D AP and lateral, respectively. The lumbar spine length was systematically measured 5.1% (mean difference = 0.87 ± 0.47 cm) and 1.5% (mean difference = 0.26 ± 0.26) smaller with EOS 2D AP and lateral, respectively, compared to EOS 3D measurements.
Figure 4 presents box plots of the difference in total spine length between the MBC measurements and the EOS 3D or EOS 2D (AP or lateral view) of patients with a major curve Cobb angle below and above 40 degrees. The mean difference of EOS 2D (lateral view) and MBC length measurements was significantly larger for patients with a major curve Cobb angle exceeding 40 degrees (mean difference = −0.86 ± 1.02 cm), compared to patients with a major curve Cobb angle below 40 degrees (mean difference = 0.04 ± 0.88 cm, P < 0.01). No significant differences between the different major curve Cobb angle groups were observed for the comparison between MBC measurements and the EOS 3D (P = 0.47) or EOS 2D AP (P = 0.16). The comparisons of MBC and EOS measurements of total spine length of patients with or without a major curve Cobb angle exceeding 40 degrees are presented in supplementary data Table 1.
Box plots of the difference in total spine length between the MBC measurements and the EOS 3D or EOS 2D (AP or lateral view) of patients with a major curve Cobb angle below and above 40 degrees. Spine length measurements are expressed in centimeters. Abbreviations: MBC, length measurements using metal beads chain; 3D, three-dimensional; 2D, two-dimensional; AP, anteroposterior
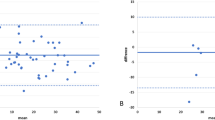
Intraobserver and interobserver reliability
Excellent intra- and interobserver reliability were established for all EOS 3D and 2D total, thoracic and lumbar spine length measurements (ICC’s for intra- and interobserver reliability were respectively ≥ 0.91 and ≥ 0.96, Tables 2, 3). The mean intra-observer differences in length measurements varied between < 0.01 and 0.06 cm and were all not significant (Table 2). The 95% limits of agreement ranged from −1.47 to 1.59 cm. Regarding the interobserver agreement, the mean difference of length measurements varied between 0.01 and 0.22 cm, and the 95% limits of agreement ranged from −0.84 and 1.02 cm. A systematic bias was observed for the EOS 3D total spine (mean difference = 0.14 cm, 95% CI = 0.01–0.27 cm), EOS 2D (AP) total spine (mean difference = 0.22 cm, 95% CI = 0.11–0.33 cm), EOS 3D thoracic spine (mean difference = 0.16 cm, 95% CI = 0.05–0.27 cm), and EOS 2D (AP) thoracic spine length measurements (mean difference = 0.22, 95% CI = 0.14–0.31 cm). There was no systematic bias between the two measurements of all EOS 2D (lateral view) length measurements and EOS 3D and 2D lumbar spine length measurements (Table 3).
Discussion
The results of this study show very strong correlations between EOS 3D and EOS 2D spinal length measurements and a calibration MBC placed over the spinous processes. Although perfect 3D parallel placement of the MBC over the full spinal length is not feasible due to the nature of the deformity, the spinal segments had a near perfect correlation (Spearman’s rho > 0.99) with the MBC indicating a good validity of the EOS system. The correlations were highest for the 3D measurements which respects the 3D nature of the deformity best. Both intra- and interobserver reliability were excellent for all length measurements on EOS-images.
In literature, spinal length measurements are often performed on coronal radiographs which have the disadvantage of X-ray beam divergence and not including deviations in the sagittal plane [6]. Due to the complex three-dimensionality of a scoliosis, 3D measurements could improve the accuracy of spinal length and growth measurements. In this study, the EOS 3D measurements resulted in the best representation of the spinal length. The MBC following the spinal curve resulted in a slight underestimation of the total spine length measurements with a small mean difference (0.59 cm). The significant systematic bias between the two measure methods can be explained by the imperfection in parallel placement of the MBC as calibration chain for the complete spinal length measurements. The MBC was placed over the spinous processes and spinal length was measured at the center of the vertebral bodies. Because of this limitation in the calibration chain, short segments with almost perfect parallel placement of the MBC were included in this validation study. Compared to the EOS 3D length measurements, the EOS 2D measurements structurally underestimated the spinal length. This is not surprising since deviations in the other plane are not taken into account during the measurements of the 3D deformity. Compared to 3D, the 2D measurements on AP and lateral view resulted in 1.97 cm (4.3%) and 0.86 cm (1.9%) underestimation, respectively. Although the mean differences between 2 and 3D EOS measurement methods for total spine length were small, the EOS 3D length measure method could be preferred above spinal length measurements on individual EOS AP or lateral view images. When the EOS 3D length measurements are not possible, spinal length measurements on lateral view images could be preferred above measurements on AP view images if the coronal major curve Cobb angle is beneath 40 degrees. The 2D measurements on AP view resulted in a significant larger underestimation compared to 2D measurements on the lateral view (P < 0.01). There was no significant difference between the two 2D measure methods if the coronal major curve Cobb angle was exceeding 40 degrees (P = 0.41).
Clinical implications
Reliable spine length measure methods would be very useful in daily practice. Knowledge about the spinal growth of each individual patient helps with accurate timing of both conservative and surgical treatment and is necessary to determine and demonstrate the performance of growth-friendly implants [6]. Based on the results, EOS 3D length measure method should be preferred above spinal length measurements on individual AP or lateral view images. It should particularly be considered in clinics where growth-friendly implants are used, since the patient’s ability to grow with these implants is limited. Length measurements on lateral view images could be regarded as alternative when the coronal major curve Cobb angle is beneath 40 degrees.
Limitations
When interpreting the results of this study, a few limitations should be considered. There is no gold standard for spinal length measurements in AIS patients. A metal bead chain was taped over the spine for calibration in this study. However, it was difficult to place the MBC correctly on every single spinous process for parallel placement. Furthermore, the spinous processes are sometimes positioned closer to the midsagittal plane than the vertebral bodies due to the vertebral rotation in a scoliotic spine. Despite these limitations, the MBC was useful as reference for the spinal length measurements and validation of EOS using short segments. Another limitation of this study is that the measure method of spinal length on EOS radiographs is not standardized and therefore labor-intensive. Despite good intra- and interobserver reliability, manual placement of measurement points may possibly be suboptimal because the visualization of vertebral endplates is not always good in the upper thoracic region due to overprojection of the shoulders. Ideally, this spinal length measurement would be captured in a 3D machine learning system. This would be less time-consuming and helpful in accurate planning of both conservative and surgical treatment.
In conclusion, this study shows a good validity and reliability for spinal length measurements on EOS radiographs. The EOS 3D length measure method is preferred above 2D spinal length measurements on EOS AP or lateral views and can be used for total, thoracic, lumbar or segmental spinal length measurements in AIS patients. When the EOS 3D measure method is not possible, spinal length measurements on EOS 2D (lateral view) could be preferred above measurements on EOS 2D (AP view) when coronal Cobb angle is below 40 degrees. In the future, an automated spinal length measurement system would be helpful in accurate timing of treatment.
References
Weinstein SL, Dolan LA, Wright JG et al (2013) Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 369(16):1512–1521. https://doi.org/10.1056/NEJMoa1307337
Negrini S, Aulisa AG, Aulisa L et al (2012) 2011 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 7:3. https://doi.org/10.1186/1748-7161-7-3
Busscher I, Wapstra FH, Veldhuizen AG (2010) Predicting growth and curve progression in the individual patient with adolescent idiopathic scoliosis: design of a prospective longitudinal cohort study. BMC Musculoskelet Disord 11:93. https://doi.org/10.1186/1471-2474-11-93
Busscher I, Gerver WJ, Kingma I et al (2011) The growth of different body length dimensions is not predictive for the peak growth velocity of sitting height in the individual child. Eur Spine J 20:791–797. https://doi.org/10.1007/s00586-010-1584-6
Shi B, Mao S, Liu Z et al (2016) Spinal growth velocity versus height velocity in predicting curve progression in peri-pubertal girls with idiopathic scoliosis. BMC Musculoskelet Disord 17:368. https://doi.org/10.1186/s12891-016-1221-6
Heemskerk JL, Wijdicks SPJ, Altena MC et al. (2020) Spinal growth in patients with juvenile idiopathic scoliosis treated with boston brace: a retrospective study. Spine (Phila Pa 1976) 45:976–982. https://doi.org/10.1097/BRS.0000000000003435
Simony A, Hansen EJ, Christensen SB et al (2016) Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. Eur Spine J 25:3366–3370. https://doi.org/10.1007/s00586-016-4747-2
Somoskeoy S, Tunyogi-Csapo M, Bogyo C et al (2012) Accuracy and reliability of coronal and sagittal spinal curvature data based on patient-specific three-dimensional models created by the EOS 2D/3D imaging system. Spine J 12:1052–1059. https://doi.org/10.1016/j.spinee.2012.10.002
Vidal C, Ilharreborde B, Azoulay R et al (2013) Reliability of cervical lordosis and global sagittal spinal balance measurements in adolescent idiopathic scoliosis. Eur Spine J 22:1362–1367. https://doi.org/10.1007/s00586-013-2752-2
Meijer MF, Boerboom AL, Bulstra SK et al (2017) Do CAS measurements correlate with EOS 3D alignment measurements in primary TKA? Knee Surg Sports Traumatol Arthrosc 25:2894–2903. https://doi.org/10.1007/s00167-016-4031-3
Peeters CMM, van Houten L, Kempen DHR et al (2021) Assessment of pedicle size in patients with scoliosis using EOS 2D imaging: a validity and reliability study. Eur Spine J. https://doi.org/10.1007/s00586-021-06839-8
Domholdt E (2000) Physical therapy research In: Principles and applications. WB Saunders, Philadelphia.
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310. S0140-6736(86)90837-8
Rankin G, Stokes M (1998) Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clin Rehabil 12:187–199. https://doi.org/10.1191/026921598672178340
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Meijer MF, Boerboom AL, Stevens M et al (2014) Assessment of prosthesis alignment after revision total knee arthroplasty using EOS 2D and 3D imaging: a reliability study. PLoS ONE 9:e104613. https://doi.org/10.1371/journal.pone.0104613
Acknowledgements
The authors would like to thank I.M. Nijholt, PhD from the department of Innovation & Science, Isala clinics Zwolle, The Netherlands for her statistical contributions.
Funding
The authors did not receive support from any organization for the submitted work. No funding was received to assist with the preparation of this manuscript. No funding was received for conducting this study. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
All authors have made direct contributions to the intellectual content of the paper and have approved the final version of the paper. The material in this paper has not been previously published or submitted elsewhere for publication. Each author believes that the manuscript represents honest work. All authors have nothing to disclose. This study was approved by the Medical Ethical Review Board (RR-number: 201800763). The Manuscript submitted does not contain information about medical device(s)/drug(s).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peeters, C.M.M., Bos, G.J.F.J., Kempen, D.H.R. et al. Assessment of spine length in scoliosis patients using EOS imaging: a validity and reliability study. Eur Spine J 31, 3527–3535 (2022). https://doi.org/10.1007/s00586-022-07326-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07326-4