Abstract
Background
Surgeons’ overload is one of the main causes of medical errors that might compromise patient safety. Due to the drawbacks of current options to monitor surgeons’ load, new, sensitive, and objective indices of task (over)load need to be considered and tested. In non-health-care scenarios, intraocular pressure (IOP) has been proved to be an unbiased physiological index, sensitive to task complexity (one of the main variables related to overload), and time on task. In the present study, we assessed the effects of demanding and complex simulated surgical procedures on surgical and medical residents’ IOP.
Methods
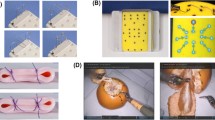
Thirty-four surgical and medical residents and healthcare professionals took part in this study (the experimental group, N = 17, and the control group, N = 17, were matched for sex and age). The experimental group performed two simulated bronchoscopy procedures that differ in their levels of complexity. The control group mimicked the same hand-eye movements and posture of the experimental group to help control for the potential effects of time on task and re-measurement on IOP. We measured IOP before and after each procedure, surgical performance during procedures, and perceived task complexity.
Results
IOP increased as consequence of performing the most complex procedure only in the experimental group. Consistently, residents performed worse and reported higher perceived task complexity for the more complex procedure.
Conclusions
Our data show, for the first time, that IOP is sensitive to residents’ task load, and it could be used as a new index to easily and rapidly assess task (over)load in healthcare scenarios. An arousal-based explanation is given to describe IOP variations due to task complexity.
Graphical Abstract


Similar content being viewed by others
References
Pham JC, Aswani MS, Rosen M, Lee H, Huddle M, Weeks K, Pronovost PJ (2012) Reducing medical errors and adverse events. Annu Rev Med 63:447–463. https://doi.org/10.1146/annurev-med-061410-121352
Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA, Fink AS, Mentzer RM, Steeger JE (2007) The patient safety in surgery study: background, study design, and patient populations. J Am Coll Surg 204:1089–1102. https://doi.org/10.1016/j.jamcollsurg.2007.03.028
Di Stasi LL, Diaz-Piedra C, Rieiro H, Sánchez Carrión JM, Martin Berrido M, Olivares G, Catena A (2016) Gaze entropy reflects surgical task load. Surg Endosc 30:5034–5043. https://doi.org/10.1007/s00464-016-4851-8
Di Stasi LL, Diaz-Piedra C, Ruiz-Rabelo JF, Rieiro H, Sanchez Carrion JM, Catena A (2017) Quantifying the cognitive cost of laparo-endoscopic single-site surgeries: gaze-based indices. Appl Ergon 65:168–174
Galy E, Cariou M, Mélan C (2012) What is the relationship between mental workload factors and cognitive load types? Int J Psychophysiol 83:269–275. https://doi.org/10.1016/j.ijpsycho.2011.09.023
Zheng B, Tien G, Atkins SM, Swindells C, Tanin H, Meneghetti A, Qayumi KA, Neely O, Panton M (2011) Surgeon’s vigilance in the operating room. Am J Surg 201:667–671. https://doi.org/10.1016/j.amjsurg.2011.01.016
Rubio S, Díaz E, Martín J, Puente JM (2004) Evaluation of subjective mental workload: a comparison of SWAT, NASA-TLX, and workload profile methods. Appl Psychol 53:61–86. https://doi.org/10.1111/j.1464-0597.2004.00161.x
Ruiz-Rabelo JF, Navarro-Rodriguez E, Di-Stasi LL, Diaz-Jimenez N, Cabrera-Bermon J, Diaz-Iglesias C, Gomez-Alvarez M, Briceño-Delgado J (2015) Validation of the NASA-TLX score in ongoing assessment of mental workload during a laparoscopic learning curve in bariatric surgery. Obes Surg 25:2451–2456. https://doi.org/10.1007/s11695-015-1922-1
Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP (2003) Common method biases in behavioural research: a critical review of the literature and recommended remedies. J Appl Psychol 88:879–903
Di Stasi LL, McCamy MB, Macknik SL, Mankin JA, Hooft N, Catena A, Martinez-Conde S (2014) Saccadic eye movement metrics reflect surgical residents’ fatigue. Ann Surg 259:824–829. https://doi.org/10.1097/SLA.0000000000000260
Di Stasi LL, Antolí A, Cañas JJ (2011) Main sequence: an index for detecting mental workload variation in complex tasks. Appl Ergon 42:807–813. https://doi.org/10.1016/j.apergo.2011.01.003
Diaz-Piedra C, Sanchez-Carrion JM, Rieiro H, Di Stasi LL (2017) Gaze-based technology as a tool for surgical skills assessment and training in urology. Urology 107:26–30. https://doi.org/10.1016/j.urology.2017.06.030
Zheng B, Jiang X, Tien G, Meneghetti A, Panton ONM, Atkins MS (2012) Workload assessment of surgeons: correlation between NASA TLX and blinks. Surg Endosc 26:2746–2750. https://doi.org/10.1007/s00464-012-2268-6
Zheng B, Jiang X, Atkins MS (2015) Detection of changes in surgical difficulty: evidence from pupil responses. Surg Innov 22:1–7. https://doi.org/10.1177/1553350615573582
Schulz CM, Schneider E, Fritz L, Vockeroth J, Hapfelmeier A, Wasmaier M, Kochs EF, Schneider G (2011) Eye tracking for assessment of workload: a pilot study in an anaesthesia simulator environment. Br J Anaesth 106:44–50. https://doi.org/10.1093/bja/aeq307
Gherghel D, Hosking SL, Orgül S (2004) Autonomic nervous system, circadian rhythms, and primary open-angle glaucoma. Surv Ophthalmol 49:491–508. https://doi.org/10.1016/j.survophthal.2004.06.003
Wang C-A, Munoz DP (2015) A circuit for pupil orienting responses: implications for cognitive modulation of pupil size. Curr Opin Neurobiol 33:134–140. https://doi.org/10.1016/j.conb.2015.03.018
Vera J, Diaz-Piedra C, Jiménez R, Morales JM, Catena A, Cardenas D, Di Stasi LL (2016) Driving time modulates accommodative response and intraocular pressure. Physiol Behav. https://doi.org/10.1016/j.physbeh.2016.05.043
Vera J, Jiménez R, García JA, Cárdenas D (2017) Intraocular pressure is sensitive to cumulative and instantaneous mental workload. Appl Ergon 60:313–319. https://doi.org/10.1016/j.apergo.2016.12.011
Vera J, García-Ramos A, Jiménez R, Cárdenas D (2017) The acute effect of strength exercises at different intensities on intraocular pressure. Graefe’s Arch Clin Exp Ophthalmol 255:2211–2217. https://doi.org/10.1007/s00417-017-3735-5
Brody S, Erb C, Veit R, Rau H (1999) Intraocular pressure changes: the influence of psychological stress and the Valsalva maneuver. Biol Psychol 51:43–57. https://doi.org/10.1016/S0301-0511(99)00012-5
Faul F, Erdfelder E, Lang A-G, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191. https://doi.org/10.3758/BF03193146
Chakraborty R, Read SA, Collins MJ (2011) Diurnal variations in axial length, choroidal thickness, intraocular pressure, and ocular biometrics. Investig Ophthalmol Vis Sci 52:5121–5129. https://doi.org/10.1167/iovs.11-7364
Bakke EF, Hisdal J, Semb SO (2009) Intraocular pressure increases in parallel with systemic blood pressure during isometric exercise. Investig Ophthalmol Vis Sci 50:760–764. https://doi.org/10.1167/iovs.08-2508
Takenaka J, Kunihara E, Rimayanti U, Tanaka J, Kaneko M, Kiuchi Y (2015) Intraocular pressure readings obtained through soft contact lenses using four types of tonometer. Clin Ophthalmol 9:1875–1881
Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC (1973) Quantification of sleepiness: a new approach. Psychophysiology 10:431–436
Morales JM, Díaz-Piedra C, Rieiro H, Roca-González J, Romero S, Catena A, Fuentes LJ, Di Stasi LL (2017) Monitoring driver fatigue using a single-channel electroencephalographic device: a validation study by gaze-based, driving performance, and subjective data. Accid Anal Prev 109:62–69. https://doi.org/10.1016/j.aap.2017.09.025
Prata TS, De Moraes CG, Kanadani FN, Ritch R, Paranhos A (2010) Posture-induced intraocular pressure changes: considerations regarding body position in glaucoma patients. Surv Ophthalmol 55:445–453. https://doi.org/10.1016/j.survophthal.2009.12.002
Mélan C, Cascino N (2014) A multidisciplinary approach of workload assessment in real-job situations: Investigation in the field of aerospace activities. Front Psychol 5:1–13. https://doi.org/10.3389/fpsyg.2014.00964
Ost D, De Rosiers A, Britt EJ, Fein AM, Lesser ML, Mehta AC (2001) Assessment of a bronchoscopy simulator. Am J Respir Crit Care Med 164:2248–2255
Goldmann K, Steinfeldt T (2006) Acquisition of basic fiberoptic intubation skills with a virtual reality airway simulator. J Clin Anesth 18:173–178. https://doi.org/10.1016/j.jclinane.2005.08.021
Nassar M, Rumsey K, Wilson R, Parikh K, Heasly B, Gold J (2013) Rational regulation of learning dynamics by pupil–linked arousal systems. Nat Neurosci 15:1040–1046. https://doi.org/10.1038/nn.3130.Rational
Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, Benumof JL, Berry FA, Bode RH, Cheney FW (2013) Practice guidelines for management of the difficult airwayan updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. J Am Soc Anesthesiol 118:251–270
Manski CF (2013) Diagnostic testing and treatment under ambiguity: using decision analysis to inform clinical practice. Proc Natl Acad Sci. https://doi.org/10.1073/pnas.1221405110/-/DCSupplemental
Davies LN, Bartlett H, Mallen EAH, Wolffsohn JS (2006) Clinical evaluation of rebound tonometer. Acta Ophthalmol Scand 84:206–209. https://doi.org/10.1111/j.1600-0420.2005.00610.x
Rüfer F, Schiller J, Klettner A, Lanzl I, Roider J, Weisser B (2014) Comparison of the influence of aerobic and resistance exercise of the upper and lower limb on intraocular pressure. Acta Ophthalmol 92:249–252. https://doi.org/10.1111/aos.12051
Armstrong R (2013) Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol Opt 33:7–14. https://doi.org/10.1111/opo.12009
Hoddes E, Zarcone V, Dement W (1972) Development and use of Stanford Sleepiness scale (SSS). Psychophysiology 9:150
Hart SG, Staveland LE (1988) Development of NASA-TLX (task load index): Results of empirical and theorical research. In: Hum. Ment. Workload. pp 139–183
Hart SG (2006) Nasa-task load index (NASA-TLX); 20 years later. Proc Hum Factors Ergon Soc Annu Meet 50:904–908. https://doi.org/10.1177/154193120605000909
Colt HG, Crawford SW, Galbraith O (2001) Virtual reality bronchoscopy simulation. Chest 120:1333–1339. https://doi.org/10.1378/chest.120.4.1333
Davoudi M, Colt HG (2009) Bronchoscopy simulation: a brief review. Adv Heal Sci Educ 14:287–296. https://doi.org/10.1007/s10459-007-9095-x
Jiménez R, Vera J (2018) Effect of examination stress on intraocular pressure in university students. Appl Ergon 67:252–258. https://doi.org/10.1016/j.apergo.2017.10.010
Yerkes RM, Dodson JD (1908) The relation of strength of stimulus to rapidity of habit-formation in the kitten. J Comp Neurl Psychol 5:330–336. https://doi.org/10.1037/h0073415
Di Stasi LL, Catena A, Cañas JJ, Macknik SL, Martinez-Conde S (2013) Saccadic velocity as an arousal index in naturalistic tasks. Neurosci Biobehav Rev 37:968–975. https://doi.org/10.1016/j.neubiorev.2013.03.011
Siegenthaler E, Costela FM, Mccamy MB, Di Stasi LL, Otero-Millan J, Sonderegger A, Groner R, Macknik S, Martinez-Conde S (2014) Task difficulty in mental arithmetic affects microsaccadic rates and magnitudes. Eur J Neurosci 39:287–294. https://doi.org/10.1111/ejn.12395
Goldwater B (1972) Psychological significance of pupillary movements. Psychol Bull 77:340–355
Mansouri K, Weinreb RN, Liu JHK (2015) Efficacy of a contact lens sensor for monitoring 24-H intraocular pressure related patterns. PLoS ONE 10:1–14. https://doi.org/10.1371/journal.pone.0125530
De Smedt S, Mermoud A, Schnyder C (2012) 24-hour intraocular pressure fluctuation monitoring using an ocular telemetry sensor. J Glaucoma 21:539–544. https://doi.org/10.1097/IJG.0b013e31821dac43
Jackson ML, Kennedy GA, Clarke C, Gullo M, Swann P, Downey LA, Hayley AC, Pierce RJ, Howard ME (2016) The utility of automated measures of ocular metrics for detecting driver drowsiness during extended wakefulness. Accid Anal Prev 87:127–133. https://doi.org/10.1016/j.aap.2015.11.033
Hunt AP, Feigl B, Stewart IB (2012) The intraocular pressure response to dehydration: a pilot study. Eur J Appl Physiol 112:1963–1966. https://doi.org/10.1007/s00421-011-2143-5
Li M, Wang M, Guo W, Wang J, Sun X (2011) The effect of caffeine on intraocular pressure: a systematic review and meta-analysis. Graefe’s Arch Clin Exp Ophthalmol 249:435–442. https://doi.org/10.1007/s00417-010-1455-1
Gaba DM, Howard SK (2002) Patient safety: fatigue among clinicians and the safety of patients. N Engl J Med 347:1249–1255. https://doi.org/10.1056/NEJMsa020846
Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, Czeisler CA (2006) Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med 3:2440–2448. https://doi.org/10.1371/journal.pmed.0030487
Stefanidis D, Korndorffer JR, Black FW, Dunne JB, Sierra R, Touchard CL, Rice DA, Markert RJ, Kastl PR, Scott DJ (2006) Psychomotor testing predicts rate of skill acquisition for proficiency-based laparoscopic skills training. Surgery 140:252–262. https://doi.org/10.1016/j.surg.2006.04.002
Harris CJ, Herbert M, Steele RJC (1994) Psychomotor skills of surgical trainees compared with those of different medical specialists. Br J Surg 81:382–383. https://doi.org/10.1002/bjs.1800810319
Yamaguchi S, Konishi K, Yasunaga T, Yoshida D, Kinjo N, Kobayashi K, Ieiri S, Okazaki K, Nakashima H, Tanoue K, Maehara Y, Hashizume M (2007) Construct validity for eye-hand coordination skill on a virtual reality laparoscopic surgical simulator. Surg Endosc Other Interv Tech 21:2253–2257. https://doi.org/10.1007/s00464-007-9362-1
Acknowledgements
Research by LLDS was supported by the BBVA Foundation, Madrid, Spain (Grant No. 2015-2) and is currently supported by the Ramón y Cajal fellowship program (RYC-2015-17483). We thank IAVANTE staff (Andalusian Public Foundation for Progress and Health) for their help during data collection. We thank Dr. G. A. Koulieris (Inria, Université Côte d’Azur, France) for proofreading the paper.
Funding
This study was funded by the Campus of International Excellence (BioTic Granada) Research Programme (Research Project V7-2015 to CDP). The funding source had no role in the design or conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Vera, Diaz-Piedra, Jiménez, Sanchez-Carrion, and Di Stasi have no conflicts of interest or financial ties to disclose.
Appendix
Appendix
Before starting the procedure, participants read the following information:
For the Procedure A, A 5-year-old child scheduled for split thickness skin grafts (STSG). He was burned in a house fire 5 months ago and has 70% TBA burns. He has required multiple anesthetics for burn dressing changes and STSGs. His last anesthetic, 2 weeks ago, was discussed extensively in your department because the anesthesiologist had a very difficult time intubating the patient, due to a Grade 3 view with laryngoscopy. It is decided that the safest way to intubate this patient is with a fiberoptic bronchoscope.
On physical exam, the child has extensive burn scars and contractures. The scarring on his face and anterior neck severely restricts his ability to open his mount or extend his head.
For the Procedure B, A 42 years old female who presents with several episodes of blood-streaked sputum. She smoked for 10 years, but quit 5 years ago. On physical examination, she is afebrile and appears well. Her blood pressure is 110/75, pulse is 84, temperature is 98.4 F, and respiratory rate is 14. No abnormalities are noted on auscultation of the chest. No lymphadenopathy is present. Her chest radiographs are normal.
Please perform flexible bronchoscopy to identify the location of any lesions that you can visualize. Capture an image of each lesion identified by depressing the video capture button on the bronchoscope.
Rights and permissions
About this article
Cite this article
Vera, J., Diaz-Piedra, C., Jiménez, R. et al. Intraocular pressure increases after complex simulated surgical procedures in residents: an experimental study. Surg Endosc 33, 216–224 (2019). https://doi.org/10.1007/s00464-018-6297-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6297-7