Abstract
Background
Accurate knowledge of the fracture of cranial bone can provide insight into the prevention of skull fracture injuries and help aid the design of energy-absorbing head protection systems and safety helmets. When cranial bone needs to be removed or is lost, subsequent reconstruction of the defect is necessary to protect the underlying brain, or correct esthetic deformities, or both. Ideal reconstruction of defected bone is possible utilizing a biocompatible implant with a bone-like design individualized for the specific patient. The purpose of this study is to investigate the anatomical and mechanical characteristics of fresh frozen human parietal bones and determine compliance of polylactic acid-based personalized three-dimensional implants in terms of mechanical properties in order to replace such defective bones.
Methods
Parietal bone specimens were extracted from 19 fresh frozen cadavers. Morphological parameters of individual bone specimens were measured using Image J software. Three-point bend tests were performed to extract Young’s modulus and tensile strength of the specimens from the measured force and displacement data by modeling the bone specimens as curved linear elastic beams. Also, three-point bend tests were performed to polylactic acid-based three-dimensional replicas mimicking geometry of the bone specimens in order to determine whether the material’s Young’s modulus and tensile strength properties comply with parietal bones.
Results
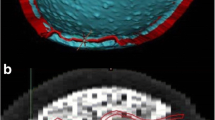
Entire fresh parietal specimens were observed to be comprised of a three-layered structure: external layers consisting of compact, high-density cortical bone and the central layer consisting of low-density, irregularly porous bone structure. Mean thickness of three-layered structure was 6.25 ± 1.46 mm. Mean Young’s modulus and tensile strength of the specimens were 1.40 ± 1.34 GPa and 44.56 ± 21.94 MPa, respectively where no statistically significant differences among genders were detected (p > 0.05). Mean Young’s modulus and tensile strength of the polylactic acid-based three-dimensional implants mimicking geometry of the bone specimens were 1.8 ± 0.7 GPa and 72.8 ± 2.5 MPa, respectively.
Conclusions
Polylactic acid-based three-dimensional implants can be considered as acceptable candidates for temporary replacement of parietal defects in terms of mechanical properties.
Level of Evidence: Not ratable.









Similar content being viewed by others
References
Peltola MJ, Vallittu PK, Vuorinen V, Aho AA, Puntala A, Aitasalo KM (2012) Novel composite implant in craniofacial bone reconstruction. Eur Arch Otorhinolaryngol 269(2):623–628
Spetzger U, Vougioukas V, Schipper J (2010) Materials and techniques for osseous skull reconstruction. Minim Invasive Ther Allied Technol 19(2):110–121
Aitasalo KM, Piitulainen JM, Rekola J, Vallittu PK (2014) Craniofacial bone reconstruction with bioactive fiber-reinforced composite implant. Head Neck 36(5):722–728
De Bonis P, Frassanito P, Mangiola A, Nucci CG, Anile C, Pompucci A (2012) Cranial repair: how complicated is filling a “hole”? J Neurotrauma 29(6):1071–1076
Hanasono MM, Goel N, DeMonte F (2009) Calvarial reconstruction with polyetheretherketone implants. Ann Plast Surg 62(6):653–655
Liao YL, Lu CF, Sun YN, Wu CT, Lee JD, Lee ST, Wu YT (2011) Three-dimensional reconstruction of cranial defect using active contour model and image registration. Med Biol Eng Comput 49(2):203–211
Chim H, Schantz JT (2005) New frontiers in calvarial reconstruction: integrating computer-assisted design and tissue engineering in cranioplasty. Plast Reconstr Surg 116(6):1726–1741
Eppley BL, Kilgo M, Coleman JJ III (2002) Cranial reconstruction with computer-generated hard-tissue replacement patient-matched implants: indications, surgical technique, and long-term follow-up. Plast Reconstr Surg 109(3):864–871
Evans FG, Lissner HR (1957) Tensile and compressive strength of human parietal bone. J Appl Physiol 10(3):493–497
Jones JR (2013) Review of bioactive glass: from Hench to hybrids. Acta Biomater 9(1):4457–4486
Staffa G, Nataloni A, Compagnone C, Servadei F (2007) Custom made cranioplasty prostheses in porous hydroxy-apatite using 3D design techniques: 7 years experience in 25 patients. Acta Neurochir 149(2):161–170 discussion 170
Ng ZY, Ang WJ, Nawaz I (2014) Computer-designed polyetheretherketone implants versus titanium mesh (± acrylic cement) in alloplastic cranioplasty: a retrospective single-surgeon, single-center study. J Craniofac Surg 25(2):e185–e189
Ng ZY, Nawaz I (2014) Computer-designed PEEK implants: a peek into the future of cranioplasty? J Craniofac Surg 25(1):e55–e58
Lindfors NC, Heikkilä JT, Koski I, Mattila K, Aho AJ (2009) Bioactive glass and autogenous bone as a bone graft substitutes in benign bone tumors. J Biomed Mater Res B Appl Biomater 90(1):131–136
Neovius E, Engstrand T (2010) Craniofacial reconstruction with bone and biomaterials: review over the last 11 years. J Plast Reconstr Aesthet Surg 63(10):1615–1623
Rosenthal G, Ng I, Moscovici S, Lee KK, Lay T, Martin C, Manley GT (2014) Polyetheretherketone implants for the repair of large cranial defects: a 3-center experience. Neurosurgery 75(5):523–529; discussion 528-9
Majola A, Vainionpää S, Vihtonen K, Mero M, Vasenius J, Törmälä P, Rokkanen P (1991) Absorption, biocompatibility, and fixation properties of polylactic acid in bone tissue: an experimental study in rats. Clin Orthop Relat Res 268:260–269
Wittbrodt B, Pearce JM (2015) The effects of PLA color on material properties of 3-D printed components. Additive Manufacturing 8:110–116
Auperrin A, Delille R, Lesueur D, Bruyere K, Masson C, Drazetic P (2014) Geometrical and material parameters to assess the macroscopic mechanical behaviour of fresh cranial bone samples. J Biomech 47(5):1180–1185
Jasinoski SC, Reddy BD, Louw KK, Chinsamy A (2010) Mechanics of cranial sutures using the finite element method. J Biomech 43(16):3104–3111
Topp T, Muller T, Huss S, Kann PH, Weihe E, Ruchholtz S, Zettl RP (2012) Embalmed and fresh frozen human bones in orthopedic cadaveric studies: which bone is authentic and feasible? Acta Orthop 83(5):543–547
Torimitsu S, Nishida Y, Takano T, Yajima D, Inokuchi G, Makino Y, Motomura A, Chiba F, Yamaguchi R, Hashimoto M, Hoshioka Y, Iwase H (2015) Differences in biomechanical properties and thickness among frontal and parietal bones in a Japanese sample. Forensic Sci Int 252(190):e191–e196
Young WC, Budynas RG (2002) Roark’s formulas for stress and strain, vol 7 McGraw-Hill New York,
Motherway JA, Verschueren P, Van der Perre G, Vander Sloten J, Gilchrist MD (2009) The mechanical properties of cranial bone: the effect of loading rate and cranial sampling position. J Biomech 42(13):2129–2135
Boresi AP, Schmidt RJ, Sidebottom OM (1993) Advanced mechanics of materials, vol 6. Wiley, New York
Peterson J, Dechow PC (2002) Material properties of the inner and outer cortical tables of the human parietal bone. Anat Rec 268(1):7–15
Rahmoun J, Auperrin A, Delille R, Naceur H, Drazetic P (2014) Characterization and micromechanical modeling of the human cranial bone elastic properties. Mech Res Commun 60:7–14
van der Meer WJ, Bos RR, Vissink A, Visser A (2013) Digital planning of cranial implants. Br J Oral Maxillofac Surg 51(5):450–452
Tuusa SM, Peltola MJ, Tirri T, Lassila LV, Vallittu PK (2007) Frontal bone defect repair with experimental glass-fiber-reinforced composite with bioactive glass granule coating. J Biomed Mater Res B Appl Biomater 82((1):149–155
Manrique OJ, Lalezarzadeh F, Dayan E, Shin J, Buchbinder D, Smith M (2015) Craniofacial reconstruction using patient-specific implants polyether ether ketone with computer-assisted planning. J Craniofac Surg 26(3):663–666
Staffa G, Barbanera A, Faiola A, Fricia M, Limoni P, Mottaran R, Zanotti B, Stefini R (2012) Custom made bioceramic implants in complex and large cranial reconstruction: a two-year follow-up. J Craniomaxillofac Surg 40(3):e65–e70
Lynnerup N (2001) Cranial thickness in relation to age, sex and general body build in a Danish forensic sample. Forensic Sci Int 117(1–2):45–51
Torimitsu S, Nishida Y, Takano T, Koizumi Y, Hayakawa M, Yajima D, Inokuchi G, Makino Y, Motomura A, Chiba F, Iwase H (2014) Effects of the freezing and thawing process on biomechanical properties of the human skull. Leg Med (Tokyo) 16(2):102–105
Shaoo D, Deck C, Yoganandan N, Willinger R (2015) Influence of stiffness and shape of contact surface on skull fractures and biomechanical metrics of the human head of different population underlateral impacts. Accid Anal Prev 80:97–105
Torimitsu S, Nishida Y, Takano T, Koizumi Y, Makino Y, Yajima D, Hayakawa M, Inokuchi G, Motomura A, Chiba F, Otsuka K, Kobayashi K, Odo Y, Iwase H (2014) Statistical analysis of biomechanical properties of the adult skull and age-related structural changes by sex in a Japanese forensic sample. Forensic Sci Int 234:185.e1–185.e9
Rammos CK, Cayci C, Castro-Garcia JA, Feiz-Erfan I, Lettieri SC (2015) Patient-specific polyetheretherketone implants for repair of craniofacial defects. J Craniofac Surg 26(3):631–633
Neugebauer J, Stachulla G, Ritter L, Dreiseidler T, Mischkowski RA, Keeve E, Zoller JE (2010) Computer-aided manufacturing technologies for guided implant placement. Expert Rev Med Devices 7(1):113–129
Lethaus B, Safi Y, Ter Laak-Poort M, Kloss-Brandstätter A, Banki F, Robbenmenke C, Steinseifer U, Kessler P (2012) Cranioplasty with customized titanium and PEEK implants in a mechanical stress model. J Neurotrauma 29(6):1077–1083
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors declare that they have no conflict of interest.
Conflict of interest
Figen Govsa, Servet Celık, Tuncer Turhan, Volkan Sahın, Meral Celık, Korhan Sahın, Mehmet Asim Ozer, Zuhal Kazak declare that they have no conflict of interest.
Ethical approval
This study complies with the current laws of the country in which it was performed (15-11/44 10.11.2015).
Informed consent
This study was carried out in accordance with the protocols of our institution concerning patient data.
Rights and permissions
About this article
Cite this article
Govsa, F., Celik, S., Turhan, T. et al. The first step of patient-specific design calvarial implant: A quantitative analysis of fresh parietal bones. Eur J Plast Surg 41, 511–520 (2018). https://doi.org/10.1007/s00238-018-1411-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-018-1411-6