Abstract
Purpose
Recent study found iron consumption has been associated with an increased risk of type 2 diabetes (T2DM). Even though, high iron intake is correlated with total caloric intake, most studies have evaluated the individual effect of iron and total caloric intake. The aim of this study was to investigate the effect of iron intake, in conjunction with total energy intake, on developing T2DM. We also investigated the interactions between dietary iron and energy ratios (IERs) and iron-related single nucleotide polymorphisms (SNPs) in the development of T2DM.
Methods
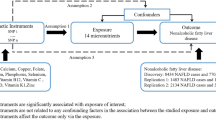
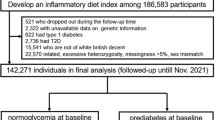
The study was carried out in Ansan and Ansung, Korea, between March 2001 and December 2014. A total of 6413 participants (3073 men and 3340 women), aged 40–69 years, were enrolled in this study. The mean follow-up period was 8.4 years. The study population was divided into quartiles based on IERs with cut-off points at 4.54, 5.41, and 6.29. The odds ratios (ORs) for new-onset T2DM were calculated across each quartile of IERs and a random forest model was constructed using the default settings to predict new-onset T2DM. To confirm the interaction among IERs, SNPs, and the incidence of T2DM, we measured the predictive power of new-onset T2DM using IER and six SNPs in genes related to iron metabolism [rs855791 (TPMRSS6), rs38116479 (TF), rs1799852 (TF), rs2280673, rs1799945 (HFT), rs180562 (HFE)].
Results
The prevalence of T2DM was 762 (11.8%). IERs showed a positive association with T2DM. The ORs were 1.30 (95% CI 1.02–1.67), 1.20 (95% CI 0.94–1.56), and 1.43 (95% CI 1.11–1.86) across the IER quartiles after adjusting for non-dietary and dietary metabolic risk factors. When the IER was 1.89-fold higher than the reference group, the risk of developing T2DM increased by 43% (OR 1.43; 95% CI 1.11–1.86).
Conclusion
A higher IER was positively associated with developing T2DM independent of dietary or non-dietary risk factors. We also found the possible interactions between the identified SNPs and iron intake in relations to T2DM.




Similar content being viewed by others
References
Lee D-H, Folsom A, Jacobs D (2004) Dietary iron intake and type 2 diabetes incidence in postmenopausal women: the Iowa Women’s Health Study. Diabetologia 47(2):185–194
Siddiqui K, Bawazeer N, Joy SS (2014) Variation in macro and trace elements in progression of type 2 diabetes. ScientificWorldJournal 2014:461591. https://doi.org/10.1155/2014/461591
Tay J, Luscombe-Marsh ND, Thompson CH, Noakes M, Buckley JD, Wittert GA, Yancy WS Jr, Brinkworth GD (2015) Comparison of low-and high-carbohydrate diets for type 2 diabetes management: a randomized trial. Am J Clin Nutr 102(4):780–790
Paolisso G, Barbagallo M (1997) Hypertension, diabetes mellitus, and insulin resistance: the role of intracellular magnesium. Am J Hypertens 10(3):346–355. https://doi.org/10.1016/s0895-7061(96)00342-1
Cefalu WT, Hu FB (2004) Role of chromium in human health and in diabetes. Diabetes Care 27(11):2741–2751. https://doi.org/10.2337/diacare.27.11.2741
Sánchez M, de la Sierra A, Coca A, Poch E, Giner V, Urbano-Márquez A (1997) Oral calcium supplementation reduces intraplatelet free calcium concentration and insulin resistance in essential hypertensive patients. Hypertension 29(1 Pt 2):531–536. https://doi.org/10.1161/01.hyp.29.1.531
Wolff SP (1993) Diabetes mellitus and free radicals. Free radicals, transition metals and oxidative stress in the aetiology of diabetes mellitus and complications. Br Med Bull 49(3):642–652. https://doi.org/10.1093/oxfordjournals.bmb.a072637
Reddy MB, Clark L (2004) Iron, oxidative stress, and disease risk. Nutr Rev 62(3):120–124. https://doi.org/10.1111/j.1753-4887.2004.tb00033.x
Piperno A, Trombini P, Gelosa M, Mauri V, Pecci V, Vergani A, Salvioni A, Mariani R, Mancia G (2002) Increased serum ferritin is common in men with essential hypertension. J Hypertens 20(8):1513–1518. https://doi.org/10.1097/00004872-200208000-00013
Ramakrishnan U, Kuklina E, Stein AD (2002) Iron stores and cardiovascular disease risk factors in women of reproductive age in the United States. Am J Clin Nutr 76(6):1256–1260. https://doi.org/10.1093/ajcn/76.6.1256
Halle M, König D, Berg A, Keul J, Baumstark MW (1997) Relationship of serum ferritin concentrations with metabolic cardiovascular risk factors in men without evidence for coronary artery disease. Atherosclerosis 128(2):235–240. https://doi.org/10.1016/s0021-9150(96)05994-1
Williams MJ, Poulton R, Williams S (2002) Relationship of serum ferritin with cardiovascular risk factors and inflammation in young men and women. Atherosclerosis 165(1):179–184. https://doi.org/10.1016/s0021-9150(02)00233-2
van Dam RM, Rimm EB, Willett WC, Stampfer MJ, Hu FB (2002) Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Ann Intern Med 136(3):201–209. https://doi.org/10.7326/0003-4819-136-3-200202050-00008
Chen Z, Watanabe RM, Stram DO, Buchanan TA, Xiang AH (2014) High calorie intake is associated with worsening insulin resistance and beta-cell function in Hispanic women after gestational diabetes mellitus. Diabetes Care 37(12):3294–3300. https://doi.org/10.2337/dc14-1433
Ali MA, Nyberg F, Chandranath SI, Ponery AS, Adem A, Adeghate E (2006) Effect of high-calorie diet on the prevalence of diabetes mellitus in the one-humped camel (Camelus dromedarius). Ann N Y Acad Sci 1084:402–410. https://doi.org/10.1196/annals.1372.034
Kim Y, Han B-G, Group K (2017) Cohort profile: the Korean genome and epidemiology study (KoGES) consortium. Int J Epidemiol 46(2):e20–e20
Ortiz-Andrellucchi A, Sánchez-Villegas A, Doreste-Alonso J, de Vries J, de Groot L, Serra-Majem L (2009) Dietary assessment methods for micronutrient intake in elderly people: a systematic review. Br J Nutr 102(S1):S118–S149
Ahn Y, Lee JE, Paik HY, Lee HK, Jo I, Kimm K (2003) Development of a semi-quantitative food frequency questionnaire based on dietary data from the Korea National Health and Nutrition Examination Survey. Nutr Sci 6(3):173–184
Hong K-W, Kim SH, Zhang X, Park S (2018) Interactions among the variants of insulin-related genes and nutrients increase the risk of type 2 diabetes. Nutr Res 51:82–92
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
American Diabetes Association (2015) (2) Classification and diagnosis of diabetes. Diabetes Care 38(Suppl):S8–S16. https://doi.org/10.2337/dc15-S005
He M, Workalemahu T, Manson JE, Hu FB, Qi L (2012) Genetic determinants for body iron store and type 2 diabetes risk in US men and women. PLoS ONE 7(7):e40919
Hong K-W, Lim J-E, Kim Y-J, Cho N-H, Shin C, Oh B-S (2010) KARE genomewide association study of blood pressure using imputed SNPs. Genom Inform 8(3):103–107
Team RC (2013) R: a language and environment for statistical computing. Austria, Vienna
van Dam RM, Willett WC, Rimm EB, Stampfer MJ, Hu FB (2002) Dietary fat and meat intake in relation to risk of type 2 diabetes in men. Diabetes Care 25(3):417–424. https://doi.org/10.2337/diacare.25.3.417
Schulze MB, Manson JE, Willett WC, Hu FB (2003) Processed meat intake and incidence of Type 2 diabetes in younger and middle-aged women. Diabetologia 46(11):1465–1473. https://doi.org/10.1007/s00125-003-1220-7
Löfvenborg JE, Ahlqvist E, Alfredsson L, Andersson T, Groop L, Tuomi T, Wolk A, Carlsson S (2020) Consumption of red meat, genetic susceptibility, and risk of LADA and type 2 diabetes. Eur J Nutr 60:769–779
Díaz-López A, Iglesias-Vázquez L, Pallejà-Millán M, Rey Reñones C, Flores Mateo G, Arija V (2020) Association between iron status and incident type 2 diabetes: a population-based cohort study. Nutrients 12(11):3249
Bertelsen M, Anggård EE, Carrier MJ (2001) Oxidative stress impairs insulin internalization in endothelial cells in vitro. Diabetologia 44(5):605–613. https://doi.org/10.1007/s001250051667
Reif DW (1992) Ferritin as a source of iron for oxidative damage. Free Radic Biol Med 12(5):417–427. https://doi.org/10.1016/0891-5849(92)90091-t
Andrews NC (1999) The iron transporter DMT1. Int J Biochem Cell Biol 31(10):991–994. https://doi.org/10.1016/s1357-2725(99)00065-5
Tiedge M, Lortz S, Drinkgern J, Lenzen S (1997) Relation between antioxidant enzyme gene expression and antioxidative defense status of insulin-producing cells. Diabetes 46(11):1733–1742. https://doi.org/10.2337/diab.46.11.1733
Fernández-Real JM, Ricart-Engel W, Arroyo E, Balançá R, Casamitjana-Abella R, Cabrero D, Fernández-Castañer M, Soler J (1998) Serum ferritin as a component of the insulin resistance syndrome. Diabetes Care 21(1):62–68. https://doi.org/10.2337/diacare.21.1.62
Riva A, Trombini P, Mariani R, Salvioni A, Coletti S, Bonfadini S, Paolini V, Pozzi M, Facchetti R, Bovo G, Piperno A (2008) Revaluation of clinical and histological criteria for diagnosis of dysmetabolic iron overload syndrome. World J Gastroenterol 14(30):4745–4752. https://doi.org/10.3748/wjg.14.4745
Trombini P, Piperno A (2007) Ferritin, metabolic syndrome and NAFLD: elective attractions and dangerous liaisons. J Hepatol 46(4):549–552. https://doi.org/10.1016/j.jhep.2007.01.004
Mendler MH, Turlin B, Moirand R, Jouanolle AM, Sapey T, Guyader D, Le Gall JY, Brissot P, David V, Deugnier Y (1999) Insulin resistance-associated hepatic iron overload. Gastroenterology 117(5):1155–1163. https://doi.org/10.1016/s0016-5085(99)70401-4
Lecube A, Hernández C, Genescà J, Simó R (2006) Glucose abnormalities in patients with hepatitis C virus infection: epidemiology and pathogenesis. Diabetes Care 29(5):1140–1149. https://doi.org/10.2337/diacare.2951140
Yokomori N, Iwasa Y, Aida K, Inoue M, Tawata M, Onaya T (1991) Transcriptional regulation of ferritin messenger ribonucleic acid levels by insulin in cultured rat glioma cells. Endocrinology 128(3):1474–1480. https://doi.org/10.1210/endo-128-3-1474
Davis RJ, Corvera S, Czech MP (1986) Insulin stimulates cellular iron uptake and causes the redistribution of intracellular transferrin receptors to the plasma membrane. J Biol Chem 261(19):8708–8711
Fernández-Real JM, López-Bermejo A, Ricart W (2002) Cross-talk between iron metabolism and diabetes. Diabetes 51(8):2348–2354. https://doi.org/10.2337/diabetes.51.8.2348
Fleming DJ, Jacques PF, Tucker KL, Massaro JM, D’Agostino RB Sr, Wilson PW, Wood RJ (2001) Iron status of the free-living, elderly Framingham Heart Study cohort: an iron-replete population with a high prevalence of elevated iron stores. Am J Clin Nutr 73(3):638–646. https://doi.org/10.1093/ajcn/73.3.638
Kang JO (2001) Chronic iron overload and toxicity: clinical chemistry perspective. Clin Lab Sci 14(3):209–219 (quiz 222)
Fleming DJ, Jacques PF, Dallal GE, Tucker KL, Wilson PW, Wood RJ (1998) Dietary determinants of iron stores in a free-living elderly population: the Framingham Heart Study. Am J Clin Nutr 67(4):722–733. https://doi.org/10.1093/ajcn/67.4.722
Lakka TA, Nyyssönen K, Salonen JT (1994) Higher levels of conditioning leisure time physical activity are associated with reduced levels of stored iron in Finnish men. Am J Epidemiol 140(2):148–160. https://doi.org/10.1093/oxfordjournals.aje.a117225
Reid JC (2015) Identification and characterization of novel proteolytic interactions of prostate cancer-expressed kallikrein-related peptidases, type II transmembrane serine proteases and matrix metalloproteinases. Queensland University of Technology
Mupfudze TG, Stoltzfus RJ, Rukobo S, Moulton LH, Humphrey JH, Prendergast AJ, Team ST (2015) Plasma concentrations of hepcidin in anemic zimbabwean infants. PLoS ONE 10(8):e0135227
Jallow MW, Cerami C, Clark TG, Prentice AM, Campino S (2020) Differences in the frequency of genetic variants associated with iron imbalance among global populations. PLoS ONE 15(7):e0235141
Benyamin B, Ferreira MA, Willemsen G, Gordon S, Middelberg RP, McEvoy BP, Hottenga J-J, Henders AK, Campbell MJ, Wallace L (2009) Common variants in TMPRSS6 are associated with iron status and erythrocyte volume. Nat Genet 41(11):1173–1175
Chambers JC, Zhang W, Li Y, Sehmi J, Wass MN, Zabaneh D, Hoggart C, Bayele H, McCarthy MI, Peltonen L (2009) Genome-wide association study identifies variants in TMPRSS6 associated with hemoglobin levels. Nat Genet 41(11):1170–1172
Gan W, Guan Y, Wu Q, An P, Zhu J, Lu L, Jing L, Yu Y, Ruan S, Xie D (2012) Association of TMPRSS6 polymorphisms with ferritin, hemoglobin, and type 2 diabetes risk in a Chinese Han population. Am J Clin Nutr 95(3):626–632
Gichohi-Wainaina WN, Melse-Boonstra A, Swinkels DW, Zimmermann MB, Feskens EJ, Towers GW (2015) Common variants and haplotypes in the TF, TNF-α, and TMPRSS6 genes are associated with iron status in a female black South African population. J Nutr 145(5):945–953
Skonieczna-Żydecka K, Jamioł-Milc D, Borecki K, Stachowska E, Zabielska P, Kamińska M, Karakiewicz B (2020) The prevalence of insomnia and the link between iron metabolism genes polymorphisms, TF rs1049296 C> T, TF rs3811647 G> A, TFR rs7385804 A> C, HAMP rs10421768 A> G and sleep disorders in polish individuals with ASD. Int J Environ Res Public Health 17(2):400
Benyamin B, McRae AF, Zhu G, Gordon S, Henders AK, Palotie A, Peltonen L, Martin NG, Montgomery GW, Whitfield JB (2009) Variants in TF and HFE explain ∼ 40% of genetic variation in serum-transferrin levels. Am J Hum Genet 84(1):60–65
Lok C, Loh T (1998) Regulation of transferrin function and expression: review and update. Neurosignals 7(3):157–178
Nielsen PB, Petersen MS, Ystaas V, Andersen RV, Hansen KM, Blaabjerg V, Refstrup M (2012) Sample-to-SNP kit: a reliable, easy and fast tool for the detection of HFE p. H63D and p. C282Y variations associated to hereditary hemochromatosis. Gene 507(1):79–84
Blanco-Rojo R, Baeza-Richer C, López-Parra AM, Pérez-Granados AM, Brichs A, Bertoncini S, Buil A, Arroyo-Pardo E, Soria JM, Vaquero MP (2011) Four variants in transferrin and HFE genes as potential markers of iron deficiency anaemia risk: an association study in menstruating women. Nutr Metab 8(1):1–8
Fernández-Real JM, Peñarroja G, Castro A, García-Bragado F, Hernández-Aguado I, Ricart W (2002) Blood letting in high-ferritin type 2 diabetes: effects on insulin sensitivity and beta-cell function. Diabetes 51(4):1000–1004. https://doi.org/10.2337/diabetes.51.4.1000
Haider LM, Schwingshackl L, Hoffmann G, Ekmekcioglu C (2018) The effect of vegetarian diets on iron status in adults: A systematic review and meta-analysis. Crit Rev Food Sci Nutr 58(8):1359–1374. https://doi.org/10.1080/10408398.2016.1259210
Hua NW, Stoohs RA, Facchini FS (2001) Low iron status and enhanced insulin sensitivity in lacto-ovo vegetarians. Br J Nutr 86(4):515–519. https://doi.org/10.1079/bjn2001421
Rockfield S, Raffel J, Mehta R, Rehman N, Nanjundan M (2017) Iron overload and altered iron metabolism in ovarian cancer. Biol Chem 398(9):995–1007. https://doi.org/10.1515/hsz-2016-0336
Lagergren K, Wahlin K, Mattsson F, Alderson D, Lagergren J (2016) Haemochromatosis and gastrointestinal cancer. Int J Cancer 139(8):1740–1743. https://doi.org/10.1002/ijc.30229
Sabatier M, Grathwohl D, Beaumont M, Groulx K, Guignard LF, Kastenmayer P, Dubascoux S, Richoz J, Habeych E, Zeder C (2020) The bioavailability of iron picolinate is comparable to iron sulfate when fortified into a complementary fruit yogurt: a stable iron isotope study in young women. Eur J Nutr 59(4):1371–1378. https://doi.org/10.1007/s00394-019-01989-4
Talaei M, Wang Y-L, Yuan J-M, Pan A, Koh W-P (2017) Meat, dietary heme iron, and risk of type 2 diabetes mellitus: the Singapore Chinese Health Study. Am J Epidemiol 186(7):824–833
Acknowledgements
Data in this study were from the Korean Genome and Epidemiology Study (KoGES; 4851-302), National Research Institute of Health, Centers for Disease Control and Prevention, Ministry for Health and Welfare, Republic of Korea. We thank all the staff working at the KoGES. There is no source of supporting to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jung, DH., Hong, K.W., Park, B. et al. Dietary iron to total energy intake ratio and type 2 diabetes incidence in a longitudinal 12-year analysis of the Korean Genome and Epidemiology Cohort Study. Eur J Nutr 60, 4453–4461 (2021). https://doi.org/10.1007/s00394-021-02596-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02596-y