Abstract
Purpose
There are epidemiologic studies indicating a positive correlation between high sodium and low potassium intake and body mass index. Therefore, this study was conducted in a cross-sectional sample of Iranian children and adolescents to evaluate the link between 24-h urinary Na:K ratio and risk of obesity.
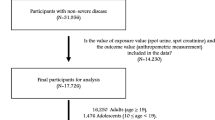
Methods
In this cross-sectional study, 374 participants aged 11–18 years were included. One 24-h urine sample was collected by each participant to estimate Na:K ratio. Anthropometric measurements were carried out and overweight/obesity was defined as a BMI ≥ 85th percentile and abdominal obesity as a waist:height ratio (WHtR) of more than 0.5.
Results
As expected, 24-h urinary Na:K ratio showed significant associations with risk of overweight/obesity. Risk of adiposity assessed by WC and PBF was significantly associated with Na:K ratio after adjusting for SSBs consumption and calorie intake. Urinary Na:K ratio showed significant association with risk of adiposity assessed by WC only in girls in the highest tertile group with OR of 2.71 (95% CI 1.14–6.43), only after the addition of calorie intake. Adiposity assessed by PBF was only associated with Na:K ratio among boys with OR of 4.47 (95% CI 1.44–9.87) and 3.87 (95% CI 1.20–8.48), after adjusting for SSBs consumption and calorie intake, respectively.
Conclusion
Our findings suggest that reducing Na and increasing K intake could be used as a useful approach to lower the risk of obesity and associated burden of disease in Iran. However, more studies are warranted.
Similar content being viewed by others
References
Djalalinia S, Kelishadi R, Qorbani M, Peykari N, Kasaeian A, Nasli-Esfahani E, Naderimagham S, Larijani B, Farzadfar F (2016) A systematic review on the prevalence of overweight and obesity, in iranian children and adolescents. Iran J Pediatr 26(3):e2599. https://doi.org/10.5812/ijp.2599
de Onis M, Blossner M, Borghi E (2010) Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr 92(5):1257–1264. https://doi.org/10.3945/ajcn.2010.29786
Delavari A, Forouzanfar MH, Alikhani S, Sharifian A, Kelishadi R (2009) First nationwide study of the prevalence of the metabolic syndrome and optimal cutoff points of waist circumference in the Middle East: the national survey of risk factors for noncommunicable diseases of Iran. Diabetes Care 32(6):1092–1097. https://doi.org/10.2337/dc08-1800
Haghdoost AA, Rezazadeh-Kermani M, Sadghirad B, Baradaran HR (2009) Prevalence of type 2 diabetes in the Islamic Republic of Iran: systematic review and meta-analysis. East Mediterr Health J 15(3):591–599
Kelishadi R, Ardalan G, Gheiratmand R, Adeli K, Delavari A, Majdzadeh R (2006) Paediatric metabolic syndrome and associated anthropometric indices: the CASPIAN Study. Acta Paediatr 95(12):1625–1634. https://doi.org/10.1080/08035250600750072
He FJ, MacGregor GA (2009) A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens 23(6):363–384
Libuda L, Kersting M, Alexy U (2012) Consumption of dietary salt measured by urinary sodium excretion and its association with body weight status in healthy children and adolescents. Public Health Nutr 15(03):433–441
El Mallah C, Merhi K, Ghattas H, Shatila D, Francis S, Hlais S, Toufeili I, Obeid O (2016) Elevated urinary Na/K ratio among Lebanese elementary school children is attributable to low K intake. Eur J Nutr. https://doi.org/10.1007/s00394-016-1164-6
Kelishadi R, Gheisari A, Zare N, Farajian S, Shariatinejad K (2013) Salt intake and the association with blood pressure in young Iranian children: first report from the middle East and north Africa. Int J Prev Med 4(4):475–483
He FJ, MacGregor GA (2007) Salt, blood pressure and cardiovascular disease. Curr Opin Cardiol 22(4):298–305
Wiseman M (2008) The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc Nutr Soc 67(03):253–256
Cappuccio FP, Kalaitzidis R, Duneclift S, Eastwood JB (2000) Unravelling the links between calcium excretion, salt intake, hypertension, kidney stones and bone metabolism. J Nephrol 13(3):169–177
Zhu H, Pollock NK, Kotak I, Gutin B, Wang X, Bhagatwala J, Parikh S, Harshfield GA, Dong Y (2014) Dietary sodium, adiposity, and inflammation in healthy adolescents. Pediatrics 133(3):e635-e642
Grimes CA, Riddell LJ, Campbell KJ, Nowson CA (2013) Dietary salt intake, sugar-sweetened beverage consumption, and obesity risk. Pediatrics 131(1):14–21
Woodruff SJ, Fryer K, Campbell T, Cole M (2014) Associations among blood pressure, salt consumption and body weight status of students from south-western Ontario. Public Health Nutr 17(05):1114–1119
Yoon Y, Oh S (2013) Sodium density and obesity; the Korea National Health and Nutrition Examination Survey 2007–2010. Eur J Clin Nutr 67(2):141–146
Rodrigues SL, Baldo MP, Machado RC, Forechi L, Molina MdCB, Mill JG (2014) High potassium intake blunts the effect of elevated sodium intake on blood pressure levels. J Am Soc Hypertens 8(4):232–238
Ge Z, Zhang J, Chen X, Yan L, Guo X, Lu Z, Xu A, Ma J (2016) Are 24 h urinary sodium excretion and sodium: potassium independently associated with obesity in Chinese adults? Public Health Nutr 19(06):1074–1080
Jain N, Minhajuddin AT, Neeland IJ, Elsayed EF, Vega GL, Hedayati SS (2014) Association of urinary sodium-to-potassium ratio with obesity in a multiethnic cohort. Am J Clin Nutr 99(5):992–998
O’Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, McQueen M, Sleight P, Sharma AM, Dans A (2011) Urinary sodium and potassium excretion and risk of cardiovascular events. Jama 306(20):2229–2238
Hedayati SS, Minhajuddin AT, Ijaz A, Moe OW, Elsayed EF, Reilly RF, Huang C-L (2012) Association of urinary sodium/potassium ratio with blood pressure: sex and racial differences. Clin J Am Soc Nephrol 7(2):315–322
Remer T, Neubert A, Maser-Gluth C (2002) Anthropometry-based reference values for 24-h urinary creatinine excretion during growth and their use in endocrine and nutritional research. Am J Clin Nutr 75(3):561–569
Cole TJ, Flegal KM, Nicholls D, Jackson AA (2007) Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 335(7612):194
Garnett S, Baur L, Cowell C (2008) Waist-to-height ratio: a simple option for determining excess central adiposity in young people. Int J Obes 32(6):1028–1030
Lee S-K, Kim MK (2016) Relationship of sodium intake with obesity among Korean children and adolescents: Korea National Health and Nutrition Examination Survey. Br J Nutr 115(05):834–841
Kelishadi R, Majdzadeh R, Motlagh M-E, Heshmat R, Aminaee T, Ardalan G, Esmaillzadeh A, Azadbakht L, Poursafa P, Movahedian M (2012) Development and evaluation of a questionnaire for assessment of determinants of weight disorders among children and adolescents: The Caspian-IV study. Int J Prev Med 3(10):699
Ghaffarpour M, Houshiar-Rad A, Kianfar H (1999) The manual for household measures, cooking yields factors and edible portion of foods. Tehran: Nashre Olume Keshavarzy 7:213
Faghihimani Z, Nourian M, Nikkar AH, Farajzadegan Z, Khavariyan N, Ghatrehsamani S, Poursafa P, Kelishadi R (2010) Validation of the child and adolescent international physical activity questionnaires in Iranian children and adolescents. ARYA Atheroscler 5 (4)
Fahimi S, Pharoah P (2012) Reducing salt intake in Iran: priorities and challenges. Arch Iran Med 15(2):110–112. http://www.sid.ir/En/Journal/ViewPaper.aspx?ID=243264
Rashidi A, Mohammadpour-Ahranjani B, Vafa M, Karandish M (2005) Prevalence of obesity in Iran. Obes Rev 6(3):191–192
Shavit L, Ferraro PM, Johri N, Robertson W, Walsh SB, Moochhala S, Unwin R (2015) Effect of being overweight on urinary metabolic risk factors for kidney stone formation. Nephrol Dial Transpl 30(4):607–613. https://doi.org/10.1093/ndt/gfu350
Taylor EN, Curhan GC (2006) Body size and 24-h urine composition. Am J Kidney Dis 48(6):905–915. https://doi.org/10.1053/j.ajkd.2006.09.004
Cai X, Li X, Fan W, Yu W, Wang S, Li Z, Scott EM, Li X (2016) Potassium and obesity/metabolic syndrome: a systematic review and meta-analysis of the epidemiological evidence. Nutrients 8(4):183
Grimes CA, Riddell LJ, Campbell KJ, He FJ, Nowson CA (2016) 24-h urinary sodium excretion is associated with obesity in a cross-sectional sample of Australian schoolchildren. Br J Nutr 115(06):1071–1079
He FJ, Marrero NM, MacGregor GA (2008) Salt intake is related to soft drink consumption in children and adolescents a link to obesity? Hypertension (Dallas, Tex: 1979) 51 (3):629–634
Fonseca-Alaniz MH, Brito LC, Borges-Silva CN, Takada J, Andreotti S, Lima FB (2007) High dietary sodium intake increases white adipose tissue mass and plasma leptin in rats. Obesity 15(9):2200–2208
Fonseca-Alaniz MH, Takada J, Andreotti S, Campos TB, Campaña AB, Borges-Silva CN, Lima FB (2008) High sodium intake enhances insulin-stimulated glucose uptake in rat epididymal adipose tissue. Obesity 16(6):1186–1192
Climent B, Simonsen U, Rivera L (2014) Effects of obesity on vascular potassium channels. Curr Vasc Pharmacol 12(3):438–452
Crunkhorn S (2013) Metabolic disease: potassium channel blocker prevents obesity. Nat Rev Drug Discov 12(8):577–577
Mariosa LSS, Ribeiro-Filho FF, Batista MC, Hirota AH, Borges RL, Ribeiro AB, Zanella MT (2008) Abdominal obesity is associated with potassium depletion and changes in glucose homeostasis during diuretic therapy. J Clin Hypertens 10(6):443–449
Yang Y, Jiang H, Wang M, Korpelainen H, Li C (2015) Male poplars have a stronger ability to balance growth and carbohydrate accumulation than do females in response to a short-term potassium deficiency. Physiol Plant 155(4):400–413
Ashcroft FM (2005) ATP-sensitive potassium channelopathies: focus on insulin secretion. J Clin Investig 115(8):2047–2058
Murakami K, Sasaki S, Uenishi K, for Nutrition JDSS., Group B (2012) The degree of misreporting of the energy-adjusted intake of protein, potassium, and sodium does not differ among under-, acceptable, and over-reporters of energy intake. Nutr Res 32(10):741–750
Acknowledgements
This study was supported by Isfahan University of Medical Sciences and Isfahan Cardiovascular Research Institute. The authors would like to thank all the schools and students/parents who agreed to participate in this study.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rafie, N., Hamedani, S.G., Mohammadifard, N. et al. 24-h urinary sodium to potassium ratio and its association with obesity in children and adolescents. Eur J Nutr 58, 947–953 (2019). https://doi.org/10.1007/s00394-018-1645-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1645-x