Abstract
This consensus statement is directed to intensivists, hematologists, and oncologists caring for critically ill cancer patients and focuses on the management of these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and background
Cancer is the second leading cause of death worldwide. According to recent publications, the incidence of neoplasms is expected to increase requiring more health care resources. Appropriate allocation of resources for cancer prevention, early diagnosis, as well as curative and palliative care remain of particular importance. This requires a detailed knowledge of the local burden of cancer [1].
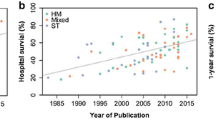
In patients with hematological or oncological malignancies, the disease itself or intensive therapy may result in critical illness in a substantial number of patients. In 1999, the American College of Critical Care Medicine stated that patients with hematological or metastasized oncological malignancies are poor candidates for ICU admission with a mortality rate of up to 90%. Thus, refusal of ICU admission of these patients was the common procedure (Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine, 1999 [2]). However, within the last 25 years, cancer and ICU treatment clearly improved. As shown in recent reports, hospital mortality decreased to less than 40% in these critically ill patients with hematologic malignancies [3]. Thus, criteria for ICU admission have to be adjusted. Aim of this consensus statement is to provide a review of the recent literature and the development of practical recommendations to hematologists, oncologists, and intensive care specialists. Due to a series of practice-changing investigations on proper ventilation techniques in cancer patients with acute respiratory failure, we put a special emphasis on discussing this topic.
Methods
The consensus group was selected to represent the expertise in the field of critical care in cancer patients in Germany and Austria. Experts were sent by the German Society of Hematology and Medical Oncology (DGHO), the Austrian Society of Hematology and Oncology (OeGHO), the German Society of Internal Intensive and Emergency Medicine (DGIIN), and the Austrian Society of Medical and General Intensive Care and Emergency Medicine (ÖGIAIN). All authors are actively supporting the “Intensive Care Medicine in Hematologic and Oncologic Patients (iCHOP)” Initiative (info@ichop.eu).
Consensus statements are based on an in-depth PubMed literature retrieval of English as well as German language literature with last access February 01, 2017. For medical heading terms (MeSH) identifying potential relevant literature, please see Appendix. Seven working groups (a: ICU transfer criteria and goals of therapy, b: respiratory failure, c: end of live decisions, d: stem cell transplant patients, e: infections, f: coagulation, and g: miscellaneous) prepared the draft proposals in a first round of consensus development. Working groups decided on references with relevant impact on guideline development, and every group member had to approve the draft guideline subchapter. Finally, the consensus statements were approved by the assembly of the members on March 2nd and 3rd 2017 in Vienna, Austria, a meeting hosted and sponsored by the OeGHO. All statements and manuscript wording underwent voting of the consensus assembly.
This guideline follows the structure and definitions of the ESCMID Guideline on Candida diseases [4,5,6]. It is in accordance with the GRADE and AGREE [7, 8] (Table 1).
All recommendations are given in boldface type.
Prognosis and ICU admission criteria
Whom to admit to the ICU/eligibility and goals of therapy
Full-code ICU management (without limitations of ICU resources) should be offered to all critically ill cancer patients if long-term survival may be compatible with the general prognosis of the underlying malignancy (A-IIu)
This statement, of course, presumes that the acute condition may be reversed by ICU measures, and that age and comorbidities of patients do not contradict such an approach. Typically, full-code management applies to patients with curative therapeutic options, those in remission of their malignancy, as well as to patients in whom cure is not likely but the expected life-span is substantial [3, 9]. It has been suggested in an earlier consensus that an assumed prognosis of 1 year may be used as cutoff for clinical decision making with regard to full-code status [10]. The authors of this manuscript believe this number is arbitrary and may be regarded as basis for individual considerations only.
Patients with poor performance status not eligible for further anti-cancer therapy, dying patients, as well as those rejecting critical care treatment should not be admitted to the ICU in general (A-III)
For patients not fulfilling the above-described criteria for full-code ICU management or ICU refusal, time-limited ICU trials or pre-defined do-not-escalate decisions (e.g., do-not-intubate or do-not-attempt-resuscitation) may be adequate options (B-IIu)
In a prospective trial on patients with intermediary prognosis (non-palliative, non-bedridden, non-full-code patients), those with worsening organ failure scores after days 5 of ICU therapy had a high risk of dying. The authors suggested to offer these patients a full-code ICU trial with re-evaluation of the goals of therapy after at least 6 days [9]. We would like to point out that almost all patients who died after day 5 had treatment-limitation decisions. Therefore, it remains unknown what their course would have been in case of further full-code management. Furthermore, data on cancer patients with poor prognosis suggest that the optimal duration of time-limited ICU trials seems to differ largely between patients with solid tumors and hematologic malignancies [11]. Thus, proposing a fixed interval from admission to re-evaluation of the goals of ICU therapy in patients undergoing time-limited ICU trials may not be generally appropriate.
When to admit to the ICU, indications and screening for organ dysfunction
Several observational investigations on cancer patients with septic complications and respiratory failure indicate that early ICU admissions and early interventions, respectively, are associated with improved survival [3, 12,13,14,15,16]. Thus, early identification of patients at risk for critical deterioration seems crucial. Severity of illness scores can only be used for describing groups of patients and should, therefore, not be used in individual clinical decision making with regard to ICU admissions or prognostication.
Cancer patients should be considered for ICU admission in case of manifest or incipient acute organ dysfunction(s) (A-IIu)
Cancer ward patients at risk should be screened for the presence of sepsis daily (A-IIt)
Cancer ward patients at risk should be screened for the presence of acute organ dysfunction(s) daily (A-IIu)
Recommendations for local structures and educational matters
Mortality of ICU cancer patients has markedly dropped over the last decades, presumably due to improved general ICU management, improved diagnostic and therapeutic strategies for several cancer-specific situations, as well as refined admission criteria [10, 17, 18]. Yet, prognostication of cancer patients and adequate patient selection remain far from perfect [19].
Centers should establish local admission criteria for critically ill cancer patients as well as standardized admission procedures, such as joint assessment by cancer specialists and intensivists, if available (A-III)
A recent Brazilian investigation showed an independent correlation between daily joint rounds of cancer specialists and intensivists as well as the number of protocols with lower mortality and more efficient resource use [20]. This is supported by Nassar and coworker stating that regular meetings may reduce possible conflicts between intensivists and oncologists [21].
Centers should establish daily joint rounds of cancer specialists and intensivists as well as standard-operating procedures for the management of frequent medical conditions of critically ill cancer patients (A-IIu)
Although a recent study by Soares and colleagues failed to identify ICU volume as a prognostic marker for ICU survival [20], the majority of available studies demonstrate a significant association of case volume and ICU mortality in cancer patients with septic shock or acute respiratory failure [22,23,24]. This effect might be linked to expertise and specific processes of care. However, some of the available observational studies may not have accounted for potential confounders related to ICU organization, structure, and process of care. Ultimately recognizing and developing “critical care of cancer patients” as a medical subspecialty may optimally serve the needs of affected patients [25]. Nevertheless, due to the fast-growing demand for critical care for cancer patients, the major practical challenge is how to provide high-quality and affordable care for all patients. Treating all critically ill cancer patients regardless of the underlying condition in specialized centers may not be feasible after all. Therefore, managing some of the rather common cancer-specific ICU problems, such as neutropenic sepsis, should become part of routine expertise for all intensive care specialists. However, in more specific situations, such as chemotherapy administration in critically ill patients with aggressive hematologic malignancies or caring for ICU patients after allogeneic stem cell transplant, transfer to specialized centers should be discussed.
Centers should establish joint continuous medical education of cancer specialists and intensivists (A-III)
Basic concepts of the care of critically ill cancer patients should be included into the curricula of both cancer specialists and intensivists (A-III)
All previous statements are summarized in Table 2.
Acute respiratory failure (ARF)
Diagnostic work-up
With respect to the critical prognosis of ARF in cancer patients, especially in patients with ARF of unknown origin [29, 30], diagnostic procedures are of major clinical importance. A systematic diagnostic work-up may lead to a (high-probability) diagnosis in approximately 70–80% of patients with ARF [31, 32]. However, diagnostic procedures should not cause a delay in the start of adequate ARF therapy including prompt antibiotic treatment (modification) in the case of a (suspected) infection (A-III).
The diagnostic strategy should encompass a comprehensive analysis of the clinical course of the underlying malignancy, including data on mechanisms of immunosuppression, antineoplastic and antimicrobial treatment, and prophylaxis [31, 33].
Independent of the clinical presentation, chest computed tomography is recommended (A-IIt)
Bronchoscopy and a BAL-based diagnostic work-up including a broad range of both culture- and non-culture-based diagnostic methods should be added to noninvasive tests depending on pretest probabilities of clinical etiologies (if clinically feasible early after ICU admission and without causing clinical worsening) (A-I)
Table 3 provides a summary of diagnostic procedures in cancer patients with ARF.
Ventilatory strategies
Noninvasive ventilation (NIV) remains the first-line standard of care in acute exacerbate chronic pulmonary disease (AECOPD) or acute cardiogenic pulmonary edema [35]. However, the role of NIV in hypoxic ARF is far less well documented. While a historic single-center randomized controlled trial (RCT) suggested superiority of NIV over conventional oxygen therapy in immunocompromised (mainly hematologic) patients with regard to intubation and survival rates [36], successive (mainly observational) studies have led to conflicting results. The 2015 “Clinical Practice Guidelines on noninvasive mechanical ventilation in ARF” on behalf of the German Society of Pneumology and Ventilatory Medicine acknowledge that NIV can be attempted to avoid intubation in immunosuppressed (including hemato-oncologic) patients. In this regard, it is of particular importance to respect common contraindications and termination, i.e., intubation criteria [35]. However, the respective guideline could not account for several meanwhile published investigations: First, a meta-analysis on 2380 mainly hematologic patients revealed that NIV as initial ventilator strategy was associated with lower mortality, whereas this finding is a mere association and cannot be interpreted as proof of principle. Importantly, 61% (range 40 to 78) of patients experienced NIV failure with secondary intubation, which itself was associated with increased mortality [37]. Second, in a large multicenter observational investigation in 1004 cancer patients with ARDS, NIV failure occurred in 71% of patients and was, again, independently associated with mortality, while mortality of ARDS patients undergoing IMV per se had decreased to 52% in recent years [38]. Finally, a recent large multicenter landmark RCT compared the use of NIV to conventional oxygen in immunocompromised (mainly hematologic) patients with hypoxic ARF (acute cardiogenic pulmonary edema or hypercapnia, i.e., PaCO2 > 50 mmHg excluded, pre-specified intubation criteria [39]). The trial did not show any clinical benefits or increased harms associated with NIV. However, the lower than expected mortality rate in the oxygen only group limited the power to detect significant differences, and a higher proportion of patients in the NIV group received high flow nasal oxygen intermittently, which may have limited the demonstrable effects of NIV. Risk factors for NIV failure in cancer patients are depicted in Table 4.
High flow nasal oxygen (HFNO) has recently been shown to be associated with reduced intubation (PaO2/FiO2 < 200) and mortality (PaO2/FiO2 < 300) rates in elderly patients with pneumonia and hypoxic ARF when compared to conventional oxygen therapy or NIV [41]. This effect was also observed in the subset of immunocompromised patients [42]. However, given conflicting data, the applicability of these findings in cancer patients, and specifically in those presenting with other etiologies than pneumonia, remains to be demonstrated [43, 44].
In case a NIV or HFNO trial is initiated in cancer patients with hypoxic ARF, common contraindications and/or the occurrence of pre-specified intubation criteria should lead to intubation and invasive mechanical ventilation without delay (A-IIu)
Given the considerable failure rates of NIV and HFNO in hypoxic ARF and the lack of sufficient data on the safety of such therapies in regular wards, NIV and HFNO should not be attempted in this indication on a regular ward (B-III)
End-of-life, palliative care
Principles in palliative care and end-of-life (EOL) management are not different in cancer patients compared to critically ill patients without a malignancy as underlying disease (A-IIt). However, (i) patient’s wish, (ii) progressive (multi-) organ failure despite full-code ICU management and no chance of reversibility, or (iii) rapid progress of cancer disease without further treatment options have to be kept in mind and could change the treatment decision or treatment goals [45]. These issues have to be discussed between oncologists and the intensive care team in an interdisciplinary manner. In cancer patients admitted to an ICU, current treatment state and estimated prognosis may be unknown to the ICU team. Therefore, consultation of an oncologist is highly recommended to provide valid prognostic information (A-III).
Intensive care admissions often represent an additional burden for patients and families in situations without option for cure. Good communication is essential to allow patients and families to meet their preferences regarding EOL. According to the literature, too many EOL decisions are made too late [46]. Early integration of an interdisciplinary palliative care team for hospitalized patients with life-limiting disease leads to fewer ICU admissions (A-I) [47]. Furthermore, integration of pro-active palliative care on ICUs, including palliative care rounds, leads to a shorter length of stay on ICU or in the hospital (A-IIt) [48, 49].
To improve quality of EOL care in critically ill patients regarding important clinical questions, i.e., preparing for withdrawal, assessment and drug management of distress, discontinuation of treatment and monitoring, or dignity conserving care [50], the authors refer to published consensus recommendations [51, 52].
Special situations
Anticancer therapy during ICU
In some cases, for example pulmonary involvement due to high grade non-Hodgkin lymphoma, hyperleukocytosis, etc., despite ICU treatment initiation or completion of anticancer chemotherapy, immunochemotherapy or radiotherapy is necessary to improve patient’s clinical situation. Such some decision needs intensive discussions between the responsible hemato-oncologist and intensivist. Again, we recommend joint assessments by cancer specialists and intensivists and that basic concepts of the care of critically ill cancer patients should be included into the curricula of both cancer specialists and intensivists.
Prevention and treatment of infections in critically ill cancer patients
Published guidelines on prevention, diagnosis, and treatment of infections in cancer patients do not specifically address critically ill cancer patients. In addition, few studies and current guidelines on infections in critically ill patients specifically address the particular requirements in the treatment of cancer patients (Table 5).
Resources on prevention and treatment of infections in cancer patients, which might be largely applicable to critically ill cancer patients, are guidelines on:
-
Management of neutropenic patients in the intensive care unit [69]
-
Prophylaxis of viral [57], bacterial [55], and fungal [56] infections including Pneumocystis jirovecii pneumonia [55]
-
Unexplained fever in neutropenic patients [60] (new version in progress)
-
Diagnosis of invasive fungal infections [70] (new version in progress)
-
Treatment of invasive fungal infections [61] and Pneumocystis jirovecii pneumonia [62]
-
Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients [63]
-
Prophylaxis and treatment of infections in recipients of autologous [71] (new version in progress) and allogeneic stem cell transplant [26]
-
Community-acquired respiratory viral infections [72]
-
Management of central venous catheter-related infections [73]
-
Gastrointestinal complications including neutropenic enterocolitis [74] (new version in progress).
-
Infections of the central nervous system in patients with hematological disorders [75]
-
The Surviving Sepsis Campaign (SSC) Guidelines for Management of Sepsis and Septic Shock recently published [76]. The guidelines published in 2014 on sepsis in neutropenic patients might be less appropriate since they are based on the 2012-ssc-guidelines [59].
-
IDSA guidelines on immunization in patients with cancer [58]; guidelines on immunization by the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO) are under progress.
-
Prophylaxis of infectious complications with colony-stimulating factors in adult cancer patients undergoing chemotherapy [68].
Allogeneic stem cell transplant setting
Criteria for ICU admission
The prognosis of allogeneic hematopoietic stem cell transplant (HSCT) patients admitted to an ICU has been significantly improved in the last years [77]. It is important to note that physicians of the primary hospital have to contact the patient’s transplant center immediately in case of critical illness. Allogeneic HSCT patients with early ICU admission or single organ dysfunction benefit from intensive care. However, patients with uncontrolled or refractory graft-versus-host disease (GvHD) should not be intubated for acute respiratory failure (A-III) [10, 78]. Thus, it is important to contact immediately patient’s transplant center.
For further information regarding isolation procedures, specific monitoring, as well as typical complications, please see supplement.
Coagulation
Venous thromboembolism (VTE), including deep-vein thrombosis and pulmonary embolism, represents a major cause of morbidity and mortality in cancer patients. An increased tumor burden results in a higher risk for VTE with the highest risk in patients receiving systemic chemotherapy or being hospitalized on surgical and medical floors.
Although there are no validated data on the risk assessment in cancer patients on the ICU, according to the American Society of Clinical Oncology guidelines, risk scores (Khorana Score, revised Khorana score, Vienna score and Protecht score) are helpful tools to identify patients at highest risk for VTE [79,80,81]. For further information on thromboprophylaxis in hospitalized patients with cancer, thromboprophylaxis in surgical patients with cancer, and treatment of thrombosis, please see Supplement Table S3 and accompanying text.
Complications after new cancer drugs or cellular immunotherapy
Pharmacological and cellular treatment of cancer is changing dramatically not only with benefits for patient’s outcome and comfort, but also with new toxicity profiles. The vast majority of adverse events can be classified as mild or moderate but there are also some cases of severe and life-threatening complications requiring ICU admission. Diagnosis and management of severe side effects after (monoclonal or bispecific) antibody treatment, tyrosine kinase inhibitors, immune checkpoint inhibitors, and chimeric antigen receptor-modified (CAR-) T cells were summarized recently in a concise review by the iCHOP group [82].
VAIA
Transfusions
In order to prevent the transfusion-associated graft versus host reaction (GvHR), all cellular blood products have to be irradiated with ≥ 30 Gy for patients with lymphatic diseases, autologous/allogeneic stem cell transplantation, and all patients treated with nucleoside analogues (fludarabine, cladribine) [83]. Generally, to prevent acute hemolysis, AB0-identic transfusions should be carried out. However, after allogeneic HSCT, in exceptional cases, it is possible to transfuse major or minor incompatible blood products according to the AB0 blood group of the patient and the donor as stated in Supplement Table S1 [84, 85]. Pooled platelet concentrates have a higher risk of immunization. Therefore, we recommend the transfusion of apheresis platelet concentrates [84].
Cytokine storm disease/Sepsis-like syndromes
Cancer patients are at risk to suffer from rare sepsis-like syndromes such as hemophagocytic lymphohistiocytosis (HLH), cytokine release syndrome (CRS), drug reaction with eosinophilia and systemic syndromes (DRESS), or capillary leak syndrome (CLS) [86,87,88,89]. Infections, malignancy itself, and drugs are major triggers for these sepsis-mimicking syndromes. Diagnostic vigilance for early recognition is essential to reduce mortality. To validate diagnosis, we recommend to include blood differential (cytopenia, eosinophilia), ferritin, soluble IL2R, fibrinogen, and triglycerides in addition to the routine ICU lab admission panel in cancer patients with sepsis or sepsis-like syndromes in whom there is no apparent focus of sepsis [90, 91] (see Table 6 for HLH diagnostic criteria). Withholding the assumed trigger drug and immediate search for an underlying malignancy or infection are pivotal. HLH patients require immediate immunosuppression with corticosteroids to prevent further progression of organ failure [92]. Early consultation with an HLH expert to stratify treatment according to the most likely trigger is recommended (www.hlh-registry.org).
Summary
During the last years, outcome of patients with malignant hematological or oncological diseases requiring intensive care treatment has clearly improved. From recently published data, we conclude that the severity of the acute illness is more important with regard to short-term survival than the underlying type and stage of malignancy. Patients receiving intensive treatment of their malignancy should be considered for ICU treatment as other severely ill patients without cancer. Centers should establish local admission criteria for critically ill cancer patients as well as standardized admission procedures, such as joint assessment by cancer specialists and intensivists, allowing identification of patients and standardized transfer to the ICU. In some patients, time-limited ICU trials with pre-defined do-not-escalate decisions (e.g., do-not-intubate or do-not-attempt-resuscitation) may be an adequate option until final decision. This implements that critically ill cancer patients should be referred to experienced intensive care units. We strongly recommend establishing a local structure with daily joint rounds of cancer specialists and intensivists as well as standard-operating procedures for the management of frequent medical conditions in critically ill cancer patients.
Furthermore, centers should organize continuous medical education of cancer specialists and intensivists. Finally, basic concepts of the care of critically ill cancer patients should be included into the curricula of both cancer specialists and intensivists.
In addition, the early integration of an interdisciplinary palliative care team is an urgently necessary measure.
In order to improve the management of critically ill cancer patients, knowledge of current practices in German-speaking countries is of utmost interest. To produce more robust data, participation of treating centers in central patient registries, e.g., the iCHOP registry (info@ichop.eu), is highly recommended.
References
Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H et al (2017) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 3(4):524–548
Medicine TFotACoCC (1999) Guidelines for intensive care unit admission, discharge, and triage. Task force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med 27(3):633–638
Azoulay E, Mokart D, Pene F, Lambert J, Kouatchet A, Mayaux J et al (2013) Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium—a groupe de recherche respiratoire en reanimation onco-hematologique study. J Clin Oncol 31(22):2810–2818
Cornely OA, Bassetti M, Calandra T, Garbino J, Kullberg BJ, Lortholary O, Meersseman W, Akova M, Arendrup MC, Arikan-Akdagli S, Bille J, Castagnola E, Cuenca-Estrella M, Donnelly JP, Groll AH, Herbrecht R, Hope WW, Jensen HE, Lass-Flörl C, Petrikkos G, Richardson MD, Roilides E, Verweij PE, Viscoli C, Ullmann AJ, ESCMID Fungal Infection Study Group (2012) ESCMID* guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect 18:19–37
Cuenca-Estrella M, Verweij PE, Arendrup MC, Arikan-Akdagli S, Bille J, Donnelly JP, Jensen HE, Lass-Flörl C, Richardson MD, Akova M, Bassetti M, Calandra T, Castagnola E, Cornely OA, Garbino J, Groll AH, Herbrecht R, Hope WW, Kullberg BJ, Lortholary O, Meersseman W, Petrikkos G, Roilides E, Viscoli C, Ullmann AJ, ESCMID Fungal Infection Study Group (2012) ESCMID* guideline for the diagnosis and management of Candida diseases 2012: diagnostic procedures. Clin Microbiol Infect 18:9–18
Ullmann AJ, Akova M, Herbrecht R, Viscoli C, Arendrup MC, Arikan-Akdagli S, Bassetti M, Bille J, Calandra T, Castagnola E, Cornely OA, Donnelly JP, Garbino J, Groll AH, Hope WW, Jensen HE, Kullberg BJ, Lass-Flörl C, Lortholary O, Meersseman W, Petrikkos G, Richardson MD, Roilides E, Verweij PE, Cuenca-Estrella M, ESCMID Fungal Infection Study Group (2012) ESCMID* guideline for the diagnosis and management of Candida diseases 2012: adults with haematological malignancies and after haematopoietic stem cell transplantation (HCT). Clin Microbiol Infect 18:53–67
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L, for the AGREE Next Steps Consortium (2010) AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ 182(18):E839–E842 xi
Brozek J, Akl E, Compalati E, Kreis J, Terracciano L, Fiocchi A et al (2011) Grading quality of evidence and strength of recommendations in clinical practice guidelines part 3 of 3. The GRADE approach to developing recommendations. Allergy 66:8
Lecuyer L, Chevret S, Thiery G, Darmon M, Schlemmer B, Azoulay E (2007) The ICU trial: a new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med 35(3):808–814
Azoulay E, Soares M, Darmon M, Benoit D, Pastores S, Afessa B (2011) Intensive care of the cancer patient: recent achievements and remaining challenges. Ann Intensive Care 1(1):5
Shrime MG, Ferket BS, Scott DJ, Lee J, Barragan-Bradford D, Pollard T, Arabi YM, al-Dorzi HM, Baron RM, Hunink MGM, Celi LA, Lai PS (2016) Time-limited trials of intensive care for critically ill patients with cancer: how long is long enough? JAMA Oncol 2(1):76–83
Gruson D, Vargas F, Hilbert G, Bui N, Maillot T, Mayet T, Pillet O, Chene G, Gbikpi-Benissan G (2004) Predictive factors of intensive care unit admission in patients with haematological malignancies and pneumonia. Intensive Care Med 30(5):965–971
Lengline E, Raffoux E, Lemiale V, Darmon M, Canet E, Boissel N et al (2012) Intensive care unit management of patients with newly diagnosed acute myeloid leukemia with no organ failure. Leuk Lymphoma 53(7):1352–1359
Hanzelka KM, Yeung SC, Chisholm G, Merriman KW, Gaeta S, Malik I et al (2013) Implementation of modified early-goal directed therapy for sepsis in the emergency center of a comprehensive cancer center. Support Care Cancer 21(3):727–734
Mokart D, Lambert J, Schnell D, Fouche L, Rabbat A, Kouatchet A et al (2013) Delayed intensive care unit admission is associated with increased mortality in patients with cancer with acute respiratory failure. Leuk Lymphoma 54(8):1724–1729
Song JU, Suh GY, Park HY, Lim SY, Han SG, Kang YR, Kwon OJ, Woo S, Jeon K (2012) Early intervention on the outcomes in critically ill cancer patients admitted to intensive care units. Intensive Care Med 38(9):1505–1513
Azoulay E, Pene F, Darmon M, Lengline E, Benoit D, Soares M, et al (2015) Managing critically Ill hematology patients: time to think differently. Blood Rev 29(6):359–367
Schellongowski P, Sperr WR, Wohlfarth P, Knoebl P, Rabitsch W, Watzke HH, Staudinger T (2016) Critically ill patients with cancer: chances and limitations of intensive care medicine-a narrative review. ESMO Open 1(5):e000018
Thiery G, Azoulay E, Darmon M, Ciroldi M, De Miranda S, Levy V et al (2005) Outcome of cancer patients considered for intensive care unit admission: a hospital-wide prospective study. J Clin Oncol 23(19):4406–4413
Soares M, Bozza FA, Azevedo LC, Silva UV, Correa TD, Colombari F et al (2016) Effects of organizational characteristics on outcomes and resource use in patients with cancer admitted to intensive care units. J Clin Oncol 34(27):3315–3324
Nassar AP, Jr., Dettino ALA, Amendola CP, Dos Santos RA, Forte DN, Caruso P (2017) Oncologists’ and intensivists’ attitudes toward the care of critically Ill patients with cancer. J Intensive Care Med. https://doi.org/10.1177/0885066617716105
Lecuyer L, Chevret S, Guidet B, Aegerter P, Martel P, Schlemmer B, Azoulay E (2008) Case volume and mortality in haematological patients with acute respiratory failure. Eur Respir J 32(3):748–754
Soares M, Toffart AC, Timsit JF, Burghi G, Irrazabal C, Pattison N et al (2014) Intensive care in patients with lung cancer: a multinational study. Ann Oncol 25(9):1829–1835
Zuber B, Tran TC, Aegerter P, Grimaldi D, Charpentier J, Guidet B, Mira JP, Pène F, CUB-Réa Network (2012) Impact of case volume on survival of septic shock in patients with malignancies. Crit Care Med 40(1):55–62
Bergwelt-Baildon M, Hallek MJ, Shimabukuro-Vornhagen AA, Kochanek M (2010) CCC meets ICU: redefining the role of critical care of cancer patients. BMC Cancer 10:5
Ullmann AJ, Schmidt-Hieber M, Bertz H, Heinz WJ, Kiehl M, Kruger W et al (2016) Infectious diseases in allogeneic haematopoietic stem cell transplantation: prevention and prophylaxis strategy guidelines 2016. Ann Hematol 95(9):1435–1455
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8):801–810
Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS et al (2016) Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8):775–787
Azoulay E, Thiéry G, Chevret S, Moreau D, Darmon M, Bergeron A, Yang K, Meignin V, Ciroldi M, Le Gall JR, Tazi A, Schlemmer B (2004) The prognosis of acute respiratory failure in critically ill cancer patients. Medicine (Baltimore) 83(6):11
Contejean A, Lemiale V, Resche-Rigon M, Mokart D, Pene F, Kouatchet A et al (2016) Increased mortality in hematological malignancy patients with acute respiratory failure from undetermined etiology: a Groupe de Recherche en Reanimation Respiratoire en Onco-Hematologique (Grrr-OH) study. Ann Intensive Care 6(1):102
Azoulay E, Mokart D, Lambert J, Lemiale V, Rabbat A, Kouatchet A, Vincent F, Gruson D, Bruneel F, Epinette-Branche G, Lafabrie A, Hamidfar-Roy R, Cracco C, Renard B, Tonnelier JM, Blot F, Chevret S, Schlemmer B (2010) Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med 182(8):1038–1046
Zompatori M, Ciccarese F, Fasano L (2014) Overview of current lung imaging in acute respiratory distress syndrome. Eur Respir Rev 23(134):519–530
Schnell D, Mayaux J, Lambert J, Roux A, Moreau AS, Zafrani L, Canet E, Lemiale V, Darmon M, Azoulay É (2013) Clinical assessment for identifying causes of acute respiratory failure in cancer patients. Eur Respir J 42(2):435–443
Alanio A, Hauser PM, Lagrou K, Melchers WJ, Helweg-Larsen J, Matos O et al (2016) ECIL guidelines for the diagnosis of Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J Antimicrob Chemother 71(9):2386–2396
Westhoff M (2013) Implementation of the German S3-guideline of non-invasive ventilation for acute respiratory failure in daily practice. Dtsch Med Wochenschr 138(16):825–830
Hilbert G, Ruson D, Vargas F, Valention R, Gbikpi-Benissan G, Dupon M et al (2001) Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med 344:7
Amado-Rodriguez L, Bernal T, Lopez-Alonso I, Blazquez-Prieto J, Garcia-Prieto E, Albaiceta GM (2016) Impact of initial ventilatory strategy in hematological patients with acute respiratory failure: a systematic review and meta-analysis. Crit Care Med 44(7):1406–1413
Neuschwander A, Lemiale V, Darmon M, Pene F, Kouatchet A, Perez P et al (2017) Noninvasive ventilation during acute respiratory distress syndrome in patients with cancer: trends in use and outcome. J Crit Care 38:295–299
Lemiale V, Mokart D, Resche-Rigon M, Pene F, Mayaux J, Faucher E, et al. (2015) Effect of noninvasive ventilation vs oxygen therapy on mortality among immunocompromised patients with acute respiratory failure: a randomized clinical trial. JAMA. :1–9
Soares M, Depuydt PO, Salluh JI (2010) Mechanical ventilation in cancer patients: clinical characteristics and outcomes. Crit Care Clin 26(1):41–58
Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira JP, Argaud L, Chakarian JC, Ricard JD, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin JM, Tonnelier JM, Pierrot M, Mathonnet A, Béduneau G, Delétage-Métreau C, Richard JC, Brochard L, Robert R, FLORALI Study Group, REVA Network (2015) High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 372(23):2185–2196
Frat JP, Ragot S, Girault C, Perbet S, Prat G, Boulain T, Demoule A, Ricard JD, Coudroy R, Robert R, Mercat A, Brochard L, Thille AW (2016) Effect of non-invasive oxygenation strategies in immunocompromised patients with severe acute respiratory failure: a post-hoc analysis of a randomised trial. Lancet Respir Med 4 (8): 646–652
Lemiale V, Resche-Rigon M, Mokart D, Pene F, Argaud L, Mayaux J et al (2017) High-flow nasal cannula oxygenation in immunocompromised patients with acute hypoxemic respiratory failure: a Groupe de Recherche Respiratoire en Reanimation Onco-Hematologique study. Crit Care Med 45(3):e274–ee80
Schellongowski P, Staudinger T (2016) Ventilatory strategies in patients with hematologic malignancies and acute respiratory failure: new insights, new questions, what now? Crit Care Med 44(7):1444–1446
Sprung CL, Cohen SL, Sjokvist P, Bulow HH, Hovilehto S, Ledoux D, Lippert A, Maia P, Phelan D, Schobersberger W, Wennberg E, Woodcock T (2003) End-of-life practices in European intensive care units. JAMA 290(6):8
Rady MY, Johnson DJ (2004) Admission to intensive care unit at the end-of-life: is it an informed decision? Palliat Med 18(8):705–711
Gade G, Venohr I, Conner D, McGrady K, Beane J, Richardson RH, Williams MP, Liberson M, Blum M, Penna RD (2008) Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med 11(2):180–190
Norton SA, Hogan LA, Holloway RG, Temkin-Greener H, Buckley MJ, Quill TE (2007) Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med 35(6):1530–1535
Braus N, Campbell TC, Kwekkeboom KL, Ferguson S, Harvey C, Krupp AE, Lohmeier T, Repplinger MD, Westergaard RP, Jacobs EA, Roberts KF, Ehlenbach WJ (2016) Prospective study of a proactive palliative care rounding intervention in a medical ICU. Intensive Care Med 42(1):54–62
Cook D, Rocker G (2014) Dying with dignity in the intensive care unit. N Engl J Med 370(26):2506–2514
Downar J, Delaney JW, Hawryluck L, Kenny L (2016) Guidelines for the withdrawal of life-sustaining measures. Intensive Care Med 42(6):1003–1017
Deutsche Krebsgesellschaft DK, AWMF (2015) Palliativmedizin für Patienten mit einer nicht heilbaren Krebserkrankung
Parmar A, Richardson H, McKinlay D, Gibney RT, Bagshaw SM (2013) Medical emergency team involvement in patients hospitalized with acute myeloid leukemia. Leuk Lymphoma 54(10):2236–2242
Rieg S, Kupper MF (2016) Infectious diseases consultations can make the difference: a brief review and a plea for more infectious diseases specialists in Germany. Infection 44(2):159–166
Neumann S, Krause SW, Maschmeyer G, Schiel X, von Lilienfeld-Toal M, Infectious diseases working P et al (2013) Primary prophylaxis of bacterial infections and Pneumocystis jirovecii pneumonia in patients with hematological malignancies and solid tumors : guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 92(4):433–442
Tacke D, Buchheidt D, Karthaus M, Krause SW, Maschmeyer G, Neumann S, Ostermann H, Penack O, Rieger C, Ruhnke M, Sandherr M, Schweer KE, Ullmann AJ, Cornely OA (2014) Primary prophylaxis of invasive fungal infections in patients with haematologic malignancies. 2014 update of the recommendations of the Infectious Diseases Working Party of the German Society for Haematology and Oncology. Ann Hematol 93(9):1449–1456
Sandherr M, Hentrich M, von Lilienfeld-Toal M, Massenkeil G, Neumann S, Penack O, Biehl L, Cornely OA (2015) Antiviral prophylaxis in patients with solid tumours and haematological malignancies—update of the Guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Medical Oncology (DGHO). Ann Hematol 94(9):1441–1450
Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M, Bousvaros A, Dhanireddy S, Sung L, Keyserling H, Kang I, Infectious Diseases Society of America (2014) 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin Infect Dis 58(3):309–318
Penack O, Becker C, Buchheidt D, Christopeit M, Kiehl M, von Lilienfeld-Toal M, Hentrich M, Reinwald M, Salwender H, Schalk E, Schmidt-Hieber M, Weber T, Ostermann H (2014) Management of sepsis in neutropenic patients: 2014 updated guidelines from the Infectious Diseases Working Party of the German Society of Hematology and Medical Oncology (AGIHO). Ann Hematol 93(7):1083–1095
Link H, Bohme A, Cornely OA, Hoffken K, Kellner O, Kern WV et al (2003) Antimicrobial therapy of unexplained fever in neutropenic patients—guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO), study group interventional therapy of unexplained fever, Arbeitsgemeinschaft Supportivmassnahmen in der Onkologie (ASO) of the Deutsche Krebsgesellschaft (DKG-German Cancer Society). Ann Hematol 82(Suppl 2):S105–S117
Mousset S, Buchheidt D, Heinz W, Ruhnke M, Cornely OA, Egerer G, Krüger W, Link H, Neumann S, Ostermann H, Panse J, Penack O, Rieger C, Schmidt-Hieber M, Silling G, Südhoff T, Ullmann AJ, Wolf HH, Maschmeyer G, Böhme A (2014) Treatment of invasive fungal infections in cancer patients-updated recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 93(1):13–32
Maschmeyer G, Helweg-Larsen J, Pagano L, Robin C, Cordonnier C, Schellongowski P, 6th European Conference on Infections in Leukemia (ECIL-6), a joint venture of The European Group for Blood and Marrow Transplantation (EBMT), The European Organization for Research and Treatment of Cancer (EORTC), the International Immunocompromised Host Society (ICHS) and The European LeukemiaNet (ELN) (2016) ECIL guidelines for treatment of Pneumocystis jirovecii pneumonia in non-HIV-infected haematology patients. J Antimicrob Chemother 71(9):2405–2413
Maschmeyer G, Carratala J, Buchheidt D, Hamprecht A, Heussel CP, Kahl C et al (2015) Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients (allogeneic SCT excluded): updated guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Ann Oncol 26(1):21–33
Bertz H, Auner HW, Weissinger F, Salwender HJ, Einsele H, Egerer G et al (2003) Antimicrobial therapy of febrile complications after high-dose chemo-/radiotherapy and autologous hematopoietic stem cell transplantation--guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 82(Suppl 2):S167–S174
Azoulay E, Attalah H, Harf A, Schlemmer B, Delclaux C (2001) Granulocyte colony-stimulating factor or neutrophil-induced pulmonary toxicity: myth or reality? Systematic review of clinical case reports and experimental data. Chest 120(5):1695–1701
Verhoef G, Boogaerts M (1991) Treatment with granulocyte-macrophage colony stimulating factor and the adult respiratory distress syndrome. Am J Hematol 36(4):285–287
Karlin L, Darmon M, Thiery G, Ciroldi M, de Miranda S, Lefebvre A et al (2005) Respiratory status deterioration during G-CSF-induced neutropenia recovery. Bone Marrow Transplant 36(3):245–250
Vehreschild JJ, Bohme A, Cornely OA, Kahl C, Karthaus M, Kreuzer KA et al (2014) Prophylaxis of infectious complications with colony-stimulating factors in adult cancer patients undergoing chemotherapy-evidence-based guidelines from the Infectious Diseases Working Party AGIHO of the German Society for Haematology and Medical Oncology (DGHO). Ann Oncol 25(9):1709–1718
Schnell D, Azoulay E, Benoit D, Clouzeau B, Demaret P, Ducassou S, Frange P, Lafaurie M, Legrand M, Meert AP, Mokart D, Naudin J, Pene F, Rabbat A, Raffoux E, Ribaud P, Richard JC, Vincent F, Zahar JR, Darmon M (2016) Management of neutropenic patients in the intensive care unit (NEWBORNS EXCLUDED) recommendations from an expert panel from the French Intensive Care Society (SRLF) with the French Group for Pediatric Intensive Care Emergencies (GFRUP), the French Society of Anesthesia and Intensive Care (SFAR), the French Society of Hematology (SFH), the French Society for Hospital Hygiene (SF2H), and the French Infectious Diseases Society (SPILF). Ann Intensive Care 6(1):90
Ruhnke M, Bohme A, Buchheidt D, Cornely O, Donhuijsen K, Einsele H et al (2012) Diagnosis of invasive fungal infections in hematology and oncology—guidelines from the Infectious Diseases Working Party in haematology and oncology of the German Society for Haematology and Oncology (AGIHO). Ann Oncol 23(4):823–833
Weissinger F, Auner HW, Bertz H, Buchheidt D, Cornely OA, Egerer G, Heinz W, Karthaus M, Kiehl M, Krüger W, Penack O, Reuter S, Ruhnke M, Sandherr M, Salwender HJ, Ullmann AJ, Waldschmidt DT, Wolf HH (2012) Antimicrobial therapy of febrile complications after high-dose chemotherapy and autologous hematopoietic stem cell transplantation—guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 91(8):1161–1174
von Lilienfeld-Toal M, Berger A, Christopeit M, Hentrich M, Heussel CP, Kalkreuth J, Klein M, Kochanek M, Penack O, Hauf E, Rieger C, Silling G, Vehreschild M, Weber T, Wolf HH, Lehners N, Schalk E, Mayer K (2016) Community acquired respiratory virus infections in cancer patients—guideline on diagnosis and management by the Infectious Diseases Working Party of the German Society for Haematology and Medical Oncology. Eur J Cancer 67:200–212
Hentrich M, Schalk E, Schmidt-Hieber M, Chaberny I, Mousset S, Buchheidt D, Ruhnke M, Penack O, Salwender H, Wolf HH, Christopeit M, Neumann S, Maschmeyer G, Karthaus M, Infectious Diseases Working Party of the German Society of Hematology and Medical Oncology (2014) Central venous catheter-related infections in hematology and oncology: 2012 updated guidelines on diagnosis, management and prevention by the Infectious Diseases Working Party of the German Society of Hematology And Medical Oncology. Ann Oncol 25(5):936–947
Vehreschild MJ, Vehreschild JJ, Hubel K, Hentrich M, Schmidt-Hieber M, Christopeit M et al (2013) Diagnosis and management of gastrointestinal complications in adult cancer patients: evidence-based guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Oncol 24(5):1189–1202
Schmidt-Hieber M, Silling G, Schalk E, Heinz W, Panse J, Penack O, Christopeit M, Buchheidt D, Meyding-Lamadé U, Hähnel S, Wolf HH, Ruhnke M, Schwartz S, Maschmeyer G (2016) CNS infections in patients with hematological disorders (including allogeneic stem-cell transplantation)-guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Ann Oncol 27(7):1207–1225
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, de Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med 45(3):486–552
Lengline E, Chevret S, Moreau AS, Pene F, Blot F, Bourhis JH et al (2015) Changes in intensive care for allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant 50(6):840–845
Saillard C, Blaise D, Mokart D (2016) Critically ill allogeneic hematopoietic stem cell transplantation patients in the intensive care unit: reappraisal of actual prognosis. Bone Marrow Transplant 51(8):1050–1061
Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW (2008) Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111(10):4902–4907
Khorana AA, McCrae KR (2014) Risk stratification strategies for cancer-associated thrombosis: an update. Thromb Res 133(Suppl 2):S35–S38
Verso M, Agnelli G, Barni S, Gasparini G, LaBianca R (2012) A modified Khorana risk assessment score for venous thromboembolism in cancer patients receiving chemotherapy: the Protecht score. Intern Emerg Med 7(3):291–292
Kroschinsky F, Stolzel F, von Bonin S, Beutel G, Kochanek M, Kiehl M et al (2017) New drugs, new toxicities: severe side effects of modern targeted and immunotherapy of cancer and their management. Crit Care 21(1):89
Moroff G, Luban NL (1997) The irradiation of blood and blood components to prevent graft-versus-host disease: technical issues and guidelines. Transfus Med Rev 11(1):15–26
Bundesärztekammer WBd (2014) Querschnitts-Leitlinien zur Therapie mit Blutkomponenten und Plasmaderivaten
Cassens U, Eichler H, Klüter H, Kroll H, Schlenke P, Wiesneth M (2004) Stellungnahme der Sektion “Transplantation und Zelltherapie” zur Transplantation hämatopoetischer Stammzellen mit Blutgruppendifferenz. Transfus Med Hemother 31:5
Lachmann G, La Rosee P, Schenk T, Brunkhorst FM, Spies C (2016) Hemophagocytic lymphohistiocytosis : a diagnostic challenge on the ICU. Anaesthesist 65(10):776–786
Schnetzke U, Bossert T, Scholl S, Freesmeyer M, Hochhaus A, La Rosee P (2011) Drug-induced lymphadenopathy with eosinophilia and renal failure mimicking lymphoma disease: dramatic onset of DRESS syndrome associated with antibiotic treatment. Ann Hematol 90(11):1353–1355
Deeren DH, Zachee P, Malbrain ML (2005) Granulocyte colony-stimulating factor-induced capillary leak syndrome confirmed by extravascular lung water measurements. Ann Hematol 84(2):89–94
Frey NV, Porter DL (2016) Cytokine release syndrome with novel therapeutics for acute lymphoblastic leukemia. Hematology Am Soc Hematol Educ Program 2016(1):567–572
Lehmberg K, Nichols KE, Henter JI, Girschikofsky M, Greenwood T, Jordan M, Kumar A, Minkov M, la Rosée P, Weitzman S, Study Group on Hemophagocytic Lymphohistiocytosis Subtypes of the Histiocyte Society (2015) Consensus recommendations for the diagnosis and management of hemophagocytic lymphohistiocytosis associated with malignancies. Haematologica 100(8):997–1004
La Rosée PS, Kunert C, Hochhaus A (2013) Die hämophagozytische Lymphohistiozytose (HLH) und das Makrophagenaktivierungssyndrom (MAS): Klinisches ERscheinungsbild und Diagnostik. Laboratoriumsmedizin 37(5):217–225
La Rosee P (2015) Treatment of hemophagocytic lymphohistiocytosis in adults. Hematology Am Soc Hematol Educ Program 2015(1):190–196
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kiehl, M.G., Beutel, G., Böll, B. et al. Consensus statement for cancer patients requiring intensive care support. Ann Hematol 97, 1271–1282 (2018). https://doi.org/10.1007/s00277-018-3312-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-018-3312-y