Abstract
Purpose
In the subgroup of patients with Simplified Acute Physiology Score (SAPS) II > 53 in the Stress Ulcer Prophylaxis in Intensive Care Unit (SUP-ICU) trial, there was interaction (P = 0.049) suggesting increased mortality in patients allocated to pantoprazole as compared with placebo. We aimed to explore this further.
Methods
The SUP-ICU trial allocated acutely admitted adults at risk of gastrointestinal bleeding to pantoprazole vs placebo. In this post hoc study, we repeated all the preplanned analyses of SUP-ICU in patients with baseline SAPS II > 53.
Results
A total of 1140 patients had a complete SAPS II > 53 and were included. At 90 days, 272/579 patients (47%) assigned to pantoprazole had died, as compared with 229/558 patients (41%) assigned to placebo [relative risk 1.13; 95% confidence interval (CI) 1.00–1.29]. This was supported by sensitivity analyses adjusted for risk factors and those in the per-protocol population. When accounting for patients with incomplete SAPS II in two additional analyses, the relative risk was 1.08; 95% CI 0.96–1.22 and 1.10; 95% CI 0.97–1.25. This was also observed for the secondary outcome days alive without life support. There were no differences between the intervention groups in the other secondary outcomes.
Conclusions
In this post hoc analysis of patients with high disease severity included in the SUP-ICU trial, we observed higher 90-day mortality and fewer days alive without life support with pantoprazole vs placebo. Some of this may have been explained by missing SAPS II data, but further research is needed to draw firm conclusions.
ClinicalTrials.gov
ClinicalTrials.gov No. NCT02467621.
Similar content being viewed by others
In this post-hoc analysis of a predefined subgroup population in the Stress Ulcer Prophylaxis in the Intensive Care Unit (SUP-ICU) trial, we observed higher 90-day mortality and fewer days alive without the use of life support in patients with a complete Simplified Acute Physiology Score (SAPS) II > 53 points allocated to pantoprazole. We found no explanations for these observations in baseline data, process variables or the other trial outcome measures–however, missing SAPS II data for some patients seem to explain a part of the observed difference. |
Introduction
Critically ill patients in the intensive care unit (ICU) are at risk of developing clinically important gastrointestinal (GI) bleeding due to stress ulcers [1,2,3]. GI bleeding in critically ill patients has been suggested to be associated with adverse outcomes, including a 2–4-fold increased risk of death and increased length of ICU stay [3]. To prevent GI bleeding, stress ulcer prophylaxis is currently recommended in international guidelines [4] and acid suppressants are frequently used in ICU patients [2, 5].
In the international Stress Ulcer Prophylaxis in the Intensive Care Unit (SUP-ICU) trial, 3350 patients at risk of GI bleeding were randomised to receive either pantoprazole or placebo during the ICU stay [1]. We observed no difference between the pantoprazole and placebo groups in the primary outcome measure—90-day mortality—but a predefined subgroup analysis suggested higher 90-day mortality in the pantoprazole group among patients who had higher baseline disease severity, i.e., Simplified Acute Physiology Score (SAPS) II > 53 points (test of interaction, p value 0.049) [6, 7]. This warrants further investigation, because it may be a chance finding or driven by baseline imbalance or differences in withdrawals or follow-up in the subgroup, or missing data for SAPS II elements in some patients.
In this post hoc study of the SUP-ICU trial, we performed the full set of preplanned outcome analyses in all patients with baseline SAPS II > 53 allocated to pantoprazole or placebo on all trial outcomes to search for explanations to substantiate or refute the suggested harm from pantoprazole in the most severely ill. We hypothesised that the increased 90-day mortality observed in patients with SAPS II > 53 allocated to pantoprazole would be substantiated in sensitivity analyses and in those of the remaining outcomes.
Methods
Study oversight
This study is a post hoc analysis of the SUP-ICU trial [7]. The trial protocol, statistical analysis plan and primary results have been published elsewhere [1, 7, 8]. The SUP-ICU trial was approved by all relevant institutions prior to randomisation of the first patient. No additional approvals were required for this study. We have prepared this manuscript according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [9], and the filled-in checklist is available in the Electronic Supplementary Material (ESM).
The SUP-ICU trial
The SUP-ICU trial was a randomised, multicenter, stratified, parallel-group, placebo-controlled, blinded clinical trial recruiting 3350 patients (3291 were available for data analyses) at risk for GI bleeding in 33 ICUs in Denmark, Finland, Norway, Switzerland, the Netherlands and UK from 4 January 2016 to 22 October 2017 [7]. Eligible subjects were patients aged 18 years or older, who were acutely admitted to the ICU and had at least one risk factor for clinically important GI bleeding, including any history of liver disease, any history of or ongoing coagulopathy, shock, or use of anticoagulant agents, renal replacement therapy, or mechanical ventilation expected to last > 24 h [1].
We excluded patients with GI bleeding during current hospital admission, ongoing daily treatment with acid suppressants, patients who were withdrawn from active treatment or brain dead, had organ transplantation during current hospital admission, had peptic ulcer confirmed by endoscopy or other method during current hospital admission, had a contraindication to pantoprazole, were pregnant or where consent for enrolment could not be obtained. The full definitions of the inclusion and exclusion criteria are presented in the ESM.
Patients were randomly assigned to daily intravenous pantoprazole 40 mg or a matching placebo during the ICU stay. Randomisation was stratified according to the presence or absence of hematological malignancy and trial site. The intervention period lasted until discharge from the ICU to a maximum of 90 days. The protocol was reinitiated in case of readmissions to trial ICUs within this period. Apart from the use of stress ulcer prophylaxis, all other parts of patient care were at the discretion of the clinicians.
At baseline we collected data on demographics and clinical characteristics. Daily recordings during the entire admission to the ICU included GI bleeding events, infectious adverse events (pneumonia and Clostridium difficile infection) and data on the usage of life support modalities. Time of death was registered for all patients at a maximum follow-up of 90 days. Observations for GI bleeding and infectious adverse events stopped at the time of discharge from the ICU.
Informed consent was obtained prior to randomisation from all participants or their legal substitutes according to national legislation.
Outcomes
The primary outcome was 90-day mortality. Secondary outcomes were the proportion of patients with clinically important events (a composite outcome of clinically significant GI bleeding, pneumonia, Clostridium difficile infection and myocardial ischemia), clinically important GI bleeding, infectious adverse events (pneumonia or Clostridium difficile infection) and serious adverse reactions (SARs) and the percentage of days alive without the use of life support (mechanical ventilation, renal replacement therapy or inotropes/vasopressor) [1].
Definitions
Clinically important GI bleeding was defined as overt GI bleeding and at least one of the following four features within 24 h of the bleeding episode, in the absence of other causes, in the ICU: (1) a spontaneous drop of systolic blood pressure, mean arterial pressure or diastolic blood pressure of 20 mmHg or more, (2) start of a vasopressor or a 20% increase in vasopressor dose, (3) decrease in hemoglobin of at least 2 g/dl (1.24 mmol/l), or (4) transfusion of two or more units of packed red blood cells [1]. The full definitions of the other outcomes are presented in the ESM.
Statistical analyses
We repeated all predefined analyses on all outcomes and in all predefined subgroups according to the published SUP-ICU trial statistical analysis plan [8] in this subgroup of patients with baseline SAPS II > 53. The SAPS II score is calculated from 17 variables with a total range from 0 to 163 points; higher scores indicating greater severity of disease (Table S7 in the ESM). Fifty-three points was chosen a priori as the cut-off for the subgroup analysis, as it was found to predict a 50% mortality rate in the original model [6] and similar cut-offs have been used previously [10].
In brief, we conducted the primary analyses in the intention-to-treat population. In the primary analyses, we compared data in the two treatment groups by binary logistic regression analysis adjusted for the stratification variables (trial site and active hematological malignancy); relative risks with 95% confidence intervals were computed from odds ratios [8]. In a sensitivity analysis, we compared the primary outcome in the per-protocol population (excluding patients having one or more major protocol violations—definition in ESM), and in the originally pre-specified subgroups, defined by the presence or absence of any history of liver disease, the presence or absence of any history of or ongoing coagulopathy, the type of ICU admission (medical versus surgical), the presence or absence of shock and the use or not of mechanical ventilation [8].
In the secondary analyses, we compared all dichotomous outcomes using binary logistic regression analyses adjusted for stratification variables and predefined risk factors at baseline (age, type of admission (medical, elective surgery or emergency surgery) and the Sepsis-related Organ Failure Assessment (SOFA) score (Table S8 in the ESM) assessed in the 24 h before randomisation). We analysed percentages of days alive without life support in the 90-day period by use of the van Elteren test (adjusted for site only), as the assumptions for Poisson or negative binomial distributions were not met [11]. We performed no adjustment for multiple comparisons and reported results as point estimates with 95% confidence intervals.
To account for the between-group imbalance in coagulopathy, we conducted a post hoc sensitivity analysis in which we included coagulopathy in the adjusted (secondary) binary logistic regression model.
As the proportion of patients with incomplete SAPS II could be of importance, we conducted the following two post hoc sensitivity analyses (of all outcomes): (1) patients with missing SAPS II who could potentially have had SAPS II > 53 were included (assigning the worst possible SAPS II sub-score, when missing, and then re-calculating the total SAPS II). An additional 169/249 patients with missing SAPS II were included in this sensitivity analysis; and (2) patients with missing SAPS II who after computer-generated single-imputation of missing SAPS II sub-scores had a SAPS II > 53 were included. The single-imputation approach was repeated three times to assess random variation and showed consistency. An additional 106/249 patients with missing SAPS II were included in this sensitivity analysis.
In the complete-case population, nine patients were lost to 90-day follow-up in the full trial population, of which three had a SAPS II > 53. Accordingly, complete-case analysis was the main primary outcome analysis. Additional details on handling of missing data, including sensitivity analyses with imputation of SAPS II values are provided in the ESM.
All analyses were performed using SAS software, version 9.4, and R software, version 3.4.3.
Results
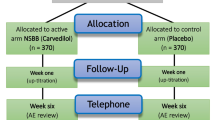
A total of 1140 patients had complete SAPS II > 53 at baseline; 580 assigned to pantoprazole and 560 assigned to placebo. Besides excluding patients with SAPS II ≤ 53, we excluded 249/3291 patients (7.6%) with incomplete SAPS II (Fig. 1). Ninety-day vital status was obtained for 1137 of 1140 patients (99.5%), including 579 in the pantoprazole group and 558 in the placebo group (Fig. 1). Patient characteristics at baseline appeared similar in the two groups, except for coagulopathy (Table 1).
Randomisation and follow-up. The list of reasons for exclusions in the SUP-ICU trial was presented in the main publication of the SUP-ICU trial. In brief, 52 patients were originally excluded immediately after randomisation prior to the first dose of trial medication because they did not meet the inclusion criteria or fulfilled one or more exclusion criteria. A total of seven patients were excluded after randomisation because the patient or their surrogate did not allow the use of the data. The applied dotted-line square marks the population for this post hoc analysis of patients with high baseline disease severity (SAPS II > 53). A total of 249 patients, 134 in the pantoprazole and 115 in the placebo group, had missing data for one or more of the SAPS II elements and therefore an incomplete SAPS II. These were excluded from the main analysis, but they were included in sensitivity analyses with the missing data imputed. Of the 1140 patients with a baseline SAPS II > 53, one patient was lost for 90-day follow-up in the pantoprazole group and two patients in the placebo group
Outcomes
At 90 days after randomisation, 272 of 579 patients (47.0%) in the pantoprazole group and 229 of 558 (41.0%) in the placebo group had died (relative risk, 1.13; 95% confidence interval 1.00–1.29) (Table 2 and Fig. 2). The results were consistent in the sensitivity analysis adjusted for baseline risk factors (relative risk, 1.14; 95% confidence interval 0.99–1.30), in the per-protocol population (relative risk, 1.17; 95% confidence interval 1.01–1.37) (Table 2), and in the post hoc sensitivity analysis with adjustment for coagulopathy at baseline estimates (relative risk, 1.14; 95% confidence interval 0.99–1.30). In the predefined subgroup analyses, we observed no heterogeneity in the effect of pantoprazole versus placebo on mortality at 90 days (Fig. 2).
Time to death and relative risk of death at day 90 in the complete-case population. Part A shows the survival curves censored at day 90 for the two groups in the intention-to-treat population. Part B shows relative risks (RRs) with 95% confidence intervals (CI) for the primary outcome measure of death at day 90 in the pantoprazole group compared with the placebo group in all patients with complete SAPS II > 53 and in the five additional pre-defined subgroups assessed by logistic regression analysis adjusted for stratification variables. For the definition of shock, coagulopathy, and history of liver disease, at baseline, please see the ESM (inclusion criteria). Note that the coagulopathy subgroup included both acute coagulopathy and history of coagulopathy. Medical admission was when no surgery was performed for at least 1 week prior to ICU admission
Some 146 of 580 patients (25.2%) in the pantoprazole group, as compared with 147 of 560 patients (26.3%) in the placebo group, had one or more clinically important events in the ICU (relative risk, 0.93; 95% confidence interval 0.75–1.16) (Table 2). Fewer patients in the pantoprazole group had clinically important GI bleeding; 19 of 580 (3.3%) and 34 of 560 (6.1%) in the pantoprazole and placebo groups, respectively, (relative risk, 0.49; 95% confidence interval 0.29–0.86). The percentage of days alive without the use of life support was 81% (interquartile range 9–95) and 85% (interquartile range 36–96), in the pantoprazole and placebo groups (P = 0.02), respectively. The remaining secondary outcomes and the remaining single components of the composite outcome were similar between the two groups (Table 2 and Table S1 in the ESM).
In the two post hoc sensitivity analysis accounting for missing SAPS II values (using a logically imputed and a single-imputed SAPS II > 53 population), 299 of 667 patients (44.8%) in the pantoprazole group and 264 of 639 (41.3%) in the placebo group had died (relative risk, 1.08; 95% confidence interval 0.96–1.22), and 292 of 636 patients (45.9%) in the pantoprazole group and 253 of 607 (41.7%) in the placebo group had died (relative risk, 1.10; 95% confidence interval 0.97–1.24), respectively (Table S2 and S3 in the ESM). This was consistent in the secondary analyses of these two populations (Table S2–S6 in the ESM).
Discussion
In this post hoc exploratory analysis of the SUP-ICU trial, we found higher 90-day mortality and a lower percentage of days alive without use of life support in ICU patients at risk of GI bleeding with baseline SAPS II > 53 who were assigned to pantoprazole compared with those assigned to placebo in the primary complete-case population. These findings did not appear to be explained by baseline imbalance or differences in withdrawals or follow-up in this subgroup, but missing SAPS II values in the original trial cohort may have explained some of these findings.
We conducted this study because one of the predefined subgroup analyses in the SUP-ICU trial main analysis suggested higher 90-day mortality in the pantoprazole group among patients who had SAPS II > 53 points (test of interaction, p-value 0.049) [7]. We may have explained some of this sub-group effect as per the sensitivity analyses estimating the effect of missing data, but 8–10% relative risk increase in mortality with pantoprazol remains unexplained. This is likely to be important to patients, relatives and health care professionals.
Most findings were consistent with the findings of the analyses of the full trial population, as neither GI bleeding, infections nor myocardial ischemia explained the potential subgroup effect.
To our knowledge it is rare to observe a potentially heterogenous intervention effect depending on baseline severity of disease in ICU trials [12], and this has not previously been suggested (or investigated) for pantoprazole [13,14,15,16]. A priori, it could be speculated that patients with the highest severity of disease are at the greatest risk of adverse events and/or tolerate side effects poorly, e.g., due to more frailty, or organ failure, or perhaps these patients constitute a different phenotype to patients with less severity of disease. An association between use of proton pump inhibitors and cardiovascular events, e.g., myocardial ischemia and stroke has previously been suggested [17,18,19], however, a causal relation, and adverse cardiovascular effects of short-term use in high disease severity ICU patients remains unconfirmed.
More patients had coagulopathy at baseline in the pantoprazole group, however this did not affect the risk estimate of mortality in the included post hoc sensitivity analysis or the risk of clinically important GI bleeding (Table 2).
In general, subgroup analyses of randomised clinical trials are prone to type 1 and 2 errors and are therefore often misleading [20, 21], and criteria to evaluate the credibility of subgroup analyses have been suggested [22, 23]. According to these criteria, the following aspects weaken the case for the suggested subgroup finding: the randomisation was not stratified for SAPS II being greater than 53 respectively lesser than or equal to 53, inconsistency between our hypothesised subgroup effect direction (as pre-specified in the trial protocol [1]) and the actually observed effect direction [7], and the observed lower limit of the 95% confidence interval close to 1.00 (imprecision) [23].
The limitations of this study include the post hoc design resulting in increased risk of attrition and detection bias [24]. However, the analyses were conducted in accordance with the predefined analyses of the main trial population [8]. As in the analyses of the full trial population, we excluded patients with missing SAPS II in the primary analysis of this study. Patients with SAPS II > 53 constituted only around a third of the full SUP-ICU trial population with resulting lower statistical power and increased risk of type 1 and 2 errors. The cut-off of SAPS II at 53 points can be debated. This cut-off represents a predicted mortality rate of 50% in the original model from 1993 [6], however, this is no longer the case due to improved ICU survival rates. Presumably it would now represent a predicted mortality of around 25% [25]. Whether other cut-offs would have yielded different results is unknown. Also, baseline imbalance may have affected results, even though additionally adjusting for coagulopathy did not change the estimates. Finally, we refrained from using multiple imputation to impute the missing SAPS II elements for sensitivity analysis as the large number of resulting populations with variations in sizes for subsequent analyses would be nearly impossible to account for and communicate clearly.
The strengths of this study include the fact that it is based on a large randomised trial with low risk of bias and that analyses were conducted according to the original statistical analysis plan, both reducing the risk of selection bias.
A recent editorial in the New England Journal of Medicine suggested that proton pump inhibitor prophylaxis may benefit the sickest ICU patients [26]. We do believe that our findings warrant further assessment and replication in randomised trials and meta-analyses with low risk of bias. We may also learn more from the pre-planned analyses of 1-year mortality after randomisation in all SUP-ICU trial patients and in the subgroups [1].
In conclusion, we found higher 90-day mortality and a lower percentage of days alive without the use of life support in the primary analysis in this post hoc investigation of ICU patients at risk of GI bleeding with complete baseline SAPS II > 53 assigned to pantoprazole versus placebo. Some of this may have been explained by missing SAPS II data in the full SUP-ICU trial cohort, but further research is needed to draw firm conclusions.
References
Krag M, Perner A, Wetterslev J et al (2016) Stress ulcer prophylaxis with a proton pump inhibitor versus placebo in critically ill patients (SUP-ICU trial): study protocol for a randomised controlled trial. Trials 17:205
Krag M, Perner A, Wetterslev J et al (2015) Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med 41:833–845
Cook DJ, Griffith LE, Walter SD et al (2001) The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients. Crit Care 5:368–375
Rhodes A, Evans LE, Alhazzani W et al (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Krag M, Perner A, Wetterslev J et al (2015) Stress ulcer prophylaxis in the intensive care unit: an international survey of 97 units in 11 countries. Acta Anaesthesiol Scand 59:576–585
Le Gall J-R, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American Multicenter Study. JAMA 270:2957
Krag M, Marker S, Perner A et al (2018) Pantoprazole in patients at risk for gastrointestinal bleeding in the ICU. N Engl J Med 379:2199–2208
Krag M, Perner A, Wetterslev J et al (2017) Stress ulcer prophylaxis in the intensive care unit trial: detailed statistical analysis plan. Acta Anaesthesiol Scand 61:859–868
von Elm E, Egger M, Altman DG et al (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335:806–808
Holst LB, Haase N, Wetterslev J et al (2014) Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med 371:1381–1391
Jakobsen JC, Tamborrino M, Winkel P et al (2015) Count data analysis in randomised clinical trials. J Biomet Biostat 6:227
Macias WL, Nelson DR, Williams M et al (2005) Lack of evidence for qualitative treatment by disease severity interactions in clinical studies of severe sepsis. Crit Care 9:R607–R622
Alhazzani W, Guyatt G, Alshahrani M et al (2017) Withholding pantoprazole for stress ulcer prophylaxis in critically ill patients: a pilot randomized clinical trial and meta-analysis. Crit Care Med 45:1121–1129
Alhazzani W, Alshamsi F, Belley-Cote E et al (2018) Efficacy and safety of stress ulcer prophylaxis in critically ill patients: a network meta-analysis of randomized trials. Intensive Care Med 44:1–11
Cook D, Guyatt G (2018) Prophylaxis against upper gastrointestinal bleeding in hospitalized patients. N Engl J Med 378:2506–2516
Selvanderan SP, Summers MJ, Finnis ME et al (2016) Pantoprazole or placebo for stress ulcer prophylaxis (POP-UP). Crit Care Med 44:1842–1850
MacLaren R, Reynolds PM, Allen RR (2014) Histamine-2 receptor antagonists vs proton pump inhibitors on gastrointestinal tract hemorrhage and infectious complications in the intensive care unit. JAMA Intern Med 174:564–574
Charlot M, Ahlehoff O, Norgaard ML et al (2010) Proton-pump inhibitors are associated with increased cardiovascular risk independent of clopidogrel use: a nationwide cohort study. Ann Intern Med 153:378–386
Sehested TSG, Gerds TA, Fosbøl EL et al (2018) Long-term use of proton pump inhibitors, dose-response relationship, and associated risk of ischemic stroke and myocardial infarction. J Intern Med 283:268–281
Sedgwick P (2014) Randomised controlled trials: subgroup analyses. BMJ 349:g7513
Wang R, Lagakos SW, Ware JH et al (2007) Statistics in medicine—reporting of subgroup analyses in clinical trials. N Engl J Med 357:2189–2194
Oxman AD, Guyatt GH (1992) A consumer’s guide to subgroup analyses. Ann Intern Med 116:78–84
Sun X, Briel M, Walter SD, Guyatt GH (2010) Is a subgroup effect believable? Updating criteria to evaluate the credibility of subgroup analyses. BMJ 340:850–854
Higgins JPT, Altman DG, Gotzsche PC et al (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Granholm A, Møller MH, Krag M et al (2016) Predictive performance of the simplified acute physiology score (SAPS) II and the initial sequential organ failure assessment (SOFA) score in acutely ill intensive care patients: post-hoc analyses of the SUP-ICU inception cohort study. PLoS One 11:e0168948
Barkun A, Bardou M (2018) Proton-pump inhibitor prophylaxis in the ICU—benefits worth the risks? N Engl J Med 379:2263–2264
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710
Acknowledgements
All authors were involved in the conduct of the SUP-ICU trial. The authors thank everybody involved in the SUP-ICU trial: research staff and investigators, clinical staff, patients and their relatives.
Funding
The authors have received no specific funding for this study. The SUP-ICU trial was funded by Innovation Fund Denmark (4108-00011A) and supported by Rigshospitalet, the Capital Region of Denmark, the Regions of Denmark, the Scandinavian Society of Anaesthesiology and Intensive Care Medicine, Ehrenreich’s Foundation, Aase and Ejnar Danielsens Foundation, the Danish Society of Anaesthesiology and Intensive Care Medicine, the Danish Medical Association and the European Society of Intensive Care Medicine. The Department of Intensive Care at Rigshospitalet has received support for other research projects from Fresenius Kabi, Germany; CSL Behring, Switzerland; Ferring Pharmaceuticals, Denmark; and the Novo Nordisk Foundation, Denmark. The SUP-ICU trial was funded by Innovation Fund Denmark and others.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
None for the present study. The Department of Intensive Care at Rigshospitalet receives support for other research projects from Fresenius Kabi, Germany; CSL Behring, Switzerland; Ferring Pharmaceuticals, Denmark; and the Novo Nordisk Foundation, Denmark. The authors report no conflicts of interest. All authors were involved in the conduct of the SUP-ICU trial.
Ethical approval
No additional approvals were needed for this post hoc sub-analysis of the SUP-ICU trial. All procedures in the SUP-ICU trial were performed in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Marker, S., Perner, A., Wetterslev, J. et al. Pantoprazole prophylaxis in ICU patients with high severity of disease: a post hoc analysis of the placebo-controlled SUP-ICU trial. Intensive Care Med 45, 609–618 (2019). https://doi.org/10.1007/s00134-019-05589-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05589-y