Abstract
Background
We investigated the analgesic efficacy of bilateral superficial cervical plexus block in patients undergoing thyroidectomy and to determine whether it reduces the adverse effects of general anesthesia.
Methods
We prospectively recruited 162 patients who underwent elective thyroid operations from March 2006 to October 2007. They were randomly assigned to receive a bilateral superficial cervical block (12 ml per side) with isotonic saline (group A; n = 56), bupivacaine 0.5% (group B; n = 52), or levobupivacaine 0.5% (group C; n = 54) after induction of general anesthesia. The analgesic efficacy of the block was assessed with: intraoperative anesthetics (desflurane), numbers of patients needing postoperative analgesics, the time to the first analgesics required, and pain intensity by visual analog scale (VAS). Postoperative nausea and vomiting (PONV) for 24 h were also assessed by the “PONV grade.” We also compared hospital stay, operative time, and discomfort in swallowing.
Results
There were no significant differences in patient characteristics. Each average end-tidal desflurane concentration was 5.8, 3.9, and 3.8% in groups A, B, and C, respectively (p < 0.001). Fewer patients in groups B and C required analgesics (A: B: C = 33:8:7; p < 0.001), and it took longer before the first analgesic dose was needed postoperatively (group A: B: C = 82.1:360.8:410.1 min; p < 0.001). Postoperative pain VAS were lower in groups B and C for the first 24 h postoperatively (p < 0.001). Incidences of overall and severe PONV were lower, however, there were not sufficient numbers of patients to detect differences in PONV among the three groups. Hospital stay was shorter in group B and group C (p = 0.011). There was no significant difference in operative time and postoperative swallowing pain among the three groups.
Conclusions
Bilateral superficial cervical plexus block reduces general anesthetics required during thyroidectomy. It also significantly lowers the severity of postoperative pain during the first 24 h and shortens the hospital stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid operations can cause mild to moderate incisional pain. In addition, discomfort in swallowing, burning sensation in the throat, nausea, and vomiting can be caused by the operation or by general anesthesia. These affect a majority of the patients, especially within the first day after operation [1, 2]. Surgeons and anesthesiologists have attempted to prevent or treat these problems with various modalities, such as opioids and nonsteroidal antiinflamatory drugs (NSAIDs), or with additional locoregional anesthesia techniques. Locoregional anesthesia, such as local anesthetic wound infiltration (LWI), bilateral superficial cervical plexus block (BSCPB), and bilateral combined superficial and deep cervical plexus block, can potentially reduce postoperative pain in patients who undergo thyroid operations [3–5].
Bilateral superficial cervical plexus block (BSCPB) is a popular regional anesthesia technique for its feasibility and efficacy. The aim of the present study was to investigate the efficacy of BSCPB by measuring postoperative pain visual analog scores (VAS) and postoperative analgesic requirement and intraoperative inhalation anesthetics required. In addition, we also wished to determine if BSCPB can reduce swallowing pain, and postoperative nausea and vomiting (PONV) in patients undergoing thyroidectomy.
Patients and methods
Patients
This study was approved by the Institutional Research Board (IRB) of Tri-service General Hospital (TSGH). A total of 179 patients underwent elective thyroid operations at TSGH from March 2006 to October 2007. We excluded 17 patients because of redo operations (n = 10), recent use of analgesics (n = 5, opioids or NSAIDs within 2 weeks), or inability to use the pain VAS scoring system for pain assessment (n = 2). All procedures were performed by the same team of anesthetists and surgeons (2 anesthesiologists and 2 surgeons, 2 surgical nurses, and 1 research staff).
Materials and methods
Using a random number sequence and sealed envelopes, 162 patients were assigned to receive a bilateral superficial cervical block (12 ml per side) with isotonic sodium chloride (group A; n = 56), bupivacaine 0.5% (group B; n = 52), or levobupivacaine 0.5% (group C; n = 54) after induction of general anesthesia. Three auditory evoked potential (AEP) electrodes (Danmeter A/S, Odense, Denmark) used to measure depth of anesthesia were placed at the mid-forehead (+), left forehead (reference), and left mastoid (−) of all patients before general anesthesia induction. Baseline arterial-line autoregressive index (AAI) (A-Line Monitor; Danmeter A/S) was recorded before anesthesia induction. General anesthesia was induced with fentanyl 2 μg/kg, 2% lidocaine (1.5 mg/kg), 2 mg cisatracurium, and 2–4 mg/kg propofol. After of the patient lost consciousness, 1.5 mg/kg succinylcholine was administered and tracheal intubation was performed until the AAI decreased to 20 [6]. Anesthesia was maintained with desflurane and oxygen. After general anesthesia induction, BSCPB was performed by the surgeon with a 22-gauge needle inserted into the mid-portion of the posterior border of the sternocleidomastoid muscle 1–2 cm deep, between the landmarks of mastoid process and C-6 transverse process. Next, 6 ml of anesthetic or saline was injected horizontally and the other 6 ml was injected caudad toward the sternal notch. After a 15-min high-flow oxygen wash-in (100% oxygen at a flow rate of 2 l/min) to fill the functional residual capacity of the lungs, desflurane was titrated in 100% oxygen at a flow rate of 300 ml/min to maintain an adequate anesthesia depth with a target AAI of 15–25 during the operation. The anesthesiologist who controlled the desflurane titration during the procedure was blinded to the study drug used. The BSCPB solutions were prepared by a surgical nurse who did not participate in the anesthesia care or evaluation of the patients. The AAI for all patients was kept at a target value range of 20 ± 5; desflurane concentration was reduced or increased by 2% in order to keep the AAI within the target range. Supplemental fentanyl (50 mcg) was prescribed in both groups if hemodynamic control could not be achieved within 5 min by a sequential 2% increase in desflurane concentration. The AAI was recorded at 1 h after skin incision and through the operation to confirm the level of AAI to be between 15 and 25. This is done to prevent awareness of patients by continuously adjusting desflurane during maintenance of anesthesia. If the AAI exceeded 25 or hypertension and tachycardia developed, desflurane was adjusted by 2% increments; if the AAI was less than 15 and was associated with hypotension, we applied 2% decrements of desflurane. The concentrations of end-tidal desflurane during operation were also recorded in parallel with the AAI records. Average desflurane concentration is the exhaled desflurane concentration recorded 1 h following BSCPB block in all groups, after the drug used for BSCPB has stabilized.
After operation, patients were sent to the postanesthesia care unit (PACU) for 1 h and then transferred to the ward. We evaluated postoperative pain with VAS (0: no pain, to 10: the worst imaginable pain) once at PACU and then every 4 h on the ward for 24 h. If the patient’s pain VAS was higher than 4, rescue analgesics were administrated with ketorolac 30 mg intravenously at 6-h intervals or longer. Nausea and vomiting were evaluated by “PONV score” as 1 = no nausea; 2 = mild nausea; 3 = severe nausea; 4 = retching and/or vomiting. Severe PONV was defined as grades 3 and 4; mild or non-PONV was defined as grade 1–2 [2]. When severe PONV developed, rescue antiemetics were administrated with metoclopramide [7, 8]. Operative time, postoperative swallowing pain, PONV, rescue analgesics, rescue antiemetics, and hospital stay were recorded by a member of the research staff.
Statistical analyses
The continuous data were analyzed by the one-way analysis of variance (ANOVA) test, and categorical data were tested by the chi-square test. Pain scores and analgesic consumption are reported as median and range, and differences between groups were analyzed with the nonparametric Kruskal–Wallis test. The statistical software used was S-Plus 2000 (CANdiensten, Amsterdam, The Netherlands). Differences were considered significant at p < 0.05.
Results
The demographics, types of operation, and intraoperative additional fentanyl requirement in the three groups are summarized in Table 1.
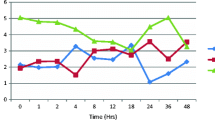
Desflurane requirements were lower in groups B and C (Table 2). Each average end-tidal desflurane concentration was 5.8 (± 0.58)%, 3.9 (± 0.56)%, and 3.8 (± 0.53)% in groups A, B, and C, respectively (p < 0.001; one-way ANOVA test). Postoperative pain VAS (Fig. 1) showed less pain in groups B and C than in group A at 2, 4, 8, 12, 16, 20, and 24 h after operation (p < 0.001; nonparametric Kruskal–Wallis test). There was no significant difference between groups B and C. Fifty-five patients developed postoperative nausea and vomiting; including 19 severe PONV (8, 5, and 6 in groups A, B, and C respectively) and 36 mild PONV (13, 14, and 9 in groups A, B, and C, respectively) (Table 2).
Visual analog scale (VAS) pain scores before discharge from the postanesthesia care unit (2 h postoperatively), and at 6 h, 10 h, 14 h, 18 h, 22 h, and 26 h after thyroidectomy or parathyroidectomy. The box represents the 25th and 75th percentiles and the median is represented by the solid line. Error bars above and below the box mark the 10th and 90th percentiles. P-values at all time period were less than 0.001
Mean operative times were 152.9 min (range: 56.4–345 min), 156.4 min (range: 55–395 min), and 164.1 min (range: 49–337 min) (p = 0.492; one-way ANOVA test). Mean hospital stays were 2.9 days (range: 1–5 days), 2.5 days (range: 1–6 days), and 2.4 days (range: 1–5 days) (p = 0.011; one-way ANOVA test). Number of patients requiring analgesics within 24 h postoperatively for the three groups were 33, 8, and 7 (p < 0.001; chi-square test). Mean times to first postoperative analgesic requirement were 82.1, 360.8, and 410.1 min (p = 0.0004; one-way ANOVA test) in groups A, B, and C, respectively. A total of 116 patients had pain with swallowing postoperatively; the incidence among the three groups did not differ (71.4, 72.2, and 64.9 % in groups A, B and C, respectively; p = 0.504; chi-square test) (Table 2). Procedure related complications were rare; only one patient had transient diaphragmatic paresis and brachial plexus block (0.6%). The patient only had transient unilateral phrenic nerve and brachial plexus blocks with mild dyspnea and weakness of the involved arm, which resolved spontaneously 6 h postoperatively. No patients reported awareness during the operation.
Discussion
This prospectively randomized study showed that a bilateral superficial cervical block combined with general anesthesia reduced postoperative pain and incidence and duration of severe PONV in patients who underwent thyroid and parathyroid operations.
Andrieu et al. [9] performed BSCPB with/without clonidine and found reduced intraoperative and postoperative analgesic requirement. However, other studies showed that local and regional anesthetic techniques did not decrease analgesic requirement after thyroid surgery [10, 11]. These results were based only on postoperative pain VAS and analgesic requirement. Procedure failure and ineffective regional anesthesia may sometimes be a problem. Unfortunately, there is no good method to confirm procedure success. Andrieu et al. used systolic blood pressure recorded at induction, incision, end of resection, and extubation to evaluate the process efficacy [9]. Among the three groups, we kept the same depth of anesthesia, maintaining a target range of arterial-line autoregressive index (AAI) between 15 and 25. The AAI is calculated from the middle latency auditory evoked potentials (AEPs) and the electroencephalogram (EEG), and it is helpful in detecting intraoperative awareness with recall and decreasing anesthetic requirements [12, 13]. Struys et al. concluded that AAI monitoring is an accurate indicator of the level of sedation and loss of consciousness [14]. Lu et al. also demonstrated that, at an AAI of 20 ± 5, desflurane can maintain an adequate anesthetic effect [12]. Therefore, if concentration of end-tidal desflurane is reduced 1 h after BSCPB, it may help to confirm procedure success. In groups B and C in the present study, lower average concentration of end-tidal desflurane both proved the efficacy of regional anesthesia and lowered the incidence of PONV.
Different techniques and local anesthetic agents used for BSCPB in previous studies could be another reason for the controversy surrounding the use of this form of anesthesia. There are two-point and three-point injection techniques for BSCPB. The standard two-point injection technique is to insert the needle at the junction of the upper and middle thirds of the posterior border of the sternocleidomastoid muscle at 1–2 cm depth (in a subcutaneous plane), then inject 2–3 ml prepared anesthetic cephalad toward the mastoid, and then inject the other 2–3 ml caudad toward the clavicle [15]. The three-point injection technique added the horizontal injection. Our technique of BSCPB is a modified two-point injection. We skipped the injection cephalad toward the mastoid; instead, we emphasized the lower neck compartment. Dieudonne et al. used a three-point injection with 10 ml of bupivacaine 0.25% and 1:200,000 epinephrine [4]. Andrieu et al. used a three-point injection with 10 ml ropivacaine and clonidine [9]. Eti et al. used a two-point injection with 0.25% bupivacaine 15 ml [10]. In addition to BSCPB, Suh, Inabnet, and Pintaric [16–18] used combined (superficial and deep) cervical plexus block. Levobupivacaine is the S(−)-enantiomer of the racemic local anesthetic bupivacaine. It is superior to bupivacaine for its less toxic effect on the central nervous and cardiovascular systems [19]. There are few studies comparing the efficacies of different local anesthetics in cervical blocks. Levobupivacaine seems to be more potent than bupivacaine in in vitro studies [20]. However, there is no difference between the two anesthetics in in vivo studies [21]. In our study, we found that levobupivacaine has a slightly longer duration of action.
Local anesthetic wound infiltration (LWI) is an excellent way to reduce postoperative pain in hernia operations [22]. For deeper procedures like thyroidectomy, the results are conflicting. Some investigators found BSCBP to be superior to LWI [1]; however Dieudonne et al. found no difference in reduction of postoperative analgesic requirement between the two techniques [4]. The reason for the controversy might be that there is no standard way to perform LWI, which affects a relatively smaller, more superficial acting area and is of shorter duration.
Nausea and vomiting after neck operations can be caused by intubations, inhalation anesthetics, perioperative analgesics, and surgical manipulation. Sonner et al. reported that 54% of their patients had nausea and vomiting after thyroidectomy, with the incidence more common in women and in those who had inhalation anesthesia. They scored postoperative nausea and vomiting (PONV) after thyroidectomy as grades 1–4 and defined severe PONV as grades 3 and 4 [2]. Our incidence of PONV in the three groups was 32.9%. This lower rate may be related to our routine use of 5 mg dexamethasone intravenously during thyroid operations [23]. Fewer patients in our groups B and C developed severe PONV. Unfortunately, our study did not have a large enough number of patients to detect differences in PONV among the three groups.
Post-thyroidectomy swallowing pain has received less attention in the literature. Suh et al. reported that bilateral superficial cervical plexus block with or without deep cervical plexus block reduced incision pain at rest and on swallowing at 0, 2, and 4 h postoperatively. They concluded that BSCPB is an effective technique with fewer side effects and greater patient satisfaction [16]. Again, in our study, because of the insufficient number of patients, there was no statistically valid basis from which to conclude if there was a difference in postoperative swallowing pain among the three groups. Superficial cervical block may not be able to cover deeper compartments to alleviate swallowing pain. We do not use deep cervical block because of the higher rate of complications, such as intravenous injection, hematoma, nerve injury, and unintended blockade of vagus nerve, brachial plexus [17], or phrenic nerve [24]. We had one patient (0.6%) who had a phrenic nerve and brachial plexus block that resolved after 6 h. She was thin and the injection was likely deeper than intended.
Cervical plexus block without general anesthesia is an option. Pintaric et al. used either superficial or combined cervical plexus block (CCPB) without general anesthesia effectively in minimally invasive parathyroidectomy [18]. Inabnet et al. and Arora et al. [17, 25] also found regional and local anesthesia without general anesthesia to be safe for same-day discharge after thyroidectomy. We have occasionally used superficial cervical plexus block without general anesthesia in high-risk patients. Factors that influence this decision may include goiter size, extent of operation, airway protection, fire risk, neck pressure, coughing during surgical manipulation, and patient anxiety. The percentage of conversion to general anesthesia was 1.8% because of ineffective anesthesia and changes in operative extent [17]. Contraindications for local/regional anesthesia without general anesthesia for thyroid surgery may include communication barrier (dementia, language barrier, mental retardation), planned sternotomy (retrosternal extension), additional procedures, known or suspected locally invasive cancer, allergy to local anesthetics, patient preference for general anesthesia, and cervical lymphadenectomy [25]. Either BSCPB or bilateral CCPB combined with general anesthesia may be safer and more widely applicable in low anesthetic risk patients.
In conclusion, bilateral superficial cervical plexus block is effective in reducing the amount of general anesthetic required during thyroidectomy. It also significantly lowers the severity of postoperative pain during the first 24 h and shortens the hospital stay.
References
Lacoste L, Thomas D, Kraimps JL et al (1997) Postthyroidectomy analgesia: morphine, buprenorphine or bupivacaine? J Clin Anesth 9:189–193
Sonner JM, Hynson JM, Clark O et al (1997) Nausea and vomiting following thyroid and parathyroid surgery. J Clin Anesth 9:398–402
Gozal Y, Shapira SC, Gozal D et al (1994) Bupivacaine wound infiltration in thyroid surgery reduces postoperative pain and opioid demand. Acta Anaesthesiol Scand 38:813–815
Dieudonne N, Gomola A, Bonnichon P et al (2001) Prevention of postoperative pain after thyroid surgery: a double-blind randomized study of bilateral superficial cervical plexus blocks. Anesth Analg 92:1538–1542
Aunac S, Carlier M, Singelyn F et al (2002) The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg 95:746–750
Kuo CP, Chen KM, Wu CT et al (2006) Utility of the auditory evoked potentials index as an indicator for endotracheal intubation. Acta Anaesthesiol Taiwan 44:205–210
Fujii Y (2008) The benefits and risks of different therapies in preventing postoperative nausea and vomiting in patients undergoing thyroid surgery. Curr Drug Saf 3:27–34
Fujii Y (2006) Prophylaxis of postoperative nausea and vomiting in patients scheduled for breast surgery. Clin Drug Investig 26:427–437
Andrieu G, Amrouni H, Robin E et al (2007) Analgesic efficacy of bilateral superficial cervical plexus block administered before thyroid surgery under general anaesthesia. Br J Anaesth 99:561–566
Eti Z, Irmak P, Gulluoglu BM et al (2006) Does bilateral superficial cervical plexus block decrease analgesic requirement after thyroid surgery? Anesth Analg 102:1174–1176
Herbland A, Cantini O, Reynier P et al (2006) The bilateral superficial cervical plexus block with 0.75% ropivacaine administrated before or after surgery dose not prevent postoperative pain after total thyroidectomy. Reg Anesth Pain Med 31:31–39
Lu CH, Borel CO, Wu CT et al (2005) Combined general-epidural anesthesia decreases the desflurane requirement for equivalent A-line ARX index in colorectal surgery. Acta Anaesthesiol Scand 49:1063–1067
Horng HC, Kuo CP, Ho CC et al (2007) Cost analysis of three anesthetic regimens under auditory evoked potentials monitoring in gynecologic laparoscopic surgery. Acta Anaesthesiol Taiwan 45:205–210
Struys MS, Eric WJ, Warren S et al (2002) Performance of the ARX-derived auditory evoked potential index as an indicator of anesthetic depth. A comparison with Bispectral Index and hemodynamic measures during propofol administration. Anesthesiology 96:803–816
Morgan GE Jr, Mikhail MS, Murray MJ (2006) Peripheral nerve blocks. Section III. Regional anesthesia & pain management, chapter 17. Clinical anesthesiology. McGraw-Hill, New York, pp 353–354
Suh YJ, Kim YS, In JH et al (2009) Comparison of analgesic efficacy between bilateral superficial and combined (superficial and deep) cervical plexus block administered before thyroid surgery. Eur J Anaesthesiol 26:1043–1047
Inabnet WB, Shifrin A, Ahmed L et al (2008) Safety of same day discharge in patients undergoing sutureless thyroidectomy: a comparison of local and general anesthesia. Thyroid 18:57–61
Pintaric TS, Hocevar M, Jereb S et al (2007) A prospective, randomized comparison between combined (deep and superficial) and superficial cervical plexus block with levobupivacaine for minimally invasive parathyroidectomy. Anesth Analg 105:1160–1163
Foster RH, Markham A (2000) Levobupivacaine: a review of its pharmacology and use as a local anesthetic. Drugs 59:551–579
Kanai Y, Katsuki H, Takasaki M (2000) Comparisons of the anesthetic potency and intracellular concentrations of S(−) and R(+) bupivacaine and ropivacaine in crayfish giant axon in vitro. Anesth Analg 90(2):415–420
Baskan S, Taspinar V, Ozdogan L et al (2010) Comparison of 0.25% levobupivacaine and 0.25% bupivacaine for posterior approach interscalene brachial plexus block. J Anesth 24:38–42
Dahl JB, Moiniche S, Kehlet H (1994) Wound infiltration with local anaesthetics for postoperative pain relief. Acta Anaesthesiol Scand 38:7–14
Fujii Y, Nakayama M (2007) Efficacy of dexamethasone for reducing postoperative nausea and vomiting and analgesic requirements after thyroidectomy. Otolaryngol Head Neck Surg 136:274–277
Weiss A, Isselhorst C, Gahlen J et al (2005) Acute respiratory failure after deep cervical plexus block for carotid endarterectomy as a result of bilateral recurrent laryngeal nerve paralysis. Acta Anaesthesiol Scand 49:715–719
Arora N, Dhar P, Fahey TJ III (2006) Seminars: local and regional anesthesia for thyroid surgery. J Surg Oncol 94:708–713
Acknowledgments
The study was supported by grants from Triservice General Hospital of Taiwan (TSGH-C96-72). The paper was presented at the International Surgical Week 2009, Adelaide, Australia, 6–10, September 2009. The author, Shih, was the winner of Selwyn Taylor Award for the best poster of endocrine surgery.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Shih, ML., Duh, QY., Hsieh, CB. et al. Bilateral Superficial Cervical Plexus Block Combined with General Anesthesia Administered in Thyroid Operations. World J Surg 34, 2338–2343 (2010). https://doi.org/10.1007/s00268-010-0698-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0698-7