Abstract
Purpose
To estimate the disease burden due to 15 mental disorders at both individual and population level.
Methods
Using a population-based survey (Nemesis, N = 7,056) the number of years lived with disability per one million population were assessed. This was done with and without adjustment for comorbidity.
Results
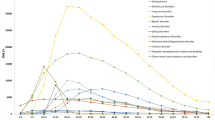
At individual level, major depression, dysthymia, bipolar disorder, panic disorder, social phobia, eating disorder and schizophrenia are the disorders most markedly associated with health-related quality of life decrement. However, at population level, the number of affected people and the amount of time spent in an adverse health state become strong drivers of population ill-health. Simple phobia, social phobia, depression, dysthymia and alcohol dependence emerged as public health priorities.
Conclusions
From a clinical perspective, we tend to give priority to the disorders that exact a heavy toll on individuals. This puts the spotlight on disorders such as bipolar disorder and schizophrenia. However, from a public health perspective, disorders such as simple phobia, social phobia and dysthymia—which are highly prevalent and tend to run a chronic course—are identified as leading causes of population ill-health, and thus, emerge as public health priorities.
Similar content being viewed by others
References
Murray CJL, Lopez AD (1996) The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. vol 1, Mass: Harvard School of Public Health, on behalf of the World Health Organization and the World Bank, Cambridge
Menken M, Munsat TL, Tolle JF (2000) The global burden of disease study: implications for neurology. Arch Neurol 57:418–420
Begg SJ, Vos T, Barker B, Stanley L, Lopez AD (2008) Burden of disease and injury in Australia in the new millennium: measuring health loss from diseases, injuries and risk factors. Med J Australia 188:36–40
Mathers CD, Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PloS Med 3(11):e442. doi:10.1371/journal.pmed.0030442
World Health Organization (2006) Dollars, DALYs and Decisions. World Health Organization, Geneva
World Health Organization (2008) Mental Health Gap Action Programme: scaling up for mental, neurological and substance use disorders. World Health Organization, Geneva
Lancet Global Mental Health Group (2007) Scale up services for mental health: a call for action. Lancet 370:1241–1252
Bijl RV, Van Zessen G, Ravelli A (1998) The Netherlands Mental Health Survey and Incidence Study (NEMESIS): objectives and design. Soc Psychiatry Psychiatr Epidemiol 33:581–586
World Health Organization (1997) Composite International Diagnostic Interview (CIDI), version 2.1, 12-months. World Health Organization, Geneva
Ter Smitten MH, Smeets RMW, van den Brink W (1998) Composite International Diagnostic Interview (CIDI),Version 2.1, 12-months (in Dutch). World Health Organization, Amsterdam/Geneva
Wittchen HU (1994) Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res 28:57–84
Brazier J, Roberts J, Deverill M (2002) The estimation of a preference-based measure of health from the SF-36. J Health Econ 21:271–292
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36): i. Conceptual framework and item selection. Med Care 3:473–483
Von Neumann J, Morgenstern O (1953) Theory of games and economic behavior. Wiley, New York
Gafni A (1994) The standard gamble method: what is being measured and how it is interpreted. Health Serv Res 29:207–224
Andrews G, Sanderson K, Beard J (1998) Burden of disease: methods of calculating disability from mental disorder. Brit J Psychiatry 173:123–131
Hox JJ (2010) Multilevel Analysis: Techniques and Applications. Taylor and Francis Group, New York
Walters SJ, Brazier JE (2005) Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 14:1523–1532
Smit F, Cuijpers P, Oostenbrink J, Batelaan N, De Graaf R, Beekman A (2006) Costs of nine common mental disorders: implications for curative and preventive psychiatry. J Ment Health Policy Econ 9:193–200
De Graaf R, Bijl RV, Spijker J, Beekman ATF, Vollebergh WAM (2003) Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance disorders. Soc Psychiatry Psychiatr Epidemiol 38:1–11
ESEMeD (2004) Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand 109(suppl):38–46
de Graaf R, Tuithof M, van Dorsselaer S, ten Have M (2012) Comparing the effects on work performance of mental and physical disorders. Soc Psychiatry Psychiatr Epidemiol: doi:10.1007/s00127-012-0496-7
Weehuizen R (2008) Mental capital: the economic significance of mental health. University of Maastricht, Dissertation
Saarni SI, Ari JS, Sintonen H, Pirkola S, Koskinen S, Aroma A, Lönnqvist J (2007) Impact of psychiatric disorders on health-related quality of life: general population survey. Brit J Psychiatry 190:326–332
Bowie C, Beck S, Bevan G, Raftery J, Silverton F, Stevens A (1997) Estimating the burden of disease in an English region. J Public Health Med 19:87–92
Mathers CD, Vos T, Stevenson E, Begg SJ (2001) The burden of disease and injury in Australia. Bull World Health Organ 79:1076–1084
Vos T, Mathers CD (2000) The burden of mental disorders: a comparison of methods between the Australian burden of disease studies and the Global Burden of Disease study. Bull World Health Organ 78:427–438
Stouthard M, Essink-Bot M-L, Bonsel G, Barendregt J, Kramers P, Van de Water H, Gunning-Schepers M-L, Van der Maas P (1997) Disability weights for diseases in the Netherlands. Department of Public Health, Erasmus University, Rotterdam
Gmel G, Gutjahr E, Rehm J (2003) How stable is the risk curve between alcohol and all-cause mortality and what factors influence the shape? A precision-weighted hierarchical meta-analysis. Eur J Epidemiol 8:613–642
Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, Sempos CT, Jernigan D (2003) Alcohol as a risk factor for global burden of disease. Eur Addict Res 9:157–164
Chisholm D, Rehm J, Van Ommeren M, Monteiro M (2004) Reducing the global burden of hazardous alcohol use: comparative cost-effectiveness analysis. J Stud Alcohol 65:782–793
Konnopka A, König H–H (2009) The health and economic consequences of moderate alcohol consumption in Germany 2002. Value Health 2:253–261
Pillai A, Nayak MB, Greenfield TK, Bond JC, Nadkarni A, Patel V (2012) Patterns of alcohol use, their correlates, and impact in male drinkers: a population-based survey from Goa India. Soc Psychiatry Psychiatr Epidemiol 48(2):275–282
Craig BM, Busschbach JJ, Salomon JA (2009) Keep it simple: ranking health states yields values similar to cardinal measurement approaches. J Clin Epidemiol 62:296–305
Acknowledgments
The Nemesis study was financially supported by the Netherlands’ Ministry of Health (VWS).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
Nemesis was conducted with the approval of the ethics committee of the Netherlands Institute of Mental Health and Addiction, Utrecht, the Netherlands. Respondents provided informed consent according to the prevailing Dutch law of 1996 after having been informed about the aims of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lokkerbol, J., Adema, D., de Graaf, R. et al. Non-fatal burden of disease due to mental disorders in the Netherlands. Soc Psychiatry Psychiatr Epidemiol 48, 1591–1599 (2013). https://doi.org/10.1007/s00127-013-0660-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-013-0660-8