Abstract
Bioactive glass (BAG) and polymethyl methacrylate (PMMA) have been used in clinical applications. Antimicrobial BAG has the ability to attach chemically to surrounding bone, but it is not possible to bend, drill or shape BAG during the operation. PMMA has advantages in terms of shaping during the operation, but it does not attach chemically to the bone and is an exothermic material. To increase the usefulness of BAG and PMMA in skull bone defect reconstructions, a new composite implant containing BAG and PMMA in craniofacial reconstructions is presented. Three patients had pre-existing large defects in the calvarial and one in the midface area. An additive manufacturing (AM) model was used preoperatively for treatment planning and custom-made implant production. The trunk of the PMMA implant was coated with BAG granules. Clinical and radiological follow-up was performed postoperatively at 1 week, and 3, 6 and 12 months, and thereafter annually up to 5 years. Computer tomography (CT) and positron emission tomography (PET-CT) were performed at 12 and 24 months postoperatively. Uneventful clinical recovery with good esthetic and functional outcome was seen. CT and PET-CT findings supported good clinical outcome. The BAG–PMMA implant seems to be a promising craniofacial reconstruction alternative. However, more clinical experience is needed.
Similar content being viewed by others
Introduction
Traditional skull and facial bone reconstructions with hard tissues have a long history with good clinical outcomes [1–3]. However, they have certain disadvantages, e.g., donor site morbidity [4]. The benefits of synthetic materials are not only the avoidance of donor site morbidity and scars, but also shorter hospitalization time, lower expenses and known composition [5]. Metallic implants have been used alone [6] or combined with bone or hydroxyapatite cement in cranial bone reconstructions [7]. Polymethyl methacrylate (PMMA) resin, polyethylene and hydroxyapatite with various formulations have been utilized in cranial bone reconstructions [8, 9]. Although these materials are readily available for immediate application, they all require preparation, adaptation and contouring into the defect and, later on, resistance to traumatic insults is uncertain. Additive manufacturing technology (AM) has been applied to many medical specialties [10–13]. A custom-made skull bone implant can be produced based on the patient’s preoperative AM three-dimensional mode, and this will result in very high accuracy in terms of the form of the skull defect [14].
Composite implant materials
PMMA is one of the most widely used alloplastic materials in surgery [8, 15]. It has the advantages of being relatively well tolerated by soft tissues and of having a density similar to that of the bone, as well as low thermal conductivity. However, in situ use of PMMA, i.e., a resin mixture of polymer powder and monomer, causes an exothermic reaction by free-radical polymerization. In addition, foreign-body reaction with polymethyl methacrylate has been observed [15].
Bioactive glass S53P4 (BAG) particles of the composition SiO2 53.0; CaO 20.0; Na2O 23.0; P2O5 4.0 wt% have been used in various clinical indications [16–18]. Effects of BAG and clinically important bacteria have been studied experimentally [19, 20]. Microbes lost their viability when placed in contact with BAG [19, 20].
BAG is a brittle and rigid material. It is not possible to drill, bend or shape BAG during the reconstruction operation. Preoperative mechanical preparation of brittle BAG for individual implants is difficult because of the risk of microscopic fractures in the BAG implant, probably leading to an unsafe individual implant. PMMA has advantages in terms of shaping during the operation, but it does not attach chemically to the bone and it is an exothermic material. To variegate BAG and PMMA usefulness in skull bone defect reconstructions, a new composite implant containing BAG granules and PMMA is presented.
Materials and methods
Patients
Of four male patients (mean age of 41 years, range 19–66 years), three needed calvarial and one facial bone defect reconstruction (Table 1). The patients were operated in 2005–2006 in the Turku University Hospital Department of Otorhinolaryngology, Head and Neck Surgery. The study plan was reviewed and approved by the Joint Commission on Ethics of Turku University and Turku University Hospital.
Implants
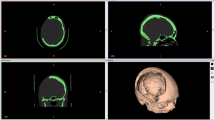
The defect in the patient’s skull (Fig. 1) was detected with a preoperative high-resolution three-dimensional CT study. With the help of the AM (Alphaform Ltd, Rusko, Finland), a custom-made implant (Fig. 2) was prepared by hand (Tables 2, 3). The resin matrix of the implant was a powder–liquid system PMMA bone cement (Palacos-R®, Heraueus Kulzer GmbH, Germany), and the surface of both sides of the implant was covered with exposed particles of BAG 0.5–0.8 mm in size (BonAlive™, BonAlive Biomaterials Ltd., Finland). The implant’s PMMA trunk was perforated with holes 1.5 mm in diameter (Figs. 2, 3) to enhance tissue ingrowth [21, 22] into the implant and body fluid perfusion (Figs. 2, 3). On the upper surface of the implant, a screw fixation rim with a thickness of 1.0 mm was used to insure the correct position of the implant in the calvarial bone defect and to prevent the implant from sinking too deep into contact with the lamina dura (Fig. 3). The implant was polymerized by autopolymerization, followed by finishing of the contour surfaces of the implant. Then, the implant was post-cured at a temperature of 120°C to optimize the degree of PMMA monomer conversion, thus reducing the quantity of residual monomers in the final implant [23, 24]. The implant was sterilized with the gamma sterilization method preoperatively with a 25 kGy irradiation dose and double packed for clinical use (Isotron Nederland, Netherlands).
Implantation technique
The defect site was prepared by isolation of the bone margins through underlying dural and overlying soft tissue dissection. The bony walls of the defects were completely removed from soft tissue. The implants were applied to the bone defects, and the correct position of the implant was ensured with screw fixation (Table 1; Figs. 2, 3). Only minor adjustment of the implants was made with a hand piece and burr under physiologic saline irrigation to achieve accurate implant fit into bony defects. An intraoral approach was used in one patient, whose lateral midface fracture in the right side could not be adequately reconstructed in three previous operations (Table 1, Fig. 4).
Follow-up examinations
The results of the clinical examinations and patients’ symptoms were recorded at 1 week, and 1, 3, 6 and 12 months, and thereafter, annually up to 5 years postoperatively (Table 1). Lateral skull X-ray pictures were obtained at each observation point and CT at 12 months. PET-CT from two patients was performed at 24 months postoperatively. Routine hematologic tests including C-reactive protein (CRP) and creatinine were carried out at postoperative controls only in the case of clinical need. In clinical examinations, special attention was paid to a progressive healing process with diminishing postoperative pain, skin wound healing and clinical position of the implant. In CT or skull X-ray studies, special attention was paid to the border between the implant and surrounding bone to detect any deviations of the permanent fit of the implant into the original defect (Fig. 5). In PET-CT with (18)F-fluoride ion marker, signs of activity of new bone formation between the bone defect margin and the implant were examined (Fig. 6).
PET-CT picture of implant 2 years after reconstruction. (18)F-fluoride marker was used. The implant is in the correct position in the skull. Metabolic activity is shown with colors (white arrows). The highest activity is shown with red and yellow, while green shows lower activity. The middle arrow shows activity on the implant’s outer surface (yellow and red areas), while the other two arrows show activity at the border between the implant and bone (yellow and red areas, patient 1)
Results
Although the defects needed large bone reconstructions (Table 1; Figs. 1–4), there was no mortality. After operation, in the early phase of clinical follow-up from 1 week to 3 months, a progressive healing process with diminishing postoperative clinical symptoms and normally progressing skin wound healing was seen. In skull X-ray studies and clinical examinations, the implants were in the original positions (Figs. 2, 3, 5). Thereafter, the postoperative course was uneventful. However, there was no donor site morbidity because the custom-made implants did not need any graft operations. As a complication, one of the skull bone defect patients had epidural hemorrhage immediately after the operation, which needed surgical intervention. Thereafter, the postoperative course was uneventful. The early and the late esthetic and functional outcomes were good in all three calvarial reconstruction patients, and a satisfactory outcome was achieved with orbit reconstruction (Figs. 5, 7). Hematologic tests revealed no abnormal findings throughout the study. At 2 years postoperatively, both CT and PET-CT studies were performed. In CT studies, the implants were in the original position and an impression of new bone formation was seen (Fig. 5). PET-CT showed activity [25, 26] similar to that reported before with bone healing (Fig. 6).
Discussion
Reconstruction of a large skull bone defect is one of the most demanding challenges for surgeons. The gold standard with long clinical experience in bone reconstruction is the use of autogenic bone [1]. However, this method has a disadvantage, namely, donor site morbidity [4] and sometimes enough autogenic tissue for large bone reconstructions or new operations is not available. In this study, three large skull bone defect reconstructions and one orbit reconstruction with a new implant containing BAG and PMMA are presented. AM technologies were utilized in both preoperative planning and in custom-made implant manufacturing. The patients were followed up for up to 5 years. In the present series, there were no long-term complications such as implant-induced skull resorption, loosening of implant or later infections. The esthetic and functional outcomes were good. The combination of biomaterials and AM can offer novel solutions for difficult skull bone reconstructions.
Exposed BAG particles on the surface of the PMMA implant improves bone formation at the interface of the PMMA implant and surrounding bone [27]. In addition, the perforated surface of the implant favors tissue ingrowth of the implant [21, 22]. The bone growth between implant and skull will result in firm adhesion, which in turn may prevent long-term complications. In this study, supposed new bone formation [27] was seen indirectly between an implant and surrounding bone (Figs. 5, 6). These results are similar to those reported before with bone healing [25, 26]. The advantages of the presented composite material are the bioactivity and osteoconductivity of BAG [27], including antimicrobial properties shown in experimental studies [16, 19, 20]. The implants contain no metals related to artefacts in imaging studies, e.g., in CT and MRI [11]. The implant can be fixed with screws or sutures or even set without specific fixation into the calvarial defect under soft tissues. The implant can be shaped with manual and hand-piece instruments. In addition, BAG particles and PMMA can be added to the implant in clinical conditions, when it is necessary to make the implant larger or stronger, e.g., in the case of a larger postoperative defect than estimated in preoperative planning. Donor site morbidity is not related to the custom-made BAG and PMMA composite implant.
In bone reconstruction with biomaterials, the most important practical factors are an adequate knowledge of the biomaterials, their advantages and disadvantages, and the exact composition of the used composite material (Tables 2, 3). Irritation reactions because of exothermic polymerization of PMMA and the presence of free and residual PMMA monomers before and after polymerization [15] can be minimized, when the implant is manufactured in controlled conditions before the operation [23, 24, 28–30]. The total cost of the implant in this study was 2,500 €. However, the shortening of the operating time decreases the total costs of implant reconstruction compared to conventional methods [5, 7, 12]. In the future, the new industrial manufacturing methods will probably reduce the price of the implant.
However, a longer clinical follow-up with more patients is needed before final conclusions can be drawn about the presented composite implant.
References
Tessier P, Kawamoto H, Matthews D et al (2005) Autogenous bone grafts and bone substitute—tools and techniques: I A 20000-case experience in maxillofacial and craniofacial surgery. Plast Reconstr Surg Suppl 5:6–24
Lenz JH, Henkel KO, Hingst V, von Versen R, Gundlach K (2003) Reconstruction of the frontal calvarial continuity in a child using freeze-preserved autogenous bone grafts. J Craniomaxillofac Surg 3:154–158
Rodrigues M, O`Malley BW Jr, Staecker H, Tamargo R (2004) Extended pericranial flap and bone graft reconstruction in anterior skull base surgery. Otolaryngol Head Neck Surg 1:69–76
Ahlmann E, Patzakis M, Roidis N et al (2002) Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am 5:716–720
Eppley BL (1999) Alloplastic implantation. Plast Reconstr Surg 104:1761–1783
Winder J, Cooke RS, Gray J et al (1999) Medical rapid prototyping and 3D CT in the manufacture of custom made cranial titanium plates. J Med Eng Technol 1:26–28
Ducic Y (2002) Titanium mesh and hydroxyapatite cement cranioplasty: a report of 20 cases. J Oral Maxillofac Surg 3:272–276
Moreira-Gonzalez A, Jackson IT, Miyawaki T et al (2003) Clinical outcome in cranioplasty: critical review in long-term follow-up. J Craniofac Surg 5:144–153
Kveton JF, Coelho DH (2004) Hydroxyapatite cement in temporal bone surgery: a 10 year experience. Laryngoscope 1:33–37
Mankovich NJ, Samson D, Pratt W et al (2005) Surgical planning using three-dimensional imaging and computer modeling. Otolaryngol Clin North Am 5:875–879
Winder J, Bibb R (2005) Medical rapid prototyping technologies: state of the art and current limitations for application in oral and maxillofacial surgery. J Oral Maxillofac Surg 63:1006–1015
Suzuki M, Ogawa Y, Kawano A et al (2004) Rapid prototyping of temporal bone for surgical training and medical education. Acta Otolaryngol 4:400–402
Sarment DP, Sukovic P, Clinthorne N (2003) Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants 4:571–577
Eppley BL, Kilgo M, Coleman JJ III (2002) Cranial reconstruction with computer-generated hard-tissue replacement patient-matched implants: indications, surgical technique, and long-term follow-up. Plast Reconstr Surg 109:864–871
Stelnicki EJ, Ousterhout DK (1996) Prevention of thermal injury induced by the application of polymethylmetacrylate to the calvarium. J Craniofac Surg 7:192–195
Peltola M, Aitasalo K, Suonpää J et al (2006) Bioactive glass S53P4 in frontal sinus obliteration: a long-term clinical experience. Head Neck 28:834–841
Turunen T, Peltola J, Yli-Urpo A et al (2004) Bioactive glass granules as a bone adjunctive material in maxillary sinus floor augmentation. Clin Oral Implants Res 2:135–141
Lindfors NC, Heikkilä JT, Koski I, Mattila K, Aho AJ et al (2009) Bioactive glass and autogenous bone as a bone graft substitutes in benign bone tumors. J Biomed Mater Res B Appl Biomater 90:131–136
Leppäranta O, Vaahtio M, Peltola T et al (2008) Antibacterial effect of bioactive glasses on clinically important anaerobic bacteria in vitro. J Mater Sci Mater Med. 19:547–551
Munukka E, Leppäranta O, Korkeamäki M et al (2008) Bactericidial effects of bioactive glasses on clinically important aerobic bacteria. J Mater Sci Mater Med. 19:27–32
Hulbert SF, Young FA, Mathews RS et al (1970) Potential of ceramic materials as permanently implantable skeletal prostheses. J Biomed Mater Res 4:433–456
Klawitter JJ, Bagwell JG, Weinstein AM, Sauer BW (1976) An evaluation of bone ingrowth into porous high density polyethylene. J Biomed Mater Res 10:311–319
Vallittu PK, Ruyter IE, Buykuilmaz S (1998) Polymerization time and temperature effects the residual monomer content of denture base polymers. Eur J Oral Sci 106:588–593
Viljanen EK, Skrifvars M, Vallittu PK (2004) Degree of conversion of an experimental monomer and methyl methacrylate copolymer for dental applications. J Appl Polym Sci 93:1908–1912
Hsu W, Feeley BT, Krenek L et al (2007) The use of 18F-fluoride and 18F-FDG PET scans to assess fracture healing in a rat femur model. Eur J Nucl Med Mol Imaging 34:1291–1301
Ullmark G, Sörensen J, Nilsson O (2009) Bone healing of severe acetabular defects after revision arthroplasty. Acta Orthop 80:170–183
Heikkilä JT, Aho AJ, Kangasniemi I et al (1996) Polymethylmetacrylate composites: disturbed bone formation at the surface of bioactive glass and hydroxylapatite. Biomaterials 18:1755–1760
Saha S, Pal S (1984) Mechanical properties of bone cement: a review. J Biomed Mater Res 18:435–462
Ginebra MP, Gil FX, Plaanell JA et al (1996) Relationship between morphology of PMMA particles and properties of acrylic bone cements. J Mater Sci Mater Med 7:375–379
Vallittu PK, Miettinen V, Alakuijala P (1995) Residual monomer content and release into water of denture polymethyl methacrylate. Dent Mater 11:338–342
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Peltola, M.J., Vallittu, P.K., Vuorinen, V. et al. Novel composite implant in craniofacial bone reconstruction. Eur Arch Otorhinolaryngol 269, 623–628 (2012). https://doi.org/10.1007/s00405-011-1607-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1607-x