Abstract
Purpose
Whole lung lavage (WLL) pathophysiologically represents a human model of controlled lung de-aeration, resembling various pathological conditions encountered in the critically ill. Through one-lung ventilation and progressive alveolar flooding, it mimics, respectively, re-absorption atelectasis formation and lung consolidation. With re-ventilation of the treated lung, PEEP application and diuretics administration, it then creates a model of pulmonary edema and its progressive resolution. No studies have so far described lung aeration changes during WLL with ultrasound: objectives of the study were to describe ultrasound findings during WLL with validated semiotics in the critically ill and to investigate their relation with the lung’s state of relative aeration.
Methods
In seven patients, 12 lung areas/patient were prospectively studied with ultrasound during six procedural steps of WLL. A three-tiered pattern classification was assigned (1, normal/nearly normal; 2, alveolar-interstitial syndrome; 3, alveolar consolidation) consistently with their previously described meaning in terms of relative air content. The distribution was compared throughout different WLL maneuvers as it was for arterial oxygen measurement distribution.
Results
During one-lung ventilation and saline flooding, ultrasound findings shifted from artifact patterns (normal/nearly normal and alveolar-interstitial syndrome) to alveolar consolidation. Saline removal, re-ventilation and negative water balance were associated with a gradual return to alveolar-interstitial syndrome, then to a normal/nearly normal pattern. Arterial oxygen tension variations were not always consistent with these changes.
Conclusions
In a controlled human model of lung air content variation, the different states of aeration determined by WLL procedure were reliably described with lung ultrasound.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung ultrasound (LUS) has been proven to yield valuable information for lung and pleural pathology assessment in the critically ill [1–4], to be accurate when compared to the imaging gold standard technique, computed tomography [5], and to be more precise than portable chest X-rays [6]. A well-defined semiotics has been validated [1, 7], based both on images (in pleural effusion and non-aerated lung areas) and on artifacts determined by the relative amount of air within explored lung areas (in normal lungs and alveolar-interstitial accumulation of fluids). Recently, LUS has also been shown to accurately describe aeration changes in the clinical setting of ventilator-associated pneumonia [8].
Whole lung lavage (WLL) as treatment of pulmonary alveolar proteinosis [9] is a procedure in which each lung is sequentially lavaged with large amounts of saline to remove from the alveoli the proteinaceous material responsible for the disease. The procedure [10] entails alternate lateral patient position, one-lung ventilation (OLV) of the dependent lung and lavage of previously de-aerated non-dependent lung with multiple tidal volumes of saline. WLL is thus a unique human model of very controlled change of lung air content where, conceptually, the state of the lung at different stages of the procedure closely resembles various pathological conditions: de-aeration of the non-ventilated lung constitutes a model of ongoing re-absorption atelectasis; alveolar flooding with saline represents a model of consolidation; the recovery phase, where re-ventilation of the treated lung, subsequent treatment with positive end expiratory pressure and diuretics promote saline removal, is a model of pulmonary edema and its progressive resolution.
To our knowledge, no one has ever investigated the effects of induced incremental lung de-aeration and of bronchial administration of water with imaging techniques. We hypothesized that already validated LUS semiology could describe the changes in lung aeration during WLL. Aims of the investigation were to: (1) describe LUS findings in WLL with the known semiotics [1, 7] and correlate these to the expected relative aeration of the lung at different steps of WLL; (2) identify if there are any site-specific features regarding the different chest regions; (3) additionally assess changes in arterial oxygenation during different steps of WLL and correlate them with variations in LUS findings.
Materials and methods
Whole lung lavage procedure
Patients were intubated with a Robertshaw oro-tracheal tube, and monitoring with ECG, invasive blood pressure, pulse oxymetry and repeated gas analysis was performed at preset intervals. Patients were maintained under total intravenous anesthesia throughout the procedure. At the beginning and at the end of the procedure, patients were kept supine, while during the lavage phase they were positioned alternatively in right and left semi-lateral decubitus positions (Fig. 1, Figure E1 in ESM). According to the well-established technique [10], patients were submitted to OLV of the dependent lung to allow for better ventilation perfusion matching (Figure E2 in ESM). After starting OLV, we clamped the tube lumen of the non-ventilated lung and waited 30 min to promote complete lung collapse. Lavage was then performed with saline boluses of 0.5–1 l, repeatedly introduced and recovered by gravity, until the recovered fluid became clear. Drainage of saline was then completed with suctioning, and the lavaged lung was re-ventilated. Upon completing the procedure on the first lung (i.e., the left lung), patients were positioned in the left semi-lateral decubitus position, and the same protocol was performed on the controlateral lung. After the second lung lavage, patients were left supine and bilaterally ventilated until extubation criteria were met.
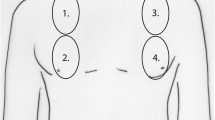
Picture of patient’s semi-lateral decubitus position during whole lung lavage. In this picture, the right semi-lateral decubitus position is shown: left lung is in the non-dependent position and is ready for lavage. Note precise points of the lung ultrasound investigation are marked on the skin to ensure reproducibility of ultrasound acquisition during the whole procedure
Lung ultrasound study
We used linear phased-array 8-MHz probes (Toshiba-Nemio™, Toshiba Medical Systems Europe, Zoetemeer, The Netherlands, or GE-Vivid i™, GE Healthcare, Milwaukee, WI). We defined six areas on each hemithorax, by dividing each hemithorax in an anterior, lateral and posterior region: each region was further divided in an upper and lower quadrant. All these areas were identified considering the thorax’s normal anatomical landmarks: from sternum to anterior axillary line (anterior areas: A and B), from anterior to posterior axillary line (lateral areas: C and D) and from posterior axillary line to spine (posterior areas: E and F). Exact points of investigation (representative of each area and named with the same letters) were identified within each area, marked on the skin (Fig. 1) and examined with ultrasound throughout the study with a longitudinal approach [1]. Twelve points per patient were thus explored at each of the six steps listed in Table 1, steps corresponding to the stages of expected greater change in air lung content consistently with the procedures performed. The overall design of the study is described by Fig. 2.
Design of study protocol. Steps of the study are indicated with Roman numerals from I to VI and are described in Table 1. At steps I and VI, patients were on bilateral ventilation and supine. During all the other phases, patients were kept in semi-lateral position alternatively on the right and left side. At step V, the patients were ventilated bilaterally but still in the semi-lateral decubitus position. Blood samples obtained at steps I, V and VI were thus made during bilateral ventilation. Those obtained at steps II to IV were made during OLV of the right lung and then OLV of the left lung. A total of ten blood samples were thus collected for each patient. Red dots indicate time of BGA sampling. Blue arrows indicate time of LUS examination, performed simultaneously on both lungs (double arrows) at steps I and VI, and sequentially on the non-dependent lung (single arrow) at steps II to V. L left lung, R right lung, OLV one lung ventilation, LUS lung ultrasound, BGA blood gas analysis
Seven-second digital video clips were acquired by a single operator (GV, with 5-year experience in LUS) and stored for subsequent off-line analysis. This was performed by re-viewing video clips and classifying the findings into the three patterns summarized in Table 2 (see Videos 1–5 in ESM). This classification was defined according to the previously described LUS semiotics [1, 7]. Numbering was assigned to the identified patterns on a three-tiered basis, according to their meaning in terms of relative lung air content: pattern 1 (none or few B-lines) is typical of aerated lung areas, while pattern 3 (consolidation) characterizes areas of complete loss of aeration. Such classification was based on current knowledge of bio-physical mechanisms underlying LUS artifacts/image formation [11] and on comparison of LUS findings with other techniques [5, 12].
Blood gas analysis
At each step of the procedure (Fig. 2), arterial blood was sampled to measure oxygen tension (ABL800FLEX™, Radiomether, Copenaghen, Denmark) and calculate its normalized value on oxygen-inspired fraction (PiO2/FiO2 ratio).
Ethics
The study was approved by the local Bioethical Review Board, and informed consent was obtained from each patient.
Statistical analysis
Continuous data were described as mean and standard deviation and categorical data as counts and percentage. Changes over time in the LUS pattern distribution were assessed by means of logistic regression models with calculation of Huber-White robust standard errors to account for intra-patient correlation of measures. For the purpose of this analysis, the pattern was dichotomized as 1/2 vs. 3 and as 1 vs. 2/3. The analysis was adjusted for chest regions. Prespecified contrasts of interest between times were performed by means of the exact McNemar test together for a test for trend. The following matched comparisons of pathophysiological interest were considered: step I vs. II, II vs. III, III vs. IV, IV vs. V, V vs. VI, as well as I vs. V and I vs. VI. Bonferroni correction for multiple tests was applied, and a p < 0.007 was considered for statistical significance. Changes over time of PiO2/FiO2 values were assessed with a general linear regression model and calculation of robust standard errors as above. PiO2/FiO2 value changes at the successive steps were informally (graphically) compared to the corresponding LUS pattern variations.
Stata10 (StataCorp, College Station, TX) was used for computation.
Additional information on material and methods is given in the ESM.
Results
Seven patients (4 males, 3 females; mean age 43 ± 15 years) were enrolled. All procedures were performed according to the study protocol. Mean duration of the core part of WLL (from steps II to V) was 4 h and 51 min (±65 min). Observation at step VI was performed after a mean time of 15 h and 8 min (±1 h and 32 min) from the end of the second lung’s lavage. The mean amount of saline used per lung was 17.3 ± 3.9 l for left lungs and 16.3 ± 4.5 l for right lungs. From steps V to VI, negative fluid balance was achieved in all patients (−1,279 ± 691 ml). On each patient LUS was performed on all areas. Quality of acquired video clips was always satisfactory. Overall, 84 lung areas (28 anterior/28 lateral/28 posterior) were prospectively explored throughout the six procedural steps. A total of 504 lung scans were thus performed. Examination time per step was <5 min (10 min for steps I and VI, entailing both lungs’ assessment).
Distribution of LUS findings is reported as counts/step in Table 3, and as percentages/step in Fig. 3a. The pattern distribution changed significantly over time (p < 0.001), except from steps III to IV.
Changes in lung ultrasound pattern (a) and PaO2/FiO2 ratio (b) over time during whole lung lavage. Steps of whole lung lavage procedure (x axis) are described in Table 1. a Percentage of lung ultrasound pattern per step is reported on y axis. Lung ultrasound patterns (also described in Table 2) are represented by: 1 normal/nearly normal pattern; 2 alveolar-interstitial syndrome; 3 alveolar consolidation. Prevalence of patterns at each step is reported as percentage of all 84 studied lung areas (6 areas per each lung per each of the 7 patients). *p < 0.001 each step vs. preceding one (I vs. II, II vs. III, IV vs. V, V vs. VI). † p < 0.001 step I vs. V, and step I vs. VI. b Values of P/F ratio (arterial oxygen tension/inspired oxygen fraction) are reported on the y axis. ‡ p < 0.007 each step vs. preceding one. § p < 0.007 step I vs. VI)
At step I a pathological pattern with alveolar-interstitial syndrome (pattern 2) was found in 71.43% of explored areas. Pattern 1 decreased at step II, and artifactual patterns (1 and 2 altogether) almost completely disappeared at step III (98.81% pattern 3) and were absent at step IV. At step V, artifactual patterns re-appeared and consolidation decreased substantially (pattern 3, 29.76%); no normal/near normal areas were found, with a prevailing high-density B-line pattern (pattern 2, 70.24%). At step VI pattern 1 re-appeared, representing together with pattern 2 the majority of findings (58.33% pattern 1, 38.1% pattern 2). A typical sequence from steps I to VI is shown in Fig. 4 and Videos 6–11 in the ESM.
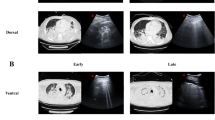
Typical sequence of ultrasound findings in a studied area. Lung ultrasound images refer in this case to the upper quadrant in the anterior region (named area “A” in the study) of the right lung. From pattern 1 (nearly normal pattern, a at basal condition, OLV determined a shift to pattern 2 (b alveolar-interstitial syndrome) then to pattern 3 (c consolidation). Saline flooding maintained the state of total loss of aeration of the lung, i.e., pattern 3 (d consolidation). Re-ventilation was associated with re-appearance of pattern 2 (e alveolar-interstitial syndrome). Prolonged ventilation with positive end expiratory pressure and negative water balance yielded a return to pattern 1 (in this case, normal pattern, f). Sequence of images from a to c describes the process of ongoing re-absorption atelectasis. Sequence from e to f illustrates the process of healing of a “wet lung.” Images c and d were obtained with a tranversal approach (note absence of ribs shadows) rather than the longitudinal one used in the study: this was done for didactical purposes to better appreciate the extension of consolidation
Similar results were obtained when considering single chest regions (anterior, lateral, posterior) (Table 4). Moreover, patterns appeared to differ between regions as well, with significant differences in pattern distribution between the posterior and both the anterior (p < 0.007) and lateral (p < 0.001) areas at steps II, V and VI (Fig. 5, Table 4).
Changes in lung ultrasound pattern over time during WLL, adjusted for chest region. Steps of WLL procedure (x axis) are described in Table 1. Prevalence of ultrasound pattern per step is reported on y axis. Lung ultrasound patterns (also described in Table 2) are represented by: 1 normal/nearly normal pattern; 2 alveolo-interstitial syndrome; 3 alveolar consolidation. Prevalence of patterns at each step is reported as percentage per each chest region, respectively, anterior (upper row of panels), lateral (middle row) and posterior (lower row). *p < 0.007 anterior vs. posterior areas. † p < 0.001 lateral vs. posterior areas. ‡ p < 0.007 lateral vs. posterior areas
P/F showed significant variation over time (P < 0.007) except from steps I to II and IV to V (Table 5, Fig. 3b).
Discussion
In this controlled human model of lung air content variation, LUS reliably recorded the changes in the state of lung aeration. Starting from a dominant pattern of alveolar-interstitial syndrome (step 1, as typical of pulmonary alveolar proteinosis [13]), relevant and obvious changes in lung air content induced by WLL maneuvers were linked to significant variations in LUS pattern in all lung areas explored (Fig. 3a). During OLV, consolidation appeared (step II), then becoming the dominant pattern with lung collapse (step III) and alveolar flooding (step IV). Upon re-ventilation (step V), a dominant artifactual pattern re-appeared: aveolo-interstitial syndrome became more frequent than at step I, with expression of residual water into the lavaged lung (making it look “more ill” than before WLL). After treatment with PEEP and negative water balance (step VI), overall B-line density markedly decreased, and “healthy” areas (pattern 1) re-appeared.
As hypothesized, LUS patterns previously validated in the critically ill accurately described the changes in lung condition determined by the procedure. In terms of LUS appearance, OLV produced a pattern of consolidation resembling atelectasis [14] and lung flooding to pneumonia [8, 15] (Fig. 4c, d). Our findings after lavaged lung re-ventilation (Fig. 4e) were comparable to well-described ones in pulmonary edema [12], acute respiratory distress syndrome [5, 16] and animal experimental settings of acute lung injury [17, 18], conditions characterized by increased extravascular lung water [12]. Changes occurring with ventilation and negative water balance were also the same as observed in healing course (and the reverse of what was observed in worsening [17, 19]) of these pathologies (Fig. 4e, f). Moreover, LUS appearance during progression from emptying of lungs after lavage (consolidation) to significant improvement before extubation (decrease/disappearance of B-lines) resembled what is described in re-aeration of lung contusion [3] and in the evolution of ventilator-associated pneumonia [8, 15]. In particular, our findings are very similar to the ones described in the clinical model represented by pneumonia and its response to antibiotic therapy [8], even though LUS changes are observed in this setting on a different time scale and show less homogeneous distribution in comparison to the iatrogenic and uniform aeration changes observed during WLL.
Local differences between studied areas, due to the position in respect to gravity, further confirmed the correlation between LUS findings and the state of lung aeration. In the early phase of OLV (step II), posterior areas showed patterns of worse aeration more frequently than in anterolateral ones (Fig. 5) (i.e., they underwent a faster disventilation). Regional differences disappeared with lung collapse and with lavage (steps III and IV), as a consequence of the complete gas re-absorption and the great amount of saline introduced, irrespectively of gravity. Differences then reappeared with re-ventilation and at end procedure stages (steps V and VI): posterior areas altogether maintained a worse degree of aeration (i.e., they re-ventilated and lost residual saline content less easily). This was not surprising, as nondependent regions of a “wet lung” are expected to place a burden on dependent ones, similarly to what is described in acute respiratory distress syndrome [20].
Arterial oxygenation (P/F) showed variations during WLL not always consistent with lung aeration changes, but rather referable to ventilation/perfusion matching. This is evident by looking at variations observed with lung flooding (from steps III to IV): saline filling of the non-dependent lung at a driving pressure of 70–80 cmH2O determined a dramatic increase in P/F (with no relevant change in LUS pattern) by diversion of blood flow toward the dependent, ventilated lung [21]. Discrepancies between P/F and LUS variations were also observed at resumption of bilateral ventilation (step V): a lack of change in P/F from step IV was associated to substantial improvement in lung aeration and LUS pattern. On a pathophysiological basis, all this is not unexpected: arterial oxygenation is the result of ventilation/perfusion matching and of both lung’s function, while LUS findings depend on the state of aeration of the sole examined lung. In addition, resumption of ventilation of the lavaged lung re-aerates it, but also re-distributes part of the previously diverted blood to a “wet” lung (the drainage of saline is always incomplete, and the lung also experiences a loss of surfactant).
Our description of lung aeration changes with previously validated LUS semiotics in this unusual biological model corroborates the recently demonstrated accuracy of LUS in bedside monitoring of lung pathology [8]. Furthermore, it represents an indirect confirmation of how ultrasound image formation in several lung diseases strictly depends on the state of relative lung aeration, as already hypothesized [1, 11].
Our work has some limitations. Firstly, these are preliminary data on a small number of patients, despite the 84 areas prospectively studied. Furthermore, LUS was not compared with other imaging techniques, but both computed tomography and chest X-ray are unsuitable because of the close bedside monitoring needed. Thirdly, we didn’t exactly quantify lung air/water content throughout the procedure, but this had a negligible effect on our findings: all changes in lung state were determined by relevant procedures (OLV, saline filling, re-ventilation, etc.), with direct and undisputable effects. Although other authors estimated lung volume with computed tomography [22], related LUS findings with lung water content [13] or even measured at bedside functional residual capacity [23], no technique suitable for our purpose is available for bedside monitoring.
Conclusions
In a human model of controlled lung air content variation, we described with previously clinically validated LUS semeiotics the different states of aeration determined by the procedure. These findings need confirmation on a wider population. Comparison with pathological states encountered in the critically ill also needs further investigation.
Abbreviations
- LUS:
-
Lung ultrasound
- OLV:
-
One-lung ventilation
- PaO2/FiO2 :
-
Arterial oxygen tension/inspired oxygen fraction ratio
- WLL:
-
Whole lung lavage
References
Lichtenstein D (2007) Ultrasound in the management of thoracic disease. Crit Care Med 35:S250–S261
Volpicelli G, Mussa A, Garofalo G, Cardinale L, Casoli G, Perotto F, Fava C, Frascisco M (2006) Bedside lung ultrasound in the assessment of alveolar–interstitial syndrome. Am J Emerg Med 24:689–696
Soldati G, Testa A, Silva FR, Carbone L, Portale G, Silveri NG (2006) Chest ultrasonography in lung contusion. Chest 130:533–538
Lichtenstein D, Mezière G (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 134:117–125
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ (2004) Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasound in acute respiratory distress syndrome. Anesthesiology 100:9–15
Soldati G, Testa A, Sher S, Pignataro G, La Sala M, Silveri NG (2008) Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest 133:204–211
Soldati G (2006) Sonographic findings in pulmonary diseases. Radiol Med 111:507–515
Bouhemad B, Liu ZH, Arbelot C, Zhang M, Ferarri F, Le-Guen M, Girard M, Lu Q, Rouby JJ (2010) Ultrasound assessment of antibiotic-induced pulmonary reaeration in ventilator-associated pneumonia. Crit Care Med 38:84–92
Juvet SC, Hwang D, Waddell TK, Downey GP (2008) Rare lung disease II: pulmonary alveolar proteinosis. Can Respir J 15:203–210
Rodi G, Iotti G, Galbusera C, Mencherini S, Raimondi F, Braschi A (1995) Whole lung lavage. Monaldi Arch Chest Dis 50:64–66
Soldati G, Copetti R, Sher S (2009) Sonographic interstitial syndrome: the sound of lung water. J Ultrasound Med 28:163–174
Agricola E, Bove T, Opizzi M (2005) “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest 127:1690–1695
Reissig A, Kroegel C (2003) Transthoracic sonography of diffuse parenchymal lung disease: the role of comet tail artifacts. J Ultrasound Med 22:173–180
Lichtenstein DA, Lascols N, Mezière G, Gepner A (2004) Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med 30:276–281
Reissig A, Kroegel C (2007) Sonographic diagnosis and follow up of pneumonia: a prospective study. Respiration 74:537–547
Copetti R, Soldati G, Copetti P (2008) Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 6:16
Gargani L, Lionetti V, Di Cristofano C, Bevilacqua G, Recchia FA, Picano E (2007) Early detection of acute lung injury uncoupled to hypoxemia in pigs using ultrasound lung comets. Crit Care Med 35:2769–2774
Rajan GR (2007) Ultrasound lung comets: a clinically useful sign in acute respiratory distress syndrome/acute lung injury. Crit Care Med 35:2869–2870
Agricola E, Picano E, Oppizzi M, Pisani M, Meris A, Fragasso G, Margonato A (2006) Assessment of stress-induced pulmonary interstitial edema by chest ultrasound during exercise echocardiography and it correlation with left ventricular function. J Am Soc Echocardiogr 19:457–463
Gattinoni L, Pesenti A (2005) The concept of “baby lung”. Intensive Care Med 31:776–784
Cohen E, Eisenkraft JB (1990) Bronchopulmonary lavage: effects on oxygenation and hemodynamics. J Cardiothorac Anesth 4:609–615
Puybasset L, Cluzel P, Chao N, Slutsky AS, Coriat P, Rouby JJ, The CT scan ARDS Study Group (1998) A computed tomography scan assessment of regional lung volume in acute lung injury. Am J Resp Crit Care Med 158:1644–1655
Patroniti N, Saini M, Zanella A, Weismann D, Isgrò S, Bellani G, Foti G, Pesenti A (2008) Measurement of end-expiratory lung volume by oxygen washin-washout in controlled and assisted mechanically ventilated patients. Intensive Care Med 34:2235–2240
Acknowledgments
We are very thankful to Dr. Gino Soldati for his valuable suggestions on developing the study, to Dr. Vincenzo Emmi for his encouraging comments and to Dr. Marco Garrone for language revision.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Video 1 (MPG 460 kb)
Supplementary Video 2 (MPG 460 kb)
Supplementary Video 3 (MPG 678 kb)
Supplementary Video 4 (MPG 290 kb)
Supplementary Video 5 (MPG 206 kb)
Supplementary Video 6 (MPG 540 kb)
Supplementary Video 7 (MPG 317 kb)
Supplementary Video 8 (MPG 499 kb)
Supplementary Video 9 (MPG 290 kb)
Supplementary Video 10 (MPG 460 kb)
Supplementary Video 11 (MPG 238 kb)
Rights and permissions
About this article
Cite this article
Via, G., Lichtenstein, D., Mojoli, F. et al. Whole lung lavage: a unique model for ultrasound assessment of lung aeration changes. Intensive Care Med 36, 999–1007 (2010). https://doi.org/10.1007/s00134-010-1834-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1834-4