Abstract
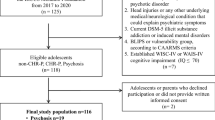
Offspring of individuals with schizophrenia (SZCOff) are at an increased risk for this disorder. Neuropsychological decline is a core feature of the disorder and researchers have reported increasing impairments in cognition during the prodromal phase in high-risk adolescents. Additionally, factors like the presence of prodromal symptoms or specific behavioral patterns could predict, together with neurocognitive functioning, the risk of conversion to severe mental disorders in SCZOff. This study aims to compare the neuropsychological functioning of a sample of 41 SCZOff children and adolescents and 105 community control offspring (CCOff) and to develop a prediction model to examine whether neuropsychological functioning, clinical and behavioral factors predict subsequent risk of severe mental disorders. We collected demographic, clinical and neuropsychological data. We found significant differences between groups in working memory, speed of processing, verbal memory and learning, visual memory and intelligence quotient (IQ). The socioeconomic status, verbal memory, working memory and positive prodromal symptoms predicted a significant proportion of the dependent variable variance. In conclusion, SCZOff showed neurocognitive impairments in several neuropsychological domains compared to CCOff. Neuropsychological functioning, environmental factors and positive prodromal symptoms could predict the risk of onset of severe mental disorders in SCZOff.
Similar content being viewed by others
References
Tsuang MT, Stone WS, Faraone SV (1999) The genetics of schizophrenia. Curr Psychiatry Rep 1(1):20–24
van Os J, Kenis G, Rutten BP (2010) The environment and schizophrenia. Nature 468(7321):203–212. https://doi.org/10.1038/nature09563
Seidman LJ, Giuliano AJ, Smith CW, Stone WS, Glatt SJ, Meyer E, Faraone SV, Tsuang MT, Cornblatt B (2006) Neuropsychological functioning in adolescents and young adults at genetic risk for schizophrenia and affective psychoses: results from the Harvard and Hillside adolescent high risk studies. Schizophr Bull 32(3):507–524. https://doi.org/10.1093/schbul/sbj078
Oner O, Munir K (2005) Attentional and neurocognitive characteristics of high-risk offspring of parents with schizophrenia compared with DSM-IV attention deficit hyperactivity disorder children. Schizophr Res 76(2–3):293–299. https://doi.org/10.1016/j.schres.2005.01.005
Andreasen NC (2000) Schizophrenia: the fundamental questions. Brain Res Brain Res Rev 31(2–3):106–112
Fuller Torrey E, Yolken RH (2000) Familial and genetic mechanisms in schizophrenia. Brain Res Brain Res Rev 31(2–3):113–117
Thorup AA, Jepsen JR, Ellersgaard DV, Burton BK, Christiani CJ, Hemager N, Skjaerbaek M, Ranning A, Spang KS, Gantriis DL, Greve AN, Zahle KK, Mors O, Plessen KJ, Nordentoft M (2015) The danish high risk and resilience study–VIA 7—a cohort study of 520 7-year-old children born of parents diagnosed with either schizophrenia, bipolar disorder or neither of these two mental disorders. BMC Psychiatry 15:233. https://doi.org/10.1186/s12888-015-0616-5
Zouraraki C, Karagiannopoulou L, Karamaouna P, Pallis EG, Giakoumaki SG (2019) Schizotypal traits, neurocognition, and paternal age in unaffected first degree relatives of patients with familial or sporadic schizophrenia. Psychiatry Res 273:422–429. https://doi.org/10.1016/j.psychres.2018.12.142
Kar SK, Jain M (2016) Current understandings about cognition and the neurobiological correlates in schizophrenia. J Neurosci Rural Pract 7(3):412–418. https://doi.org/10.4103/0976-3147.176185
Sugranyes G, de la Serna E, Romero S, Sanchez-Gistau V, Calvo A, Moreno D, Baeza I, Diaz-Caneja CM, Sanchez-Gutierrez T, Janssen J, Bargallo N, Castro-Fornieles J (2015) Gray matter volume decrease distinguishes schizophrenia from bipolar offspring during childhood and adolescence. J Am Acad Child Adolesc Psychiatry 54(8):677–684.e672. https://doi.org/10.1016/j.jaac.2015.05.003
Sugranyes G, de la Serna E, Borras R, Sanchez-Gistau V, Pariente JC, Romero S, Baeza I, Díaz-Caneja CM, Rodriguez-Toscano E, Moreno C, Bernardo M, Moreno D, Vieta E, Castro-Fornieles J (2017) Clinical, cognitive, and neuroimaging evidence of a neurodevelopmental continuum in offspring of probands with schizophrenia and bipolar disorder. Schizophr Bull 43(6):1208–1219. https://doi.org/10.1093/schbul/sbx002
Suvisaari JM, Taxell-Lassas V, Pankakoski M, Haukka JK, Lönnqvist JK, Häkkinen LT (2013) Obstetric complications as risk factors for schizophrenia spectrum psychoses in offspring of mothers with psychotic disorder. Schizophr Bull 39(5):1056–1066. https://doi.org/10.1093/schbul/sbs109
Buka SL, Seidman LJ, Tsuang MT, Goldstein JM (2013) The New England family study high-risk project: neurological impairments among offspring of parents with schizophrenia and other psychoses. Am J Med Genet B Neuropsychiatr Genet 162B(7):653–660. https://doi.org/10.1002/ajmg.b.32181
Ziermans T, de Wit S, Schothorst P, Sprong M, van Engeland H, Kahn R, Durston S (2014) Neurocognitive and clinical predictors of long-term outcome in adolescents at ultra-high risk for psychosis: a 6-year follow-up. PLoS One 9(4):e93994. https://doi.org/10.1371/journal.pone.0093994
Hameed MA, Lewis AJ (2016) Offspring of parents with schizophrenia: a systematic review of developmental features across childhood. Harv Rev Psychiatry 24(2):104–117. https://doi.org/10.1097/HRP.0000000000000076
Agerbo E, Sullivan PF, Vilhjálmsson BJ, Pedersen CB, Mors O, Børglum AD, Hougaard DM, Hollegaard MV, Meier S, Mattheisen M, Ripke S, Wray NR, Mortensen PB (2015) Polygenic risk score, parental socioeconomic status, family history of psychiatric disorders, and the risk for schizophrenia: a danish population-based study and meta-analysis. JAMA Psychiatry 72(7):635–641. https://doi.org/10.1001/jamapsychiatry.2015.0346
van Os J, Hanssen M, de Graaf R, Vollebergh W (2002) Does the urban environment independently increase the risk for both negative and positive features of psychosis? Soc Psychiatry Psychiatr Epidemiol 37(10):460–464. https://doi.org/10.1007/s00127-002-0588-x
Seidman LJ, Buka SL, Goldstein JM, Tsuang MT (2006) Intellectual decline in schizophrenia: evidence from a prospective birth cohort 28 year follow-up study. J Clin Exp Neuropsychol 28(2):225–242. https://doi.org/10.1080/13803390500360471
Arango C, Fraguas D, Parellada M (2014) Differential neurodevelopmental trajectories in patients with early-onset bipolar and schizophrenia disorders. Schizophr Bull 40(Suppl 2):S138–146. https://doi.org/10.1093/schbul/sbt198
Green MF (1996) What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 153(3):321–330. https://doi.org/10.1176/ajp.153.3.321
Nuechterlein KH, Dawson ME (1984) Information processing and attentional functioning in the developmental course of schizophrenic disorders. Schizophr Bull 10(2):160–203
Heinrichs RW, Zakzanis KK (1998) Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 12(3):426–445
Bora E, Lin A, Wood SJ, Yung AR, McGorry PD, Pantelis C (2014) Cognitive deficits in youth with familial and clinical high risk to psychosis: a systematic review and meta-analysis. Acta Psychiatrica Scand 130(1):1–15. https://doi.org/10.1111/acps.12261
Cornblatt BA, Lencz T, Smith CW, Correll CU, Auther AM, Nakayama E (2003) The schizophrenia prodrome revisited: a neurodevelopmental perspective. Schizophr Bull 29(4):633–651
McGorry PD, Yung AR, Phillips LJ (2003) The “close-in” or ultra high-risk model: a safe and effective strategy for research and clinical intervention in prepsychotic mental disorder. Schizophr Bull 29(4):771–790
Goldstein JM, Seidman LJ, Buka SL, Horton NJ, Donatelli JL, Rieder RO, Tsuang MT (2000) Impact of genetic vulnerability and hypoxia on overall intelligence by age 7 in offspring at high risk for schizophrenia compared with affective psychoses. Schizophr Bull 26(2):323–334
Giuliano AJ, Li H, Mesholam-Gately RI, Sorenson SM, Woodberry KA, Seidman LJ (2012) Neurocognition in the psychosis risk syndrome: a quantitative and qualitative review. Curr Pharm Des 18(4):399–415
Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rossler A, Schultze-Lutter F, Keshavan M, Wood S, Ruhrmann S, Seidman LJ, Valmaggia L, Cannon T, Velthorst E, De Haan L, Cornblatt B, Bonoldi I, Birchwood M, McGlashan T, Carpenter W, McGorry P, Klosterkotter J, McGuire P, Yung A (2013) The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry 70(1):107–120. https://doi.org/10.1001/jamapsychiatry.2013.269
Diwadkar VA, Montrose DM, Dworakowski D, Sweeney JA, Keshavan MS (2006) Genetically predisposed offspring with schizotypal features: an ultra high-risk group for schizophrenia? Prog Neuro-psychopharmacol Biol Psychiatry 30(2):230–238. https://doi.org/10.1016/j.pnpbp.2005.10.019
Shad MU, Tamminga CA, Cullum M, Haas GL, Keshavan MS (2006) Insight and frontal cortical function in schizophrenia: a review. Schizophr Res 86(1–3):54–70. https://doi.org/10.1016/j.schres.2006.06.006
Schreiber H, Stolz-Born G, Heinrich H, Kornhuber HH, Born J (1992) Attention, cognition, and motor perseveration in adolescents at genetic risk for schizophrenia and control subjects. Psychiatry Res 44(2):125–140
Li P, Zhang Q, Robichaud AJ, Lee T, Tomesch J, Yao W, Beard JD, Snyder GL, Zhu H, Peng Y, Hendrick JP, Vanover KE, Davis RE, Mates S, Wennogle LP (2014) Discovery of a tetracyclic quinoxaline derivative as a potent and orally active multifunctional drug candidate for the treatment of neuropsychiatric and neurological disorders. J Med Chem 57(6):2670–2682. https://doi.org/10.1021/jm401958n
Erlenmeyer-Kimling L, Rock D, Roberts SA, Janal M, Kestenbaum C, Cornblatt B, Adamo UH, Gottesman II (2000) Attention, memory, and motor skills as childhood predictors of schizophrenia-related psychoses: the New York high-risk project. Am J Psychiatry 157(9):1416–1422. https://doi.org/10.1176/appi.ajp.157.9.1416
Davalos DB, Compagnon N, Heinlein S, Ross RG (2004) Neuropsychological deficits in children associated with increased familial risk for schizophrenia. Schizophr Res 67(2–3):123–130. https://doi.org/10.1016/S0920-9964(03)00187-7
Ozan E, Deveci E, Oral M, Karahan U, Oral E, Aydin N, Kirpinar I (2010) Neurocognitive functioning in a group of offspring genetically at high-risk for schizophrenia in Eastern Turkey. Brain Res Bull 82(3–4):218–223. https://doi.org/10.1016/j.brainresbull.2010.04.013
Sugranyes G, de la Serna E, Borras R, Sanchez-Gistau V, Pariente JC, Romero S, Baeza I, Diaz-Caneja CM, Rodriguez-Toscano E, Moreno C, Bernardo M, Moreno D, Vieta E, Castro-Fornieles J (2017) Clinical, cognitive, and neuroimaging evidence of a neurodevelopmental continuum in offspring of probands with schizophrenia and bipolar disorder. Schizophr Bull. https://doi.org/10.1093/schbul/sbx002
de la Serna E, Sugranyes G, Sanchez-Gistau V, Rodriguez-Toscano E, Baeza I, Vila M, Romero S, Sanchez-Gutierrez T, Penzol MJ, Moreno D, Castro-Fornieles J (2017) Neuropsychological characteristics of child and adolescent offspring of patients with schizophrenia or bipolar disorder. Schizophr Res 183:110–115. https://doi.org/10.1016/j.schres.2016.11.007
de la Serna E, Vila M, Sanchez-Gistau V, Moreno D, Romero S, Sugranyes G, Baeza I, Llorente C, Rodriguez-Toscano E, Sanchez-Gutierrez T, Castro-Fornieles J (2016) Neuropsychological characteristics of child and adolescent offspring of patients with bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 65:54–59. https://doi.org/10.1016/j.pnpbp.2015.08.014
Sugranyes G, de la Serna E, Romero S, Sanchez-Gistau V, Calvo A, Moreno D, Baeza I, Diaz-Caneja CM, Sanchez-Gutierrez T, Janssen J, Bargallo N, Castro-Fornieles J (2015) Gray matter volume decrease distinguishes schizophrenia from bipolar offspring during childhood and adolescence. J Am Acad Child Adolesc Psychiatry 54(8):677–684. https://doi.org/10.1016/j.jaac.2015.05.003
Sanchez-Gistau V, Romero S, Moreno D, de la Serna E, Baeza I, Sugranyes G, Moreno C, Sanchez-Gutierrez T, Rodriguez-Toscano E, Castro-Fornieles J (2015) Psychiatric disorders in child and adolescent offspring of patients with schizophrenia and bipolar disorder: a controlled study. Schizophr Res 168(1–2):197–203. https://doi.org/10.1016/j.schres.2015.08.034
Hollingshead AB, Redlich FC (1958) Social class and mental illness. Wiley, New York
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36(7):980–988. https://doi.org/10.1097/00004583-199707000-00021
Ulloa RE, Ortiz S, Higuera F, Nogales I, Fresan A, Apiquian R, Cortes J, Arechavaleta B, Foulliux C, Martinez P, Hernandez L, Dominguez E, de la Pena F (2006) Interrater reliability of the Spanish version of schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL). Actas Esp Psiquiatr 34(1):36–40
Soutullo C (1999) Traducción al español de la entrevista diagnóstica: kiddie-schedule for affective disorders and schizophrenia, present and lifetime version (K-SADS-PL, 1996). http://www.cun.es/la-clinica/departamentos-yservicios-medicos/psiquiatria-y-psicologia-medica/mas-sobreel-departamento/unidades/psiquiatria-infantil-y-adolescente. Accessed May 2003
First MB, Spitzer RL, Gibbon M, Williams JB (1996) Structured clinical interview for DSM-IV axis I disorders, clinician version (SCID-CV). American Psychiatric Press Inc, Washington
Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, McFarlane W, Perkins DO, Pearlson GD, Woods SW (2003) Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull 29(4):703–715
McGlashan TH, Miller TJ, Woods SW, Hoffman RE, Davidson L (2001) A scale for the assessment of prodromal symptoms and states. In: Miller TJ, Mednick SA, McGlashan TH, Liberger J, Johannessen JO (eds) Early intervention in psychotic disorders. Kluwer Academic Publishers, Dordrecht, pp 135–149
Goodman R (1997) The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 38(5):581–586
Wechsler D (2001) Escala de inteligencia de wechsler para niños—revisada. TEA Ediciones S.A., Madrid
Reynolds CR y Bigler ED (2001) TOMAL: Test de Memoria y Aprendizaje, Madrid: TEA Ediciones
Wechsler D (1997) Wechsler Memory Scale-(WMS-III) Administration and scoring manual third, San Antonio: Psychological Corporation
Rey A (1964) L’examen clinique en psychologie (The Clinical Psychological Examination). Paris: Presse Universitaires de France
Conners CK (2000) Conners’ continuous performance test II: computer program for windows technical guide and software manual. North Tonwanda: Multi-Health Systems
Golden CJ (1978) Stroop color and word test. A manual for clinical and experimental uses. Stoelting Co, Illinois
Heaton RK, Chelune GJ, Talley JL, Kay GG, Custiss GC (2001) Test de clasificación de tarjetas de Wisconsin. TEA Ediciones S.A., Madrid
IBM Corp (2010) IBM SPSS statistics for windows, vol 19.0, 19.0th edn. IBM Corp, Armonk
Cornblatt B, Obuchowski M, Schnur DB, O’Brien JD (1997) Attention and clinical symptoms in schizophrenia. Psychiatric Q 68(4):343–359
Corcoran C, Perrin M, Harlap S, Deutsch L, Fennig S, Manor O, Nahon D, Kimhy D, Malaspina D, Susser E (2009) Effect of socioeconomic status and parents’ education at birth on risk of schizophrenia in offspring. Soc Psychiatry Psychiatr Epidemiol 44(4):265–271. https://doi.org/10.1007/s00127-008-0439-5
Kelleher I, Murtagh A, Clarke MC, Murphy J, Rawdon C, Cannon M (2013) Neurocognitive performance of a community-based sample of young people at putative ultra high risk for psychosis: support for the processing speed hypothesis. Cogn Neuropsychiatr 18(1–2):9–25. https://doi.org/10.1080/13546805.2012.682363
Carrion RE, Goldberg TE, McLaughlin D, Auther AM, Correll CU, Cornblatt BA (2011) Impact of neurocognition on social and role functioning in individuals at clinical high risk for psychosis. Am Jo Psychiatry 168(8):806–813. https://doi.org/10.1176/appi.ajp.2011.10081209
Frommann I, Pukrop R, Brinkmeyer J, Bechdolf A, Ruhrmann S, Berning J, Decker P, Riedel M, Moller HJ, Wolwer W, Gaebel W, Klosterkotter J, Maier W, Wagner M (2011) Neuropsychological profiles in different at-risk states of psychosis: executive control impairment in the early—and additional memory dysfunction in the late—prodromal state. Schizophr Bull 37(4):861–873. https://doi.org/10.1093/schbul/sbp155
Rodriguez-Sanchez JM, Crespo-Facorro B, Gonzalez-Blanch C, Perez-Iglesias R, Vazquez-Barquero JL, Study PG (2007) Cognitive dysfunction in first-episode psychosis: the processing speed hypothesis. B J Psychiatry Suppl 51:s107–110. https://doi.org/10.1192/bjp.191.51.s107
Knowles EE, David AS, Reichenberg A (2010) Processing speed deficits in schizophrenia: reexamining the evidence. Am J Psychiatry 167(7):828–835. https://doi.org/10.1176/appi.ajp.2010.09070937
Erlenmeyer-Kimling L (2000) Neurobehavioral deficits in offspring of schizophrenic parents: liability indicators and predictors of illness. Am J Med Genet 97(1):65–71
Byrne M, Hodges A, Grant E, Owens DC, Johnstone EC (1999) Neuropsychological assessment of young people at high genetic risk for developing schizophrenia compared with controls: preliminary findings of the edinburgh high risk study (EHRS). Psychol Med 29(5):1161–1173
Cornblatt B, Obuchowski M, Schnur D, O’Brien JD (1998) Hillside study of risk and early detection in schizophrenia. Br J Psychiatry Suppl 172(33):26–32
Reetzke R, Maddox WT, Chandrasekaran B (2016) The role of age and executive function in auditory category learning. J Exp Child Psychol 142:48–65. https://doi.org/10.1016/j.jecp.2015.09.018
Luna B, Garver KE, Urban TA, Lazar NA, Sweeney JA (2004) Maturation of cognitive processes from late childhood to adulthood. Child Dev 75(5):1357–1372. https://doi.org/10.1111/j.1467-8624.2004.00745.x
Medalia A, Saperstein AM, Hansen MC, Lee S (2018) Personalised treatment for cognitive dysfunction in individuals with schizophrenia spectrum disorders. Neuropsychol Rehabil 28(4):602–613. https://doi.org/10.1080/09602011.2016.1189341
Acknowledgements
We express all our thanks to the families who participated in the study. Dr. D. Moreno has been a consultant to or has received honoraria from Janssen Cilag, Shire and Rovi. Dr. Sanchez-Gutierrez has received a research grant from the Carlos III Health Institute. Dr. Sugranyes has received research grants from the Alicia Koplowitz Foundation and the Carlos III Health Institute. She has received research support from Janssen and Otsuka, educational support from Otsuka, and travel support from Adamed Pharma. Dr. Baeza has received honoraria and travel support from Otsuka and Janssen. Dr. Calvo has received a predoctoral fellowship award from Gobierno de La Rioja, a Fellowship Award for short-term placements from the Health Research Institute of Hospital Gregorio Marañon (IiSGM) and a grant for short-term placements from the Alicia Koplowitz Foundation. Dr. C. Moreno has served as a consultant to Janssen, Servier, and Lundbeck. Dr. Rodríguez-Toscano has received a research grant from the Carlos III Health Institute. Drs. Llorente, Romero, Espliego, de la Serna, Sánchez-Gistau and Castro-Fornieles have declared that they do not have conflicts of interest in relation to the subject of this study.
Funding
This work was supported by the Spanish Ministry of Economy, Industry and Competitiveness; Carlos III Health Institute [PI070066, PI1100683, PI15/00810]; and Catalonia Government [DIUE 2014SGR489]; co-financed by ERDF Funds from the European Commission, “A way of making Europe”; CIBERSAM; Madrid Regional Government [S2010/BMD-2422 AGES]; European Union Structural Funds and European Union Seventh Framework Program and H2020 Program; the Alicia Koplowitz Foundation and the Mutua Madrileña Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Sánchez-Gutiérrez, T., Rodríguez-Toscano, E., Llorente, C. et al. Neuropsychological, clinical and environmental predictors of severe mental disorders in offspring of patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci 270, 739–748 (2020). https://doi.org/10.1007/s00406-019-01044-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-019-01044-7