Abstract
Purpose
The aim of this study was to examine the effects of intravenous (IV) fluid restriction on time to resolution of hyperlactatemia in septic shock. Hyperlactatemia in sepsis is associated with worse outcome. Sepsis guidelines suggest targeting lactate clearance to guide fluid therapy despite the complexity of hyperlactatemia and the potential harm of fluid overload.
Methods
We conducted a post hoc analysis of serial plasma lactate concentrations in a sub-cohort of 777 patients from the international multicenter clinical CLASSIC trial (restriction of intravenous fluids in intensive care unit (ICU) patients with septic shock). Adult ICU patients with septic shock had been randomized to restrictive (n = 385) or standard (n = 392) intravenous fluid therapy. The primary outcome, time to resolution of hyperlactatemia, was analyzed with a competing-risks regression model. Death and discharge were competing outcomes, and administrative censoring was imposed 72 h after randomization if hyperlactatemia persisted. The regression analysis was adjusted for the same stratification variables and covariates as in the original CLASSIC trial analysis.
Results
The hazard ratios (HRs) for the cumulative probability of resolution of hyperlactatemia, in the restrictive vs the standard group, in the unadjusted analysis, with time split, were 0.94 (confidence interval (CI) 0.78–1.14) at day 1 and 1.21 (0.89–1.65) at day 2–3. The adjusted analyses were consistent with the unadjusted results.
Conclusion
In this post hoc retrospective analysis of a multicenter randomized controlled trial (RCT), a restrictive intravenous fluid strategy did not seem to affect the time to resolution of hyperlactatemia in adult ICU patients with septic shock.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this retrospective analysis, a restrictive intravenous fluid therapy strategy did not seem to affect time to resolution of hyperlactatemia in intensive care unit patients treated for septic shock. |
Introduction
In patients with sepsis, hyperlactatemia is associated with increased mortality and morbidity [1]. Traditionally, hyperlactatemia has been viewed as a marker of hypoperfusion leading to tissue hypoxia. But adrenergic stress response, increased glycolysis, liver dysfunction/failure, and certain concomitant medication use have also been shown to increase plasma lactate levels [2, 3]. Current sepsis guidelines suggest guiding resuscitation to decrease lactate in patients with elevated lactate level [4], implying that this should be the goal for ongoing management including vasopressors and fluid therapy despite the complexity of hyperlactatemia [5,6,7] and the potential harm of fluid overload [8].
In this post hoc retrospective analysis, we aimed to investigate how fluid treatment strategy affects lactate concentrations. We hypothesized, due to the poor specificity of lactate for hypoperfusion, that a restrictive approach would not significantly affect the time to resolution of hyperlactatemia in septic shock. Further, as an initial lactate level ≥ 4 mmol/L is associated with a markedly increased mortality in patients with sepsis [9], we hypothesized that lactate clearance would be different in this subgroup of more severely deranged patients.
Methods
Study design
This secondary post hoc analysis of the CLASSIC multicenter trial was registered at clinicaltrials.gov (NCT05629780), published prior to conduct of the analyses but after the main CLASSIC trial results were published.
Setting and participants
CLASSIC (The European Clinical Trials Database 2018-000404-42, ClinicalTrials.gov NCT03668236) was an European, stratified, parallel-group, open-label randomized clinical trial, investigating whether a restrictive approach to intravenous (IV) fluid therapy compared to a standard care strategy would result in fewer deaths on day 90 [10]. The 1554 participants were enrolled in 31 intensive care units (ICUs) in Denmark, Norway, Sweden, Switzerland, Italy, the Czech Republic, the United Kingdom and Belgium between November 2018 and November 2021. Adult patients fulfilling criteria for septic shock (according to Sepsis-3 criteria) [11] were eligible if onset was within 12 h and at least 1 L of IV fluids had been administered within 24 h prior to screening. The participants were randomly assigned 1:1 to restricted IV fluid or standard IV fluid therapy during their ICU stay for a maximum of 90 days. Additional details on the CLASSIC trial, inclusion and exclusion criteria with full definitions, trial interventions and results after 90 days and 1 year, are available elsewhere [10, 12, 13].
The analysis was conducted on a subset of 777 out of the 1554 patients originally included in the CLASSIC trial. The cohort consisted of all Swedish, all Czech, and all Danish patients from the Capital and Zealand regions. Five Danish patients had withdrawn their previous consent to participate in the CLASSIC study and one Czech patient had no recorded lactate concentration. These patients were excluded from our analyses (Fig. 1).
Ethical considerations
Ethical approval was ensured through amendments to the original ethical applications for CLASSIC in Sweden, Denmark and the Czech Republic (Etikprövningsmyndigheten, Sverige, Diarie-Nr 2021-06283-02, De videnskapsetiske komiteer, Centrum for Sundhed, Danmark Journal-Nr H-18006255 and Ethical Committee University Hospital Pilsen, Charles University, Czech Republic Reference Nr 473/2021). The original patient consent declarations were deemed sufficient by all ethics committees.
Data sources
We retrospectively collected, from patients’ health records, all available point-of-care blood gas analyses of lactate within the first 72 h after randomization, until death, or discharge from the ICU. Consecutive plasma lactate measurements were not included in the CLASSIC trial protocol [10], so the number of available recorded plasma lactate values varied across patients and sites due to practice variation.
The full baseline patient characteristics of the cohort (age, sex, previous comorbidities (hematological or metastatic cancer, ischemic heart disease, chronic hypertension and long-term dialysis), time from hospital/ICU admission to randomization, simplified mortality score for the intensive care unit (SMS-ICU) [14] and corresponding predicted 90-day mortality, source of ICU admission, focus of infection, bodyweight, highest plasma lactate concentration, highest dose of norepinephrine, volume of IV fluid 24 h before randomization, use of systemic corticosteroids, highest creatinine concentration, and use of respiratory support) were collected from the CLASSIC database. Descriptive data are summarized as medians with interquartile ranges (IQRs) for numerical data and as counts (percentages) for categorical data.
Outcome
The primary outcome was the time to resolution of hyperlactatemia, defined as the first recorded plasma lactate concentration < 2 mmol/L within 72 h after randomization, irrespective of subsequent changes.
Statistical analysis
For analysis of the primary outcome, a competing-risks regression model [15] was used. Death and discharge were considered competing outcomes, and administrative censoring was imposed 72 h after randomization if hyperlactatemia persisted.
In line with the primary CLASSIC results, we adjusted the regression analysis for two stratification variables, trial site and presence of hematologic or metastatic malignancy, and for five covariates; the predefined stratification variables, the SMS-ICU [14], focus of infection (urinary tract infection versus other foci), and use of systemic corticosteroids.
An additional analysis was performed for the subgroups of patients with a higher baseline (up to 3 h prior to randomization) plasma lactate concentration of ≥ 4 mmol/L.
The two-sided significance level for the analysis was 5%. All analyses and procurement of graphs were performed using R software, version 4.1.2 (R Foundation for Statistical Computing).
Model assessment
The p test for Schoenfeld residuals did not indicate a violation of the proportional-hazards (PH) assumption (p-value 0.09; see electronic supplementary material (ESM) – Fig. S1) [16]. However, visual inspection of the Schoenfeld residuals plot of the primary analysis indicated potential violations of the assumption. When assessing the cumulative curves, they converged around day 1. Consequently, a time split was introduced to allow different hazard ratios (HRs) before and after day 1. The unexpected potential violation of the PH assumption led to introduction of a time split model. However, since this decision constituted an amendment to the statistical analysis plan, we also present the originally planned analysis for transparency purposes.
For the subgroups of patients with a baseline plasma lactate concentration ≥ 4 mmol/L, the PH assumption was met, so no time split was introduced (p-value = 0.93; see ESM—Fig. S2).
Missing data
All analyses included complete cases only because < 5% of the values were missing in each analysis.
Results
Trial population
We included 777 patients (n = 129 from Sweden, n = 599 from Denmark and n = 49 from the Czech Republic); 385 from the restrictive fluid group and 392 from the standard fluid group. The baseline patient characteristics and fluid intervention volumes are presented in Tables 1 and 2.
The cohort had generally balanced baseline characteristics, but there was a higher prevalence of coexisting ischemic heart disease and/or heart failure in the standard group. There was a high degree of concordance with the baseline characteristics of the CLASSIC patients not included, added for comparison (Table S3) in the ESM.
Intravenous fluid intervention
We extracted a total of 16,674 lactate concentration values (8243 from the restrictive, and 8431 from the standard group). Of these, 93 percent (7631) in the restrictive, and 91 percent (7713) in the standard group were arterial measurements. A graph, showing all median plasma lactate concentrations in mmol/L, for every hour, with the interquartile range illustrated as a ribbon, in the first 72 h after randomization, is illustrated in Fig. 2.
Top graph: Median plasma lactate concentrations in mmol/L (interpolated to hourly resolution) with the interquartile range illustrated as a ribbon in the first 3 days after randomization in the restrictive fluid (red) and standard fluid (blue) groups (days). Bottom graph: The number of patients within the restrictive fluid (red) and standard fluid (blue) group contributing to the measured lactate values above. Example: The number of patients contributing with lactate values constituted 118 in each group around the eighth hour of the first day
Outcome
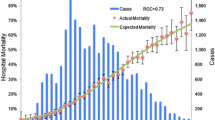
For the primary analysis, there were no statistically significant differences in the cumulative probability for any of the competing outcomes (time to resolution of hyperlactatemia, death, or discharge) between the groups at any of the time points. The adjusted models were consistent with the primary results. The cumulative probabilities for the competing outcomes are presented in a graph and in a table with HRs and corresponding 95% confidence intervals (CIs) (Fig. 3 and Table 3). A HR < 1 indicates a lower cumulative probability of resolution of hyperlactatemia, death, or discharge in the intervention (restrictive) group, and vice versa.
In addition, we repeated the analysis in the subgroup of patients with a higher plasma lactate concentration at baseline (≥ 4 mmol/L). There were no significant differences between the restrictive and standard care groups, and the adjusted models yielded similar results (Table 4). The baseline characteristics and the fluid volumes for the subgroup analysis stratified by baseline lactate concentrations are presented in separate tables (supplementary Tables S1 and S2) in the ESM.
Discussion
In this post hoc analysis of adult patients with septic shock in the ICU, randomized to either restricted or standard fluid therapy, we observed no statistically significant differences in the time to resolution of hyperlactatemia, or any of the competing outcomes, between the groups during the first 72 h after randomization. This result aligns with the post hoc analysis of plasma lactate levels during 24 h from the CLASSIC feasibility trial [17, 18], and strengthens the primary CLASSIC trial result.
While acknowledging that these retrospective analyses are hypothesis generating, this finding might be contradictory to many clinicians’ belief that the mainstay treatment for hyperlactatemia in septic shock consists of fluid therapy.
Lactate could seem to be the ideal biomarker for critically ill patients, given its strong association with morbidity and mortality. Both sepsis-associated hyperlactatemia (isolated high values) and delayed resolution of elevated lactate have been associated with unfavorable outcomes [19, 20]. Elevated early lactate levels were significantly associated with increased mortality (odds ratio (OR) 2.92 CI 2.40–3.55 p < 0.00001) in a meta-analysis by Liu et al. [9].
Serial plasma lactate measurements during early sepsis are valuable warning tools related to prognosis, but the value and implications of monitoring lactate levels beyond 24 h have received less attention [21]. Specifically, a resuscitation strategy targeting lactate clearance might lead to unnecessary fluid replacement, blood transfusion and use of inotropic agents. Plasma lactate concentrations are often used by clinicians to guide fluid therapy, but few randomized studies have evaluated this strategy.
The ANDROMEDA-SHOCK randomized controlled trial (RCT) evaluated two resuscitation endpoint strategies, based on lactate reduction versus normalizing capillary refill time, and a post hoc analysis showed potential worse outcome from the lactate-guided strategy [22, 23]. The patients in the lactate-guided group received more resuscitative interventions and presented more organ dysfunction. In contrast, Jones et al. conducted a RCT in which a strategy to normalize ScvO2 was compared with a strategy to decrease lactate levels by 10% in a 6 h study protocol. The hospital point estimate indicated that mortality was 5% lower in the lactate-guided group, but this difference was not statistically significant [24]. Similarly, in a Dutch multicenter RCT of 348 patients, lactate-guided resuscitation in hyperlactatemia (albeit not limited to sepsis) reduced hospital mortality by nearly 10% when corrected for baseline imbalances. Hyperlactatemia was defined as > 3 mmol/L, and the protocol had the aim to optimize oxygen delivery to decrease lactate levels ≥ 20% every 2 h during the first 8 h after admission [25]. The intervention group received more fluids and vasodilators, but interestingly, there were no significant differences in lactate levels between the groups, indicating that measures aimed at improving perfusion and oxygen delivery do not seem to affect lactate levels per se. The ongoing ANDROMEDA-SHOCK-2 RCT [26] will assess the evolution of lactate levels, in subgroups with baseline lactate < 4 and ≥ 4 mmol/L, as a (tertiary) clinical outcome which may shed some light on the issue in future.
The strengths of this study include the randomized design of the original trial. The patients were recruited from 13 different university and non-university ICUs in three different countries, which makes the results generalizable, at least within Europe. There was a high completeness of the data, minimal loss to follow-up (0.8%) and the trial succeeded in achieving separation in fluids administered via a pre-published protocol [10].
Our study has several limitations. First, the study cohort consists of only half of the 1554 patients included in the original trial. Procurement of plasma lactate values for the whole CLASSIC cohort (5 additional countries) was not possible within the scope of this study. Lactate measurements were not mandated nor reported in the CLASSIC trial and centers participating in this secondary analysis had to complete additional ethical amendments and (sometimes manually) extract lactate values for the participants from their respective study sites and only centers who volunteered to extract and share these data could be included. 777 patients still composed a reasonably large cohort, which is why this pragmatic strategy was chosen. Second, due to the retrospective design of this study, we were limited by the availability of plasma lactate concentrations from the participating sites. In most cases, one would presume that fewer blood gasses are analyzed as the patient improves, and vice versa. Ideally, the samples should be taken at standardized time points or time intervals. Since we were limited to recorded values, the resolution of hyperlactatemia might have occurred earlier than calculated, but the large number of patients and the randomized design of the study partly counteracts this bias. Third, even though there was a clear separation of IV fluid volumes between the two study arms, the differences were small, which increases the risk of a type II error. Finally, in the subgroup with a higher plasma lactate concentration at baseline, where the effect of treatment strategies might have been strongest, there is also a limitation in that a plasma lactate concentration of ≥ 4 mmol/L was a condition allowing for, however not mandating, administration of IV fluid in the restrictive group.
Data availability
For ethical and legal reasons the raw data collected for this study cannot be publicly shared. Aggregated results and statistical summaries are presented in the manuscript and its supplementary materials. Any further inquiries regarding the data may be directed to the corresponding author.
References
Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS et al (2016) Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):775–787
Hernandez G, Bellomo R, Bakker J (2019) The ten pitfalls of lactate clearance in sepsis. Intensive Care Med 45(1):82–85
Bakker J, de Backer D, Hernandez G (2016) Lactate-guided resuscitation saves lives: we are not sure. Intensive Care Med 42(3):472–474
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C et al (2021) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med 49(11):e1063–e1143
Kushimoto S, Akaishi S, Sato T, Nomura R, Fujita M, Kudo D et al (2016) Lactate, a useful marker for disease mortality and severity but an unreliable marker of tissue hypoxia/hypoperfusion in critically ill patients. Acute Med Surg 3(4):293–297
Bloos F, Zhang Z, Boulain T (2016) Lactate-guided resuscitation saves lives: yes. Intensive Care Med 42(3):466–469
Monnet X, Delaney A, Barnato A (2016) Lactate-guided resuscitation saves lives: no. Intensive Care Med 42(3):470–471
Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA (2011) Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med 39(2):259–265
Liu G, Haijin L, An Y, Wei X, Yi X, Yi H (2017) Early lactate levels for prediction of mortality in patients with sepsis or septic shock: a meta-analysis. Int J Clin Exp Med 10:37–47
Meyhoff TS, Hjortrup PB, Møller MH, Wetterslev J, Lange T, Kjaer MN et al (2019) Conservative vs liberal fluid therapy in septic shock (CLASSIC) trial-Protocol and statistical analysis plan. Acta Anaesthesiol Scand 63(9):1262–1271
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810
Meyhoff TS, Hjortrup PB, Wetterslev J, Sivapalan P, Laake JH, Cronhjort M et al (2022) Restriction of intravenous fluid in ICU patients with septic shock. N Engl J Med 386(26):2459–2470
Kjær MN, Meyhoff TS, Sivapalan P, Granholm A, Hjortrup PB, Madsen MB et al (2023) Long-term effects of restriction of intravenous fluid in adult ICU patients with septic shock. Intensive Care Med 49(7):820–830
Granholm A, Perner A, Krag M, Hjortrup PB, Haase N, Holst LB et al (2017) Simplified Mortality Score for the Intensive Care Unit (SMS-ICU): protocol for the development and validation of a bedside clinical prediction rule. BMJ Open 7(3):e015339
Haller B, Schmidt G, Ulm K (2013) Applying competing risks regression models: an overview. Lifetime Data Anal 19(1):33–58
Bradburn MJ, Clark TG, Love SB, Altman DG (2003) Survival analysis Part III: multivariate data analysis—choosing a model and assessing its adequacy and fit. Br J Cancer 89(4):605–611
Hjortrup PB, Haase N, Wetterslev J, Lange T, Bundgaard H, Rasmussen BS et al (2017) Effects of fluid restriction on measures of circulatory efficacy in adults with septic shock. Acta Anaesthesiol Scand 61(4):390–398
Hjortrup PB, Haase N, Bundgaard H, Thomsen SL, Winding R, Pettilä V et al (2016) Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med 42(11):1695–1705
Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA et al (2004) Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med 32(8):1637–1642
Arnold RC, Shapiro NI, Jones AE, Schorr C, Pope J, Casner E et al (2009) Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock 32(1):35–39
Chertoff J, Chisum M, Garcia B, Lascano J (2015) Lactate kinetics in sepsis and septic shock: a review of the literature and rationale for further research. J Intensive Care 3:39
Kattan E, Hernández G, Ospina-Tascón G, Valenzuela ED, Bakker J, Castro R (2020) A lactate-targeted resuscitation strategy may be associated with higher mortality in patients with septic shock and normal capillary refill time: a post hoc analysis of the ANDROMEDA-SHOCK study. Ann Intensive Care 10(1):114
Hernández G, Ospina-Tascón GA, Damiani LP, Estenssoro E, Dubin A, Hurtado J et al (2019) Effect of a resuscitation strategy targeting peripheral perfusion status vs serum lactate levels on 28-day mortality among patients with septic shock: the ANDROMEDA-SHOCK randomized clinical trial. JAMA 321(7):654–664
Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA (2010) Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA 303(8):739–746
Jansen TC, van Bommel J, Schoonderbeek FJ, Sleeswijk Visser SJ, van der Klooster JM, Lima AP et al (2010) Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med 182(6):752–761
Kattan E, Bakker J, Estenssoro E, Ospina-Tascón GA, Cavalcanti AB, Backer D et al (2022) Hemodynamic phenotype-based, capillary refill time-targeted resuscitation in early septic shock: The ANDROMEDA-SHOCK-2 Randomized Clinical Trial study protocol. Rev Bras Ter Intensiva 34(1):96–106
Funding
Open access funding provided by Karolinska Institute. The original CLASSIC study was supported by a grant from the Novo Nordisk Foundation and by the Sofus Friis’ Foundation, the Rigshospitalets Research Council and the Danish Society of Anesthesiology and Intensive Care Medicine. This study was supported by grants from Scandinavian Society of Anesthesia and Intensive Care Medicine (SSAI), Stockholm County Council and the Olof Norlander memorial fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ahlstedt, C., Sivapalan, P., Kriz, M. et al. Effects of restrictive fluid therapy on the time to resolution of hyperlactatemia in ICU patients with septic shock. A secondary post hoc analysis of the CLASSIC randomized trial. Intensive Care Med 50, 678–686 (2024). https://doi.org/10.1007/s00134-024-07385-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-024-07385-9