Abstract
Background
Advanced cancer patients’ end-of-life care preferences in oncology units, medical-surgical units, nursing homes and palliative care services have been established. However, less is known about end-of-life care preferences of patients with advanced cancer in intensive care units and their families.
Aim
To explore end-of-life care preferences of patients with advanced cancer and their families in intensive care units and if these align with essential elements for end-of-life care.
Design
Electronic databases were searched up to February 2018. Reference lists of retrieved articles were screened for potential studies.
Results
A total of 112 full text articles were retrieved. Of these, 12 articles reporting outcomes from 10 studies were eligible for inclusion. The majority were retrospective chart reviews (n = 7) and conducted in developed countries (n = 9). Care preferences change over time with deteriorating physical condition. Ongoing patient-centred communication and shared decision-making are critical as is teamwork and involvement of a palliative care team. Marital status, gender and ethnicity appear to influence care preferences. Of those studies examining patient preferences and/or the receiving of their preferences, these could be aligned with approximately half of the Australian essential elements for end-of-life care.
Conclusions
Providing end-of-life care for patients with advanced cancer in intensive care units is challenging. No studies have investigated prospectively the end-of-life care preferences of patients and their families in this acute setting. Further research is required to determine the elements of care preferences for patients with advanced cancer and their families in intensive care units in developing countries.

Similar content being viewed by others
References
Sharma N, Sharma AM, Wojtowycz MA, Wang D, Gajra A (2016) Utilization of palliative care and acute care services in older adults with advanced cancer. J Geriatr Oncol 7(1):39–46
Jang RW, Krzyzanowska MK, Zimmermann C, Taback N, Alibhai SM (2015) Palliative care and the aggressiveness of end-of-life care in patients with advanced pancreatic cancer. J Natl Cancer Inst 107(3)
Kim YJ, Kim MJ, Cho YJ, Park JS, Kim JW, Chang H, Lee JO, Lee KW, Kim JH, Yoon HI, Bang SM, Lee JH, Lee CT, Lee JS (2014) Who should be admitted to the intensive care unit? The outcome of intensive care unit admission in stage IIIB-IV lung cancer patients. Med Oncol 31(3):847
World Health Organisation. Cancer: fact sheets 2017 2017 [cited 2017 11 DEC]. Available from: http://www.who.int/mediacentre/factsheets/fs297/en/
Tosi P, Barosi G, Lazzaro C, Liso V, Marchetti M, Morra E, Pession A, Rosti G, Santoro A, Zinzani PL, Tura S (2008) Consensus conference on the management of tumor lysis syndrome. Haematologica. 93(12):1877–1885
Greer JA, Pirl WF, Jackson VA, Muzikansky A, Lennes IT, Heist RS, Gallagher ER, Temel JS (2012) Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non–small-cell lung cancer. J Clin Oncol 30(4):394–400
Worldwide Palliative Care Alliance. Global Atlas of Palliative Care at the End of Life 2014 [cited 2017 22 Nov]. Available from: http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
Australian Commission on Safety and Quality in Health Care (2015) National Consensus Statement: essential elements for safe and high-quality end-of-life care. ACSQHC, Sydney
Canadian Nurses Association.2018 The palliative approach to care and the role of the nurse. Ottawa
The National Institute for health and care excellence. 2015 Care of dying adults in the last days of life.
Kwak J, Haley WE, Chiriboga DA (2008) Racial differences in hospice use and in-hospital death among Medicare and Medicaid dual-eligible nursing home residents. Gerontologist. 48(1):32–41
Levy C, Hutt E, Pointer L (2012) Site of death among veterans living in veterans affairs nursing homes. J Am Med Dir Assoc 13(3):199–201
Ng CW, Cheong SK, Govinda Raj A, Teo W, Leong I (2016) End-of-life care preferences of nursing home residents: results of a cross-sectional study. Palliat Med 30(9):843–853
Shin JA, Parkes A, El-Jawahri A, Traeger L, Knight H, Gallagher ER et al (2016) Retrospective evaluation of palliative care and hospice utilization in hospitalized patients with metastatic breast cancer. Palliat Med 30(9):854–861
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Australian Institute of Health and Welfare.n.d. Informal carer—relationship to care recipient [cited 2017 20 DEC]. Available from: http://meteor.aihw.gov.au/content/index.phtml/itemId/269485
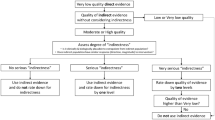
Effective Public Health Practice Project .1998 Quality Assessment Tool For Quantitative Studies [cited 2017. Available from: https://merst.ca/wp-content/uploads/2018/02/quality-assessment-tool_2010.pdf
Truog RD, Campbell ML, Curtis JR, Haas CE, Luce JM, Rubenfeld GD, Rushton CH, Kaufman DC, American Academy of Critical Care Medicine (2008) Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med 36(3):953–963
Romano AM, Gade KE, Nielsen G, Havard R, Harrison JH, Barclay J et al (2017) Early palliative care reduces end-of-life intensive care unit (ICU) use but not ICU course in patients with advanced cancer. Oncologist. 22(3):318–323
Cruz VM, Camalionte L, Caruso P (2015) Factors associated with futile end-of-life intensive care in a cancer hospital. Am J Hosp Palliat Care 32(3):329–334
Miller SJ, Desai N, Pattison N, Droney JM, King A, Farquhar-Smith P, Gruber PC (2015) Quality of transition to end-of-life care for cancer patients in the intensive care unit. Ann Intensive Care 5(1):59
Blechman JA, Rizk N, Stevens MM, Periyakoil VS (2013) Unmet quality indicators for metastatic cancer patients admitted to intensive care unit in the last two weeks of life. J Palliat Med 16(10):1285–1289
Fu S, Hong DS, Naing A, Wheler J, Falchook G, Wen S, Howard A, Barber D, Nates J, Price K, Kurzrock R (2011) Outcome analyses after the first admission to an intensive care unit in patients with advanced cancer referred to a phase I clinical trials program. J Clin Oncol 29(26):3547–3552
Cesta MA, Cardenas-Turanzas M, Wakefield C, Price KJ, Nates JL (2009) Life-supportive therapy withdrawal and length of stay in a large oncologic intensive care unit at the end of life. J Palliat Med 12(8):713–718
Delgado-Guay MO, Parsons HA, Li Z, Palmer LJ, Bruera E (2009) Symptom distress, interventions, and outcomes of intensive care unit cancer patients referred to a palliative care consult team. Cancer. 115(2):437–445
Balboni TA, Balboni M, Enzinger AC, Gallivan K, Paulk ME, Wright A, Steinhauser K, VanderWeele TJ, Prigerson HG (2013) Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Intern Med 173(12):1109–1117
Loggers ET, Maciejewski PK, Paulk E, DeSanto-Madeya S, Nilsson M, Viswanath K, Wright AA, Balboni TA, Temel J, Stieglitz H, Block S, Prigerson HG (2009) Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol 27(33):5559–5564
Hwang IC, Keam B, Yun YH, Ahn HY, Kim YA (2015) Quality of life changes and intensive care preferences in terminal cancer patients. Palliat Support Care 13(5):1309–1316
Sharma RK, Prigerson HG, Penedo FJ, Maciejewski PK (2015) Male-female patient differences in the association between end-of-life discussions and receipt of intensive care near death. Cancer. 121(16):2814–2820
Kinoshita S, Miyashita M (2012) Evaluation of end-of-life cancer care in the ICU: perceptions of the bereaved family in Japan. Am J Hosp Palliat Care 30(3):225–230
Dennis BK (2014) Understanding participant experiences: reflections of a novice research participant. Int J Qual Methods 13(1):395–410
Wickson-Griffiths A, Kaasalainen S, Ploeg J, McAiney C (2014) Revisiting retrospective chart review: an evaluation of nursing home palliative and end-of-life care research. Palliat Med Care 1(2):8
Sutton J, Austin Z (2015) Qualitative research: data collection, analysis, and management. Can J Hosp Pharm 68(3):226–231
Kastbom L, Milberg A, Karlsson M (2017) A good death from the perspective of palliative cancer patients. Support Care Cancer 25(3):933–939
Miyashita M, Morita T, Sato K, Hirai K, Shima Y, Uchitomi Y (2008) Good death inventory: a measure for evaluating good death from the bereaved family member’s perspective. J Pain Symptom Manag 35(5):486–498
Hammami MM, Al-Jawarneh Y, Hammami MB, Al Qadire M (2014) Information disclosure in clinical informed consent: "reasonable" patient's perception of norm in high-context communication culture. BMC Med Ethics 15:3
Mohan D, Alexander SC, Garrigues SK, Arnold RM, Barnato AE (2010) Communication practices in physician decision-making for an unstable critically ill patient with end-stage cancer. J Palliat Med 13(8):949–956
Virdun C, Luckett T, Lorenz K, Davidson PM, Phillips J (2017) Dying in the hospital setting: a meta-synthesis identifying the elements of end-of-life care that patients and their families describe as being important. Palliat Med 31(7):587–601
Phelps AC, Lauderdale KE, Alcorn S, Dillinger J, Balboni MT, Van Wert M et al (2012) Addressing spirituality within the care of patients at the end of life: perspectives of patients with advanced cancer, oncologists, and oncology nurses. J Clin Oncol 30(20):2538–2544
Virdun C, Luckett T, Davidson PM, Phillips J (2015) Dying in the hospital setting: a systematic review of quantitative studies identifying the elements of end-of-life care that patients and their families rank as being most important. Palliat Med 29(9):774–796
UK Department of Health (2008) End of life care strategy. In: Life PHQCfAAatEo, editor. London: UK Department of Health
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
The author(s) also declare that they have full control of all primary data and that they agree to allow the journal to review their data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 47 kb)
Rights and permissions
About this article
Cite this article
Alyami, H.M., Chan, R.J. & New, K. End-of-life care preferences for people with advanced cancer and their families in intensive care units: a systematic review. Support Care Cancer 27, 3233–3244 (2019). https://doi.org/10.1007/s00520-019-04844-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04844-8