Abstract
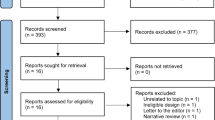
Although antimicrobials are the cornerstone of neonatal sepsis management, adjunctive therapies are required to improve outcomes. The aim of our study was to evaluate the effect of exchange transfusion (ET) on mortality (primary outcome) in neonatal sepsis, as well as on immunoglobulin, complement and neutrophil levels and assess its complications (secondary outcomes). Databases searched include PubMed, NCBI, Google Scholar, CINHAL, Ovid and Scopus. Randomized controlled trials (RCTs), controlled observational studies (COSs) and uncontrolled observational studies (UOSs) reporting mortality data from using ET in neonatal sepsis were included. Studies with additional interventions, non-septic ET indications and populations aged > 28 days were excluded. Data extracted include demographics, features of study, sepsis and ET, as well as mortality rates, immunological and laboratory changes and complications. Data was meta-analysed and displayed using forest plots. The meta-analysis of 14 studies (3 RCTs, 11 COSs) revealed a mortality benefit in septic neonates who underwent ET-RR 0.72 (CI 0.61–0.86, p = 0.01) and a significant increase in pooled immunological parameters (immunoglobulin, complement levels) (SMD 1.13, [0.25, 2.02], p = 0.02) and neutrophil levels (SMD 1.07 [0.04, 2.11], p = 0.03) compared to controls. The descriptive analysis of 9 UOSs revealed thrombocytopenia as the most frequently reported complication (n = 48). Moderate–high risk of bias was largely due to inadequate sample sizes and follow-up durations.
Conclusion: Currently, the use of ET in neonatal sepsis is not directly recommended due to low certainty of evidence, inadequate power and moderate–high risk of bias and heterogeneity.
Trial registration: PROSPERO (CRD42020176629) (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=176629)
What is Known: • Exchange transfusion is one of the adjunctive methods for treatment of neonatal sepsis. | |
What is New: • The pooled analysis of all studies shows that exchange transfusion has a low certainty of evidence in the context of neonatal mortality. However, at this point, this intervention cannot be refuted or recommended due to heterogeneity of studies and inadequate power. |






Similar content being viewed by others
Abbreviations
- AMR:
-
Antimicrobial resistance
- CCF:
-
Congestive cardiac failure
- CI:
-
Confidence intervals
- CSF:
-
Cerebrospinal fluid
- DVET:
-
Double volume exchange transfusion
- ET:
-
Exchange Transfusion
- GBS:
-
Group B streptococci
- G-CSF:
-
Granulocyte colony stimulating factor
- GM-CSF:
-
Granulocyte monocyte colony stimulation factor
- HMD:
-
Hyaline membrane disease
- NHLBI:
-
National Heart, Lung and Blood Institute
- NOS:
-
Newcastle-Ottawa Scale
- PDA:
-
Patent ductus arteriosus
- RCT:
-
Randomized controlled trial
- RR:
-
Risk ratio
- SMD:
-
Standardized mean difference
- SVET:
-
Single volume exchange transfusion
- TRALI:
-
Transfusion-related acute lung injury
References
Bohanon FJ, Nunez Lopez O, Adhikari D et al (2018) Race, income and insurance status affect neonatal sepsis mortality and healthcare resource utilization. Pediatr Infect Dis J 37:e178–e184. https://doi.org/10.1097/INF.0000000000001846
Ranjeva SL, Warf BC, Schiff SJ (2018) Economic burden of neonatal sepsis in sub-Saharan Africa. BMJ Glob Health 3. https://doi.org/10.1136/bmjgh-2017-000347
Agarwal R, Chaurasia S, Jeeva Sankar M et al (2016) Characterisation and antimicrobial resistance of sepsis pathogens in neonates born in tertiary care centres in Delhi, India: A cohort study. Lancet Glob Health 4:e752–e760. https://doi.org/10.1016/S2214-109X(16)30148-6
Tarnow-Mordi W, Isaacs D, Dutta S (2010) Adjunctive immunologic interventions in neonatal sepsis. Clinics in Perinatology 37:481–499. https://doi.org/10.1016/j.clp.2009.12.002
Falciglia HS, Greenwood CS (2013) Double volume exchange transfusion: A review of the “Ins and Outs.” In: NeoReviews. https://www.researchgate.net/publication/270456970_Double_Volume_Exchange_Transfusion_A_Review_of_the_Ins_and_Outs. Accessed 28 Jun 2020
Liberati A, Altman DG, Tetzlaff J, et al 2009 The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed) 339. https://doi.org/10.1136/bmj.b2700
McMaster University, Evidence Prime Inc (2015) GRADEpro GDT: GRADEpro Guideline Development Tool [Software]
Harrer M, Cuijpers P, Furukawa TA, Ebert DD (2019) Doing meta-analysis in R: a hands-on guide. PROTECT Lab Erlangen
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557 LP – 560. https://doi.org/10.1136/bmj.327.7414.557
Ac J, Hernán MA, Reeves BC, et al (2016) The risk of bias in non-randomized studies – of Interventions (ROBINS-I) assessment tool (version for cohort-type studies) ROBINS-I tool (stage I): at protocol stage ROBINS-I tool (stage II): For each study Specify a target randomized trial specif. 1–22
Pt J, Savović J, Page MJ, Sterne JAC (2019) Revised Cochrane risk-of-bias tool for randomized trials ( RoB 2 )
Mathur NB, Subramanian BK, Sharma VK, Puri RK (1993) Exchange transfusion in neutropenic septicemic neonates: effect on granulocyte functions. Acta Paediatrica (Oslo, Norway: 1992) 82:939–943. https://doi.org/10.1111/j.1651-2227.1993.tb12604.x
Sadana S, Mathur NB, Thakur A (1997) Exchange transfusion in septic neonates with sclerema: effect on immunoglobulin and complement levels. Indian Pediatr 34:20–25
Aradhya AS, Sundaram V, Kumar P et al (2016) Double volume exchange transfusion in severe neonatal sepsis. Indian J Pediatr 83:107–113. https://doi.org/10.1007/s12098-015-1841-0
Pugni L, Ronchi A, Bizzarri B et al (2016) Exchange transfusion in the treatment of neonatal septic shock: a ten-year experience in a neonatal intensive care unit. Int J Mol Sci 17:1–12. https://doi.org/10.3390/ijms17050695
Rajput U, L.S.D (2013) Exchange transfusion in neonatal sepsis does not reduces overall mortality. J Evol Med Den Sci 2:8297–8301. https://doi.org/10.14260/jemds/1456
Gunes T, Koklu E, Buyukkayhan D et al (2006) Exchange transfusion or intravenous immunoglobulin therapy as an adjunct to antibiotics for neonatal sepsis in developing countries: A pilot study. Ann Trop Paediatr 26:39–42. https://doi.org/10.1179/146532806X90592
Töllner U, Pohlandt F, Heinze F et al (1977) Treatment of septicaemia in the newborn infant: choice of initial antimicrobial drugs and the role of exchange transfusion. Acta Paediatr Scand 66:605–610. https://doi.org/10.1111/j.1651-2227.1977.tb07955.x
Prod’hom LS, Choffat JM, Frenck N et al (1974) Care of the seriously ill neonate with hyaline membrane disease and with sepsis (sclerema neonatorum). Pediatrics 53:170–181
Narayanan I, Mitter A, Gujral VV (1982) A comparative study on the value of exchange and blood transfusion in the management of severe neonatal septicemia with sclerema. Ind J Pediatr 49:519–523. https://doi.org/10.1007/BF02834557
Verma A, Pandita A, Gupta G et al (2020) Role of DVET in severe neonatal sepsis in an era of high antibiotic resistance: A retrospective observational study. J Matern-Fetal Neonatal Med 1:6. https://doi.org/10.1080/14767058.2020.1771303
Togari H, Mikawa M, IWANAGA T, et al (1983) Endotoxin clearance by exchange blood transfusion in septic shock neonates. Acta Paediatr Scand 72:87–91. https://doi.org/10.1111/j.1651-2227.1983.tb09669.x
Dalvi R, Rao S, Rangnekar J, Fernandez A (1991) Exchange transfusions in neonatal sepsis. Indian pediatrics 28:39–43
De Curtis M, Vetrano G, Romano G et al (2020) Improvement tetrazolium ttransfusions immunizations of phagocytosis reduction in two after preterm and nitroblue with exchange infants septicemia. 829–830
Christensen RD, Hill HR, Anstall HB, Rothstein G (1984) Exchange transfusion as an alternative to granulocyte concentrate administration in neonates with bacterial sepsis and profound neutropenia. J Clin Apher 2:177–183. https://doi.org/10.1002/jca.2920020206
Vain NE, Mazlumian JR, Swarner OW, Cha CC (1980) Role of exchange transfusion in the treatment of severe septicemia. Pediatrics 66:693–697
Bossi E, Meister B, Pfenninger J (1981) Exchange transfusion for severe neonatal septicemia. Pediatrics 67:941
Kokk T, Talvik R, Zilmer M, et al (2010) Markers of oxidative stress before and after exchange transfusion for neonatal sepsis. Acta Paediatr 85:1244–1246. https://doi.org/10.1111/j.1651-2227.1996.tb18239.x
Hall R, Shigeoka A, Hill H (1983) Serum opsonic activity and peripheral neutrophil counts before and after exchange transfusion in infants with early onset group B streptococcal septicaemia. Pediatric Infectious Disease 2:356–358
Courtney SSS, Hall RR, Harris DDDD (1979) Effect of blood-transfusions on mortality in early-onset group-b streptococcal septicemia. Lancet 462
Pearse SP (1978) Exchange Transfusion in treatment of severe infections in newborns and of sclerema neonatorum. Arch Dis Child 53:262. https://doi.org/10.1054/cupe.2001.0272
Belohradsky BH, Roos R, Marget W (1978) Exchange transfusion in neonatal septicemia — clinical and immunological results in vivo and in vitro. Infection 6:139–144. https://doi.org/10.1007/BF01646086
Lemos L (1981) Exchange transfusion in treatment of sepsis. Pediatrics 68:471–472
Xanthou M, Mandyla H, Photopoulos S (1985) The use of exchange transfusions, immunoglobulins and granulocyte transfusions in neonatal sepsis. In: Ross Laboratories Special Conference Washington DC
Fleischmann-Struzek C, Goldfarb DM, Schlattmann P et al (2018) The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med 6:223–230
Wynn JL (2016) Defining neonatal sepsis. Curr Opin Pediatr 28:135–140. https://doi.org/10.1097/MOP.0000000000000315
Pelet B, Pediatrie S De, Hospitalier C, Vaudois U (1979) Exchange transfusion in newborn infants: Effects on granulocyte function. 687–690
Patra K, Storfer-Isser A, Siner B et al (2004) Adverse events associated with neonatal exchange transfusion in the 1990s. J Pediatr 144:626–631. https://doi.org/10.1016/j.jpeds.2004.01.054
Jc J (2020) Adverse events associated with exchange transfusion in healthy and ill newborns. Pediatrics
Chacham S, Kumar J, Dutta S, Kumar P (2019) Adverse events following blood exchange transfusion for neonatal hyperbilirubinemia: a prospective study. J Clin Neonatol 8:79–84. https://doi.org/10.4103/jcn.JCN
Wolf MF, Childers J, Gray KD, et al (2020) Exchange transfusion safety and outcomes in neonatal hyperbilirubinemia. J Perinatol. https://doi.org/10.1038/s41372-020-0642-0
Murakami Y, Yamashita Y, Nishimi T, et al (1998) Changes of cerebral hemodynamics and oxygenation in unstable septic newborns during exchange transfusion. Kurume Med J 45:321–325. https://doi.org/10.2739/kurumemedj.45.321
Piasek CZ, Bel FV, Sola A (2014) Perfusion index in newborn infants: a noninvasive tool for neonatal monitoring. Acta Paediatr 103:468–473. https://doi.org/10.1111/apa.12574
Monin P, Vert P, Andre M, Vibert M (1979) Transcutaneous PO2 monitoring (tcPO2) in the newborn during apneic spells, convulsions, cardiac catheterizations, and exchange transfusions. Birth Defects Orig Artic Ser 15:469–491
Taylor AW, Blau DM, Bassat Q, et al (2020) Initial findings from a novel population-based child mortality surveillance approach: a descriptive study. Lancet Glob Health 8:e909–e919. https://doi.org/10.1016/S2214-109X(20)30205-9
Saha SK, Schrag SJ, El Arifeen S, et al (2018) Causes and incidence of community-acquired serious infections among young children in South Asia (ANISA): an observational cohort study. Lancet 392:145–159. https://doi.org/10.1016/S0140-6736(18)31127-9
Andrews B, Muchemwa L, Kelly P, et al (2014) Simplified severe sepsis protocol: a randomized controlled trial of modified early goal-directed therapy in Zambia. Crit Care Med 42:2315–2324. https://doi.org/10.1097/CCM.0000000000000541
Maitland K, Kiguli S, Opoka RO, et al (2011) Mortality after fluid bolus in African children with severe infection. N Engl J Med 364:2483–2495. https://doi.org/10.1056/NEJMoa1101549
Acknowledgements
Thank you to Dr. Nishad Plakkal (Associate Professor, Neonatology, JIPMER) for reviewing our manuscript and providing invaluable insight and suggestions.
Author information
Authors and Affiliations
Contributions
Prof. S. Rao conceptualized the study and critically reviewed the manuscript for intellectual content, Dr. Britto designed the study, carried out the meta-analysis, assessment of publication bias and graphical representation of data; drafted the initial manuscript; and reviewed and revised the final manuscript, Drs. Balachander and Bosco conducted the search for articles and reviewed the manuscript. Dr Balachander was also involved in analysis and critically reviewed the manuscript for intellectual content, Dr. Mathias conducted the search for articles, designed the data collection instruments and extracted relevant data from the articles; carried out the descriptive analysis, assessment of study quality and risk of bias; drafted the initial manuscript; and reviewed and revised the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Since it is a meta-analysis, ethics approval was not sought.
Consent for participation
No human subjects were enrolled as part of the study. A meta-analysis was done.
Consent for publication
All authors have scrutinized the manuscript and consent to publish.
Conflict of interest
The authors declare no competing interests.
Table of contents summary
The role of exchange transfusion is unclear in neonatal sepsis. Based on this meta-analysis exchange transfusion is not directly recommended for neonatal sepsis given the heterogeneity and high risk of bias. Exchange transfusion may be considered on a case-basis in centres with adequate monitoring facilities.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mathias, S., Balachander, B., Bosco, A. et al. The effect of exchange transfusion on mortality in neonatal sepsis: a meta-analysis. Eur J Pediatr 181, 369–381 (2022). https://doi.org/10.1007/s00431-021-04194-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04194-w