Abstract
Background
Defining severe postoperative ileus in terms of consequences could help physicians standardize the management of this condition. The recently described classification based on consequences requires further investigation. The aim of this study was to obtain a snapshot of postoperative ileus in patients undergoing colorectal surgery within enhanced recovery programs and to identify factors associated with non-severe and severe postoperative ileus.
Methods
This prospective registry data analysis was conducted in 40 centers in five different countries. A total of 786 patients scheduled for colorectal surgery within enhanced recovery programs were included. The primary endpoint was the incidence rate of postoperative ileus as defined by Vather et al.
Results
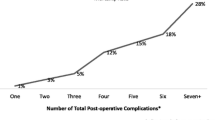
A total of 121 patients experienced postoperative ileus (15.4%). Non-severe POI occurred in 48 patients (6.1%), and severe postoperative ileus occurred in 73 patients (9.3%). In multivariate analysis, the male gender and intra-abdominal complications were associated with severe postoperative ileus: odd ratio (OR) = 2.03 [95% confidence interval (CI) 1.14–3.59], p = 0.01 and OR = 3.60 [95% CI 1.75–7.40], p < 0.0001, respectively. Conversely, open laparotomy and urinary retention were associated with non-severe POI: OR = 3.03 [95% CI 1.37–6.72], p = 0.006 and OR = 2.70 [95% CI 0.89–8.23], p = 0.08, respectively.
Conclusions
Postoperative ileus occurred in 15% of patients after colorectal surgery within enhanced recovery programs. For 60% of patients, this was considered severe. The physiopathology of these two entities could be different, severe POI being linked to intraabdominal complication, while non-severe POI being linked with risk factors for “primary” POI. The physician should pay attention to male patients having POI after colorectal surgery and look for features evocating intraabdominal complications.

Similar content being viewed by others
Change history
28 January 2020
In the list of participating investigators that appears in Acknowledgements, one of the investigators names appears incorrectly.
References
Venara A, Slim K, Regimbeau J-M et al (2017) Proposal of a new classification of postoperative ileus based on its clinical impact-results of a global survey and preliminary evaluation in colorectal surgery. Int J Colorectal Dis 32:797–803
Asgeirsson T, El-Badawi KI, Mahmood A, Barletta J, Luchtefeld SA (2010) Postoperative ileus: it costs more than you expect. J Am Coll Surg 210:228–231
Barbieux J, Hamy A, Talbot MF et al (2017) Does enhanced recovery reduce postoperative ileus after colorectal surgery? J Visc Surg 154:79–85
Grass F, Slieker J, Jurt J, Kummer A et al (2017) Postoperative ileus in an enhanced recovery pathway—a retrospective cohort study. Int J Colorectal Dis 32:675–681
Gignoux B, Gosgnach M, Lanz T et al (2018) Short-term outcomes of ambulatory colectomy for 157 consecutive patients. Ann Surg (in press)
Venara A, Alfonsi P, Cotte E, Loria J, Hamel JF, Slim K, Francophone Group for enhanced recovery after surgery (2018) Postoperative ileus concealing intra-abdominal complications in enhanced recovery programs-a retrospective analysis of the GRACE database. Int J Colorectal Dis 34:71–83
Courtot L, Le Roy B, Memeo R et al (2018) Risk factors for postoperative ileus following elective laparoscopic right colectomy: a retrospective multicentric study. Int J Colorectal Dis 33:1373–1382
Yorkshire Surgical Research Collaborative (2018) Multicentre observational study of gastrointestinal recovery after elective colorectal surgery. Colorectal Dis 20:536–544
Vather R, Trivedi S, Bissett I (2013) Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg 17:962–972
Wolthuis AM, Bislenghi G, Fieuws S et al (2016) Incidence of prolonged postoperative ileus after colorectal surgery: a systematic review and meta-analysis. Colorectal Dis 18:O1–O9
Vather R, Josephson R, Jaung R, Robertson J, Bissett I (2015) Development of a risk stratification system for the occurrence of prolonged postoperative ileus after colorectal surgery: a prospective risk factor analysis. Surgery 157:764–773
Ceretti AP, Maroni N, Longhi M et al (2018) Risk factors for prolonged postoperative Ileus in adult patients undergoing elective colorectal surgery: an observational cohort study. Rev Recent Clin Trials 13:295–304
Wolthuis AM, Bislenghi G, Lambrecht M et al (2017) Preoperative risk factors for prolonged postoperative ileus after colorectal resection. Int J Colorectal Dis 32:883–890
Mariette C, Alves A, Benoist S, Bretagnol F, Mabrut JY, Slim K (2015) Perioperative care in digestive surgery. Guidelines for the French society of digestive surgery (SFCD). Ann Chir 130:108–124
Venara A, Neunlist M, Slim K, Barbieux J, Colas PA, Hamy A, Meurette G (2016) Postoperative ileus: pathophysiology, incidence, and prevention. J Visc Surg 153:439–446
Millan M, Biondo S, Fraccalvieri D, Frago R, Golda T, Kreisler E (2012) Risk factors for prolonged postoperative ileus after colorectal cancer surgery. World J Surg 36:179–185. https://doi.org/10.1007/s00268-011-1339-5
Rybakov EG, Shelygin YA, Khomyakov EA, Zarodniuk IV (2017) Risk factors for postoperative ileus after colorectal cancer surgery. Colorectal Dis (in press)
Kalff JC, Schraut WH, Simmons RL, Bauer AJ (1998) Surgical manipulation of the gut elicits an intestinal muscularis inflammatory response resulting in postsurgical ileus. Ann Surg 228:652–663
Uemura K, Tatewaki M, Harris MB et al (2004) Magnitude of abdominal incision affects the duration of postoperative ileus in rats. Surg Endosc 18:606–610
Gervaz P, Inan I, Perneger T, Schiffer E, Morel P (2010) A prospective, randomized, single-blind comparison of laparoscopic versus open sigmoid colectomy for diverticulitis. Ann Surg 252:3–8
The FO, Bennink RJ, Ankum WM et al (2008) Intestinal handling-induced mast cell activation and inflammation in human postoperative ileus. Gut 57:33–40
Cali RL, Meade PG, Swanson MS, Freeman C (2000) Effect of Morphine and incision length on bowel function after colectomy. Dis Colon Rectum 43:163–168
Kaufman PN, Krevsky B, Malmud LS, Maurer AH, Chase BJ, Fisher RS (1998) Role of opiate receptors in the regulation of colonic transit. Gastroenterology 94:1351–1356
Chen JY, Ko TL, Wen YR, Wu SC, Chou YH, Yien HW, Kuo CD (2009) Opioid-sparing effects of ketorolac and its correlation with the recovery of postoperative bowel function in colorectal surgery patients: a prospective randomized double-blinded study. Clin J Pain 25:485–489
Elsamra SE, Ellsworth P (2012) Effects of analgesic and anesthetic medications on lower urinary tract function. Urol Nurs 32:60–67
Grass F, Slieker J, Frauche P et al (2017) Postoperative urinary retention in colorectal surgery within an enhanced recovery pathway. J Surg Res 207:70–76
Peters EG, Dekkers M, van Leeuwen-Hilbers FW et al (2017) Relation between postoperative ileus and anastomotic leakage after colorectal resection: a post hoc analysis of a prospective randomized controlled trial. Colorectal Dis 19:667–674
Zhuang CL, Chen FF, Lu JX et al (2015) Impact of different surgical traumas on postoperative ileus in rats and the mechanism involved. Int J Clin Exp Med 15:16778–16786
Acknowledgements
GRACE Collaborative Group for Ileus Study/Participating Investigators who provided care for study patients: CHAPUIS O, GUIGNARD B (Clinique du Val d’Or, Saint Cloud, France), GERMAIN A (Nancy, France), SAINT DENIS M, SIRIEIX D (Hôpital privé d’Antony, Antony, France), ARIMONT JM, FIGUET S (CH-Alpes Leman, Contamine sur Arve, France), MILOU F (HIA Desgenettes, Lyon, France), HAIL K (Clinique Chirurgicale B, CHU Mustapha, Alger, Algérie), K OTHONIDIS K (App Sambre et Meuse/CHR Val de Sambre, Sambreville, France), FAUCHERON JL, SAGE PY (CHU Grenoble Alpes, La Tronche, France), MAUVAIS F (CH Beauvais, Beauvais, France), RIO D (CH Bretagne Atlantique, Vannes, France), GUIOT JL (Pole Santé du Plateau, Meudon La Forêt, France), POINCENOT J (CHIC, Créteil, France), CUELLAR E (CHU Toulouse, Toulouse, France), LUYER M, BOUDEWIJN S (Catharina Hospital, Eindhoven, The Netherlands), AUMONT O, DUPRE A, POIBLANC M, SENS N (Centre Leon Berard, Lyon, France), BRIGAND C, STEINMETZ JP (Hôpital de Hautepierre, Strasbourg, France), PLUMEREAU F (CH Laval, France), MATHONNET M, CHRISTOU N (CHRU Limoges, Limoges, France), ORTEGA-DEBALLON P, VAUCLAIR E (CHU Dijon, Dijon, France), BOZIO G (Médipole de Savoie, Challes Les Eaux, France), FERNOUX P, MASSARD JL (Hôpital Privé Sainte Marie, Chalon sur Saone, France), BELLOUARD A, de la FONTAINE C, FINIANOS A, MICHAUD P (Clinique de l’Archette, Olivet, France), BOSSARD AE, DENET C, GRIGORIU M, KATTOU F (Institut Mutualiste Montsouris, Paris, France), GIGNOUX B, VERRIER JF (Clinique de la Sauvegarde, Lyon, France), RASPADO O (Infirmerie protestante, Caluire et Cuire, France), ARNALSTEEN L, LAMBLIN A (Hôpital Privé La Louvière, Lille, France), DOLBEAU JB (Polyclinique Bordeaux Rive Droite, Lormon, France), AUVRAY S, LAMMENS S, LEPORRIER J, SIRISIER F (Hôpital privé Saint Martin, Caen, France), DILEON S (Clinique Saint Roch, Cavaillon, France).
Funding
Webhosting of GRACE-audit data was funded by the “Caisse National D’Assurance Maladie.”
Author information
Authors and Affiliations
Consortia
Contributions
AV contributed to conception, design, analysis and interpretation of data; manuscript author provided criticism of the manuscript, drafted the article and revised it for important intellectual content. Final approval of the version to be published. HM, EC, MO, ED, CMM, AW, JMR, SO, JJ have provided care for study patients, provided criticism of the manuscript, drafted the article and revised it for important intellectual content. Final approval of the version to be published. JFH contributed to methodology, statistical analysis and interpretation. Final approval of the version to be published. KS contributed to conception, design, analysis and interpretation of data, provided criticism of the manuscript, drafted the article and revised it for important intellectual content. Final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Venara, A., Meillat, H., Cotte, E. et al. Incidence and Risk Factors for Severity of Postoperative Ileus After Colorectal Surgery: A Prospective Registry Data Analysis. World J Surg 44, 957–966 (2020). https://doi.org/10.1007/s00268-019-05278-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05278-3