Abstract
Introduction and hypothesis
The current literature on pelvic organ prolapse (POP) employs wildly varying definitions of surgical success. Understanding which definitions of success have been used and how these may impact reported outcomes is critical. Therefore, we performed a systematic review to identify and summarize these definitions and how they have changed over time.
Materials and methods
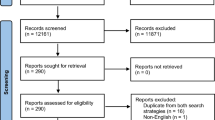
A PubMed search was performed for studies reporting POP surgical outcomes (1996 and later). Inclusion criteria were: original research, English, adult women with POP, nonobliterative surgical treatment, comparison group, reported prolapse-specific outcomes, and clear definition of treatment success. This definition was categorized according to presence of anatomic, subjective, retreatment, or other components and whether these components were evaluated individually or in a composite definition (in which all components must be present for success).
Results
One-hundred forty articles were included. The number of included studies increased over time (r = 0.90, p < 0.00001). Ninety-five studies (67.9%) reported an anatomic-only definition of success, 43 (30.7%) included a subjective component to their definition of success, and 23 (16.4%) reported a composite definition of success, including 11 (7.9%) containing anatomic, symptomatic, and retreatment components. The most common definition of anatomic success was Pelvic Organ Prolapse Quantification (POP-Q) stage ≤ 1. The report of a significant difference between treatment groups (positive study) was most common in studies using an anatomic-only definition of success (p = 0.037).
Conclusion
The number of comparative studies evaluating POP surgical outcomes has increased from 1996 to 2016. Most use definitions of success based solely on anatomic criteria despite increasing awareness of the importance of reporting subjective outcomes and retreatment rates.


Similar content being viewed by others
References
Maher C. ICI 2012: pelvic organ prolapse surgery. Int Urogynecol J. 2013;24(11):1781.
Wu JM, et al. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Colombo M, et al. Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse. BJOG. 2000;107(4):544–51.
Barber MD, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9.
Weber AM, et al. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185(6):1299–304. discussion 1304-6
Chmielewski L, et al. Reanalysis of a randomized trial of 3 techniques of anterior colporrhaphy using clinically relevant definitions of success. Am J Obstet Gynecol. 2011;205(1):69.e1–8.
Bump RC, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–90.
Meister MR,Sutcliffe S, Lowder JL. Definitions of apical vaginal support loss: a systematic review. Am J Obstet Gynecol. 2016.
Toozs-Hobson P, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Int Urogynecol J. 2012;23(5):527–35.
Kowalski JT et al. Do patient characteristics impact the relationship between anatomic prolapse and vaginal bulge symptoms? Int Urogynecol J. 2016.
Bradley CS, et al. Vaginal descent and pelvic floor symptoms in postmenopausal women: a longitudinal study. Obstet Gynecol. 2008;111(5):1148–53.
Menefee SA, et al. Colporrhaphy compared with mesh or graft-reinforced vaginal paravaginal repair for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol. 2011;118(6):1337–44.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Kowalski, J.T., Mehr, A., Cohen, E. et al. Systematic review of definitions for success in pelvic organ prolapse surgery. Int Urogynecol J 29, 1697–1704 (2018). https://doi.org/10.1007/s00192-018-3755-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3755-7