Abstract
Introduction
Mental disorders are highly prevalent in Germany, and associated with decreased quality of life for those affected as well as high economic burden for the society. The purpose of this study was to determine the excess costs of mental disorders and to examine how these differ with respect to disease severity.
Methods
We analyzed mean 6-month costs using the baseline data from the RECOVER trial in Hamburg, Germany, which evaluates an innovative stepped-care model for mental disorders. Four severity levels were classified based on the current level of mental illness, loss of functioning, and psychiatric diagnosis. In this work, direct costs (outpatient, inpatient, and social/informal care) and indirect costs (sick leave, unemployment, and early retirement) were estimated using interview-based data on health care utilization and productivity losses. Excess costs were determined by matching a comparison group of the German general population without mental disorders. Group differences in sociodemographic covariates and somatic comorbidities were balanced using entropy balancing. Excess costs by severity levels were estimated using generalized linear models (GLM) with gamma distribution and log-link function.
Results
Overall, the RECOVER group included n = 816 and the comparison group included n = 3226 individuals. Mean total 6-month excess costs amounted to 19,075€, with higher indirect excess costs (13,331€) than direct excess costs (5744€) in total excess costs. The excess costs increased with increasing disease severity, ranging from 6,123€ with mild disease severity (level 1) to 31,883€ with severe mental illness (level 4). Indirect excess costs ranged from 5612€ in level 1 to 21,399€ in level 4, and were statistically significant for all disease severity levels. In contrast, direct excess costs were only statistically significant for the levels 2 to 4, and ranged from 511€ in level 1 to 10,485€ in level 4. The main cost drivers were hospital stays (level 2–4), sick leave and unemployment (all levels), and early retirement (level 3–4).
Discussion
Mental disorders are associated with high costs that increase with the level of disease severity, which was also shown for individual ICD-10 diagnosis groups. Due to their influence on costs, indirect costs and disease severity levels should be considered in future cost-of-illness studies of mental disorders.
Clinical trial registration
clinicaltrials.gov, trial registration number NCT03459664.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental disorders are associated with a high disease burden, including reduced quality of life and social functioning, as well as increased costs for society [1, 2]. In Germany, the total costs of mental disorders are estimated to be about 147 billion Euros in 2015, including direct costs due to health care service utilization, spending for social security, and indirect costs due to lost or reduced productivity [3]. With a 12-month-prevalence of 27.8%, about one third of the German adult population is affected by at least one mental disorder each year [4]. However, only 18.9% of the individuals with mental disorders (12-month diagnosis) sought for any health care treatment related to mental health within 1 year [5].
By international standards, the German health care system generally provides universal access, and a high quality of care [6]. Yet, there are shortcomings in care with respect to the treatment of mental disorders. In general, the outpatient and inpatient sectors are strictly separated, which limits the continuity of treatment for individuals with mental disorders [7]. Long waiting times, especially in the outpatient sector, encourage a shift to the cost-intensive inpatient sector [8]. In this context, the German mental health care system is particularly challenging, as a large number of different health service providers, funded by different authorities, is involved [9]. Furthermore, for mental disorders such as schizophrenia, which are associated with severe courses of illness, there are fewer psychotherapeutic services available than recommended in clinical practice guidelines [7]. New care approaches aim to overcome the existing structural deficits in the health care system to meet the demand for more patient-oriented, resource-efficient treatment options. The German Association for Psychiatry, Psychotherapy and Psychosomatics (Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde e. V.—DGPPN) calls among others for treatment of mental disorders based on the level of disease severity, as provided by stepped care approaches [10]. The stepped care approach aims to improve care while being resource efficient by aligning and constantly adjusting the intensity of care with the disease severity, starting with the least intensive approach [11].
Cost-of-illness studies of mental disorders provide information about the economic impact on society, which can be valuable for health policy decisions. So far, few studies have analyzed the costs of mental disorders as a group in Germany, most recently, the study by Gustavsson and colleagues [12]. This study provides comprehensive cost estimates of mental and neurological disorders for several European countries, which were also used for more recent reports on the economic burden of mental disorders [3, 12]. However, the data for the included diagnosis groups stem from different data sources that originated in 2010 or earlier [12]. Excess costs are generally reported less frequently, and to our knowledge, excess costs of mental disorders have not been estimated for the German health care system yet. Within the EU, the latest findings on excess costs of mental disorders were reported from Austria [13]. Excess costs are calculated as the difference in mean costs of a group with a particular disease and a control group without that disease. The advantage of this approach is that it also captures costs that cannot be directly related to a disease, and thus cost-of-illness can be measured more precisely [14, 15]. More recent studies from Germany have estimated the cost-of-illness of specific diagnosis groups, including social anxiety disorder, depression, alcohol-dependence and schizophrenia [16,17,18,19]. Since there is in most cases no differentiation between diagnosis groups in the provision of health care services for mental disorders, cost estimates for mental disorders as a whole have the advantage that they are much closer to the actual healthcare system. In addition, comorbid mental disorders can be addressed comprehensively. This study contributes to the existing body of research by providing actual estimates of the direct and indirect excess costs of mental disorders in Germany. Further, excess costs by different levels of disease-severity are estimated to provide information on the extent to which severity levels differ in terms of health care utilization and productivity losses, and thus economic burden.
Methods
Study design
Data on individuals with mental disorders were obtained from the randomized-controlled trial (RCT) RECOVER, conducted at the University Medical Center Hamburg-Eppendorf in Northern Germany. In the RECOVER care model, several innovative and evidence-based care components such as case management, assertive community treatment, and e-therapy were combined in a cross-sectoral, stepped care approach and compared to regular care with respect to patient-relevant outcomes, costs, and effectiveness [20]. For our analysis, we used the baseline data (n = 889), which was collected from 2018 to 2019 by clinically trained interviewers. We matched a control group using a dataset representative of the German general population in age, sex, residence state, and education level (n = 5005) [21]. The data of the control group were collected via telephone interviews and contains general information on the sample like sociodemographic variables or comorbidities, as well as information on the resource utilization. More details on the data sources are published elsewhere [20, 21].
Study sample
Many study participants with mental disorders were directly recruited at the University Medical Center Hamburg-Eppendorf, while other recruitment channels were external partners such as primary care physicians or psychotherapists, or the website of the RECOVER study. Since home treatment was a part of the RECOVER intervention, the study participants were recruited from the catchment area of the study center (≤ 8 km distance). Furthermore, study participants were eligible for inclusion if they were ≥ 16 years old and insured in one of the participating statutory health insurance funds, which together account for a population share of approximately 38%.
We excluded participants with missing values with respect to sociodemographic and clinical covariates (n = 38), health care utilization and productivity losses (n = 35) from the analysis, resulting in a final sample of n = 816 individuals with mental disorders. Among these were n = 56 individuals with mild disease severity (level 1), n = 306 individuals with moderate disease severity (level 2), n = 294 individuals with moderate to severe disease severity (level 3), and n = 160 individuals with severe mental illness (level 4).
As for the control group, we further restricted the data to individuals without self-reported medical diagnosis of any mental disorder (exclusion of n = 985 participants), with statutory health insurance (exclusion of n = 685 participants), and without missing values (exclusion of n = 109 participants), resulting in a final sample of n = 3226 individuals without mental disorders.
Assessment of the psychiatric diagnosis
Clinically trained interviewers conducted a thorough assessment of the psychiatric diagnosis using the structured clinical interview for DSM-IV (SCID-I/II) [22] and diagnosis-specific questionnaires (for details see Table S1) [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. Participants with any primary diagnosis of a mental disorder according to the International Statistical Classification of Diseases and Related Health Problems—10th Revision (ICD-10) were included, except for study participants with a primary diagnosis in the spectrum of organic, including symptomatic, mental disorders (ICD-10 F0) or mental and behavioral disorders due to psychoactive substance use (ICD-10 F1). The following primary diagnoses were included: Schizophrenia, schizotypal and delusional disorders (ICD-10 F2), mood disorders (ICD-10 F3), neurotic, stress-related and somatoform disorders (ICD-10 F4), behavioral syndromes associated with physiological disturbances and physical factors (ICD-10 F5), disorders of adult personality and behavior (ICD-10 F6), disorders of psychological development (ICD-10 F8) or behavioral and emotional disorders with onset usually occurring in childhood and adolescence (ICD-10 F9).
Assessment of the severity level
In this study, four severity levels were distinguished as classified for the stepped-care treatment in the RECOVER study, which was based on the psychiatric diagnosis, the current level of mental illness (Clinical Global Impressions-Severity scale, CGI-S [43]), and the loss of functioning (Global Assessment of Functioning, GAF [44]), for further details see Table 1 and the study protocol of the RECOVER study [20]. Only patients with severe mental illness and a diagnosis of psychosis or borderline personality disorder were assigned to severity level 4, as they were included in integrated care models for these disorders. If there were discrepancies between the three measures, the GAF and CGI-S were leading, and in the rare case that these measures differed, the GAF. For severity level 4, it was sufficient if either the GAF or the CGI-S fulfilled the criteria for a severe mental illness.
Cost assessment
We analyzed 6-month direct and indirect costs on the basis of self-reported resource utilization, assessed for the 6 months before the interview using modified versions of the FIMA questionnaire (‘Fragebogen zur Erhebung von Gesundheitsleistungen im Alter’—Questionnaire for Health-Related Resource Use in an Elderly Population) and FIMPsy questionnaire (‘Fragebogen zur Inanspruchnahme medizinischer und nicht medizinischer Versorgungsleistungen bei psychischen Erkrankungen’—Questionnaire for the Assessment of Medical and non Medical Resource Utilization in Mental Disorders) [45, 46]. In general, the costs were estimated by multiplying self-reported resource use with published unit costs.
Direct costs included outpatient, inpatient, and social/informal care services, which were valued with published unit costs for Germany [47, 48]. Outpatient services encompassed physicians, outpatient clinic/psychiatric outpatient department, and other health care professionals. In the RECOVER baseline data, outpatient treatment in the hospital was surveyed separately for general and psychiatric services, contrary to the dataset of the control group. Therefore, the data were combined in the cost category ‘outpatient clinic/psychiatric outpatient department’. For outpatient clinic/psychiatric outpatient department and radiologists, we used the arithmetic mean of the other physicians’ unit costs since no published unit costs were available. Inpatient services encompassed hospital/day-care and rehabilitation. Hospital/day care encompassed day care and inpatient stays in general or psychiatric hospitals. For full inpatient stays (> 1 day in hospital/rehabilitation), we subtracted 1 day from the number of days reported, as the number of overnight stays are reimbursed in Germany. Social/informal care services encompassed professional home help and help from family or friends (informal care). Informal care was assessed by asking the study participants about the number of days they received help from family and friends in the last 6 months, and the average duration of this contact per day. The information on total duration (in hours) was then valued monetarily with average published unit costs, representing substitution costs of a comparable professional occupation [47]. The following services were assessed for the group of individuals with mental disorders, but were not available for the control group, and consequently not included in the cost analysis: Medication, sheltered/supported accommodation, and services for participation in working life.
Indirect costs included productivity losses due to sick leave, unemployment, and early retirement and were estimated with the human capital approach. The human capital approach assesses productivity losses to society by taking the entire period of lost working force due to morbidity or death into account, and evaluates indirect costs with income losses [49]. Another commonly used approach would be the friction cost approach, which only assesses the costs incurred in the time period until the replacement by a new employee, including training and recruitment-related expenses [50]. In both approaches, productivity losses due to unemployment are generally not directly evaluated. Mental disorders are associated with higher unemployment rates than in the general population [51, 52]. In this analysis, we wanted to assess the differences in unemployment rates between individuals with mental disorders and individuals without mental disorders. For this purpose, we have also valued unemployment in monetary terms.
The basic approach was to multiply the productivity losses by average daily wages for full-time and part-time employees. In particular, the average monthly gross income for full-time and part-time work was supplemented by the employer's social insurance contributions, and calculated on a daily basis after deduction of vacation days and public holidays, resulting in 265.53 € per day [53, 54]. We estimated the costs of sick leave for individuals who reported to be working either in full-time or part-time by valuing monetarily the number of self-reported days spent on sick leave in the last 6 months. The costs of early retirement were estimated if persons indicated that they received a disability pension at the time of the interview. In Germany, individuals receiving full disability pension are allowed to work a maximum of two hours per day, which corresponds to 6 h or 75% of lost productivity in a regular 8-h working day [55]. The amount of productivity losses due to the disability pension was not assessed. Therefore, we assumed productivity losses of 75% for full disability pension, which equals 97.5 days of lost productivity for 6 months. In this study, the unemployment rates for individuals with mental disorders were much higher compared to individuals without mental disorders. Therefore, we also valued the costs of unemployment monetarily by valuing assumed productivity losses of 100% (130 days) monetarily if individuals indicated that they were unemployed at the time of the interview. All unit costs were inflated to the year 2019 using the consumer price index. Table S2 provides further details on the cost categories included and their respective unit costs.
Statistical analysis
Before the analysis of excess costs, differences in sociodemographic covariates and somatic comorbidities between the group of individuals with mental disorders and the control group were balanced to account for potential confounding. Balancing of the groups was performed with entropy balancing (EB) using the corresponding software package in Stata [56]. EB is a method that assigns a weight to each observation in the control group to achieve covariate balance between groups, in this study with respect to the mean and variance of all covariates included in the EB model [57]. EB allows to balance many relevant socioeconomic and clinical covariates at the same time, and can thus be used to estimate the average treatment effect on the treated [57]. The following covariates were reweighted in the control group to balance the control group and the group of individuals with mental disorders: age, gender, marital status (three categories), school level (five categories), education level (three categories), body mass index (five categories following the World Health Organization [58]), and somatic comorbidities according to the ICD-10 chapters II, IV, and IX–XIII. After EB, the included covariates are expected to be almost equally distributed in mean and variance between the group of individuals with mental disorders and the control group. See Table 2 for the sample characteristics of the groups and more details on the included covariates, and see Table S3 in the supplement for the sample characteristics before balancing.
We estimated costs using generalized linear models (GLM) with a gamma distribution and log-link function to account for the distribution of cost data. Each cost category was analyzed in a GLM, with the respective cost category as dependent variable and the group assignment (individuals with/without mental disorders) as independent variable. The groups were adjusted for observable factors by including the EB weights in the GLM. For each group, the weighted mean costs were calculated. The excess costs were estimated as average marginal effects of the groups, and considered to be statistically significant at a p value < 0.05. The excess costs were further estimated for each severity level using the previously calculated EB weights to balance the respective severity level group and the control group. In addition, subgroup analyses were performed for the most frequent primary diagnosis groups according to the ICD-10, as these were represented differently in the severity levels. Since the subdivision according to main diagnosis led to small subgroups in some cases, we only analyzed subgroups with at least 25 observations. For severity level 1, no subgroup analyses were performed. In severity levels 2 and 3, the diagnosis groups neurotic, stress-related and somatoform disorders (ICD-10 F4), mood disorders (ICD-10 F3), and disorders of adult personality and behavior (ICD-10 F6) were analyzed, and in level 4, the diagnosis groups disorders of adult personality and behavior (ICD-10 F6) and schizophrenia, schizotypal and delusional disorders (ICD-10 F2). For better comparability across subgroups, the control groups were adjusted using the same EB weights as in the primary analysis. All analyses were performed in Stata version 16.
Sensitivity analyses
In a first sensitivity analysis, we conducted an unweighted analysis of excess costs to test the influence of the group balancing on costs. In this study, unemployment was considered when calculating indirect costs, which is quite uncommon in cost-of-illness studies. Therefore, we excluded the indirect costs of unemployment in a second sensitivity analysis to test their influence on the total and indirect excess costs.
Results
Sample characteristics
Among the individuals with mental disorders, 46.8% were diagnosed with mood disorders (ICD-10 F3), in 90.3% of the cases major depression, followed by 22.4% diagnosed with neurotic, stress-related and somatoform disorders (ICD-10 F4), 21.6% diagnosed with disorders of adult personality and behavior (ICD-10 F6), 8.1% diagnosed with schizophrenia, schizotypal and delusional disorders (ICD-10 F2), 0.5% diagnosed with behavioral syndromes associated with physiological disturbances and physical factors (ICD-10 F5), 0.5% diagnosed with behavioral and emotional disorders with onset usually occurring in childhood and adolescence (ICD-10 F9), and 0.1% diagnosed with disorders of psychological development (ICD-10 F8). After the adjustment of the control group, the predefined covariates in the groups were almost equally distributed in mean and variance (see Table 2). In both groups, individuals were on average 36.9 years old, and the share of women (59.9%) was higher than that of men. The study participants were mostly single (53.8%) or married/having a partner (38.8%), and of normal weight (52.8%). Before the group adjustment, individuals in the control group were on average 54.4 years old, and the share of women (53.1%) was lower than after the adjustment; for more details, see Table S3.
However, the difference in unemployment rates was substantial: While unemployment was low at 2.9% in the control group, it was at 28.9% in the RECOVER sample. Within the group of individuals with mental disorders, the proportion of unemployment varied according to the main diagnosis, with about a quarter unemployed among individuals with mood disorders (ICD-10 F3) or neurotic, stress-related and somatoform disorders (ICD-10 F4), and about half of the individuals diagnosed with disorders of adult personality and behavior (ICD-10 F6) (42.6%) or schizophrenia, schizotypal and delusional disorders (ICD-10 F2) (50%). Table S4 provides details on the share of unemployment by severity levels as well as information on the quantity of health care services used.
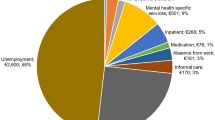
Excess costs
In total, the average 6-month excess costs of mental disorders amounted to 19,075 € (see Table 3). With 13,331 €, the share of indirect excess costs was considerably higher than the share of direct excess costs of 5744 €, mainly due to unemployment (8996 €). The main driver for direct excess costs was hospital/day care (5020 €). All estimated excess costs were statistically significant, with the exception of costs of services provided by other outpatient health care providers.
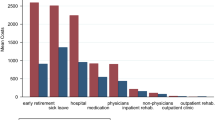
The analysis of excess costs by severity levels showed that the excess costs of mental disorders increased with increasing disease severity (see Table 4; Table S5 shows the corresponding mean costs for each severity level). In total, the excess costs ranged between 6123 € in level 1 and 31,883 € in level 4. This trend could be seen for direct excess costs (511 € to 10,485 €) and indirect excess costs (5612 € to 21,399 €). Except for direct excess costs in level 1, all previously reported excess costs were statistically significant. Hospital/day care services were the main driver for direct excess costs in the severity levels 2–4, and the excess costs of outpatient physicians were also statistically significant higher for these severity levels. In addition, higher severity levels (3 and 4) incurred statistically significantly higher costs of social/informal care compared to individuals without mental disorders. Again, indirect excess costs were the main contributor to total excess costs for all severity levels. Although the costs of unemployment were statistically significantly increased in all severity levels, the excess costs in levels 1 and 2 were still considerably lower than in the case of a severe course of the disease. As for early retirement, none of the individuals with mild disease severity (level 1) received disability pension. Therefore, the average marginal effects of mental disorders compared to the control group were not estimable, and only descriptive early retirement excess costs were reported (− 345 €). For the higher severity levels, the excess costs of early retirement again were increasing with disease severity, but the estimates were statistically significant only in the levels 3 and 4. The excess costs of sick leave were statistically significant for all severity levels, peaked in level 2 (3426 €), and then decreased to 1858 € in level 4, which would be consistent with the findings that a smaller proportion of persons was working in severity levels 3 and 4.
Subgroup analysis
The analysis by ICD-10 diagnosis groups showed that the excess costs also increased with higher disease severity levels within diagnosis groups (see Table 5).
In severity level 2, the diagnosis group neurotic, stress-related and somatoform disorders (ICD-10 F4) incurred the lowest total excess costs (7513 €) compared to mood disorders (ICD-10 F3) (10,622 €) or disorders of adult personality and behavior (ICD-10 F6) (11,840 €). In contrast, the total excess costs of these diagnosis groups were similarly high in severity level 3 and ranged from 24,195 € to 25,073 €. In level 4, the total excess costs were higher for the diagnosis group schizophrenia, schizotypal and delusional disorders (ICD-10 F2) (35,281 €) than for disorders of adult personality and behavior (ICD-10 F6) (29,154 €). For all subgroups, indirect excess costs were statistically significant and with a share of at least 69% the main contributor to total excess costs. The only subgroup without statistically significant direct excess costs was the diagnosis group disorders of adult personality and behavior (ICD-10 F6) in severity level 2.
Sensitivity analyses
The unadjusted excess costs in sensitivity analysis 1 (see Table S7) were in general slightly lower compared to the main analysis except for indirect excess costs, resulting from higher unemployment excess costs. In contrast to the main analysis, the unadjusted excess costs of rehabilitation and of social/informal care were not statistically significant, and the excess costs of other outpatient healthcare providers were negatively associated (− 17 €). In sensitivity analysis 2 without the costs of unemployment, the estimates were lower, but the direction and significance of the excess costs have not changed (see Table S7).
Discussion
Overall, mental disorders showed high excess costs, which increased with the levels of disease severity. Direct costs were 8.7-times higher and indirect costs were 8.4-times higher than for individuals without mental disorders. The study sample was mainly composed of individuals diagnosed with mood disorders (ICD-10 F3), neurotic, stress-related and somatoform disorders (ICD-10 F4), disorders of adult personality and behavior (ICD-10 F6), and schizophrenia, schizotypal and delusional disorders (ICD-F2), although the recruitment of study participants was open to different mental disorders. However, these diagnosis groups also appear in public statistics among the most frequent diagnoses in specialist departments for psychiatry and psychotherapy in Germany [59]. Another explanation for the fact that mood disorders and neurotic, stress-related and somatoform disorders, with a total of almost 70%, represent the majority of the study sample would be that these disorders have the highest prevalence of all mental disorders in the German population with 12-month prevalence rates of 9.8% and 24.8%, respectively [4]. The analysis by disease severity showed that direct and indirect costs increased with increasing severity levels. With mild disease severity, the differences in direct costs were not significant. However, with mild disease severity, indirect costs due to unemployment and sick leave were already significantly higher compared to individuals without mental disorders, indicating that measures relating to the working life could already be useful at a mild severity level. The findings that the excess costs of early retirement were only significant in moderate to severe severity might reflect that these groups already have a chronic course of illness since it takes some time to receive an early retirement pension. Overall, moderate to severe mental disorders incurred the highest direct excess costs. Furthermore, inpatient stays were the main contributor to direct excess costs, and considerably high in severity levels 3 and 4. Therefore, acute treatment options and a shift to the outpatient sector could be a resource-efficient approach in the interest of the patient. The high excess costs for social/informal care services in the severity levels 3 and 4 show that these patient groups need support in everyday life, which is often provided by relatives. The resulting burden for relatives should be taken into account in future research, and might be reduced by better mental health care for severe mental disorders.
To our knowledge, no study has yet evaluated the excess costs of mental disorders in Germany. The excess costs of mental disorders in our study are quite high (direct and indirect costs of mental disorders were 8.7-times and 8.4-times higher, respectively) compared to estimates on the 12-month excess costs of mental disorders in Austria, which reported 1.4-times higher direct and 2.6-times higher indirect costs [13]. In our study, the high excess costs were also evident at the level of primary diagnosis groups: For the most represented disorders, mood disorders (ICD-10 F3) and neurotic, stress-related and somatoform disorders (ICD-10 F4), direct costs were both 7.6-times higher, respectively and indirect costs were 7.2-times and 6.5-times higher, respectively compared to the control group. These findings were considerably higher compared to previous findings from meta-analyses [60, 61]. An explanation for the high excess costs could be that many study participants were directly recruited from an inpatient stay at the University Medical Center Hamburg-Eppendorf, which is also reflected in the estimated excess costs for hospital/day care. There were also many referrals from primary care physicians, but they possibly only referred patients who were severely affected by the disease. Furthermore, although the majority of the study participants had a diagnosis of mood disorders or neurotic, stress-related and somatoform disorders, almost one third of the included study participants were diagnosed with disorders of adult personality and behavior (ICD-10 F6) or schizophrenia, schizotypal and delusional disorders (ICD-10 F2) disorders that are known to be associated with high costs [12]. The study by Frey reported 9.5-times higher annual total costs of patients with schizophrenia compared to individuals without schizophrenia in Germany [16]. These estimates were still lower than the 6-month total excess costs of schizophrenia, schizotypal and delusional disorders (ICD-10 F2) in this study, which were estimated to be 13.2-times higher compared to individuals without mental disorders. This could possibly be due to the fact that many participants in our analysis belonged to severity level 4, and thus often had a very severe disease manifestation or were close to inpatient treatment.
In this study, the share of indirect costs in total costs was equal to 70%, and thus higher than the share of direct costs. By contrast, population-based estimates for Germany in 2010 reported a share of 41% of indirect costs in total costs [12]. This gap is mainly due to the additional consideration of the economic consequences of unemployment in our work, which is generally not assessed in cost-of-illness studies. Łaszewska and colleagues also estimated costs due to unemployment and reported a share of 48% of unemployment excess costs in total excess costs, which aligns with our findings [13]. Without the consideration of unemployment (sensitivity analysis 2), the share of indirect costs in total costs decreased to 45%, which is consistent with earlier studies that have assessed indirect costs without unemployment [12, 62]. A literature review showed that the share of indirect costs in the total costs of schizophrenia was 44% on average [62]. However, the amount of indirect costs depends strongly on the level of disease severity, and could be more than twice as high at a high severity level (GAF < 50) than for a low severity level (GAF ≥ 70) [63]. These findings support the high share of indirect costs in our analysis, since over 90% of the individuals with schizophrenia, schizotypal and delusional disorders (ICD-10 F2) were in severity level 4 (GAF ≤ 50).
Strengths and limitations
In this study, data from individuals with mental disorders were drawn from a RCT in the city of Hamburg in Northern Germany. A particular strength of this study was that the diagnoses were obtained in clinically structured interviews by experienced clinicians. This ensured higher data quality than with self-completed questionnaires, medical records or claims data from health insurance funds. The self-reported utilization of health care services and productivity losses were also assessed interview-based for a period of 6 months. For mental disorders in particular, it was shown that more cost categories were captured with survey data than with other data sources [64]. However, survey data are prone to recall bias and reporting bias, especially in the case of severe mental disorders. In addition, only complete cases were included in the analysis. In relation to the sample size, the proportion of excluded observations was higher in the group with severe mental illness than in the mild to moderate disease levels.
Another advantage of this study is that the individuals were insured in different major statutory health insurance funds, as differences between insurers were documented with regard to sociodemographic characteristics and morbidity [65]. However, not all statutory health insurance funds and no private insurance funds participated in the study, thus this study might be affected by selection bias. A large share of the individuals with mental disorders were recruited from the University Medical Center Hamburg-Eppendorf, which also poses the risk of selection bias (many severe cases and an underrepresentation of persons with undiagnosed mental disorders). In addition, due to the study design, not all diagnoses groups in the spectrum of mental disorders could have been included. On the one hand, persons with a primary diagnosis in the spectrum of organic, including symptomatic, mental disorders (ICD-10 F0) or mental and behavioral disorders due to psychoactive substance use (ICD-10 F1) were excluded due to the treatment options offered in the RECOVER study. On the other hand, the sample composition was open with regard to the diagnoses included, resulting in a heterogeneous group picture with a high proportion of mood disorders (ICD-10 F3), especially major depression. As a result, the representativeness of the study is limited, which limits the generalizability of our findings.
Another strength of this study was that the use of a comparison group allowed the calculation of excess costs, and thus a precise estimation of disease-related costs. We have balanced the control group using modern approaches. Yet, the data for the control group stem from another study setting and earlier survey period. The different interview modes might also have caused differences in the datasets. For example, it was shown that telephone interviews have a higher risk of social desirability bias than face-to-face interviews [66]. Moreover, it was not possible to estimate medication excess costs, as these were not collected in the control group. Despite for that, we have considered many cost categories and also evaluated unemployment in monetary terms, which has been rarely conducted for the evaluation of indirect costs. The high excess costs of unemployment showed that taking these costs into account for mental disorders is quite reasonable. However, the causal relationship of mental disorders with unemployment needs further clarification, since unemployment can also lead to mental disorders. Especially in the case of a mild disease severity, the causal relationship could be reversed, so that unemployment could have promoted the disease symptomology like depressive symptoms [67].
Conclusions
The excess costs of mental disorders in our study were high and increased by levels of disease severity. Based on the study setting, our findings showed that acute phases of illness substantially increased the costs associated with mental disorders compared to population-based estimates. Future research is needed to investigate, whether these findings are also reflected in other diagnosis groups that are underrepresented in this study, as well as in larger study samples in Germany. Cost-of-illness studies serving as the basis for policy interventions and decisions for mental disorders should take indirect costs and the levels of disease severity into account.
References
Mack S et al (2015) Functional disability and quality of life decrements in mental disorders: results from the mental health module of the german health interview and examination survey for adults (DEGS1-MH). Eur Psychiatry 30(6):793–800
Christensen MK et al (2020) The cost of mental disorders: a systematic review. Epidemiol Psychiatr Sci 29:e161
OECD & European Union, Health at a Glance: Europe 2018 State of Health in the EU Cycle (2018) OECD Publishing, Paris. https://doi.org/10.1787/health_glance_eur-2018-en
Jacobi F et al (2014) Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: the Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH). Int J Methods Psychiatr Res 23(3):304–319
Mack S et al (2014) Self-reported utilization of mental health services in the adult German population—evidence for unmet needs? Results of the DEGS1-Mental Health Module (DEGS1-MH). Int J Methods Psychiatr Res 23(3):289–303
OECD & European Union, Health at a Glance: Europe 2020: State of Health in the EU circle (2020) OECD Publishing, Paris. https://doi.org/10.1787/82129230-en
BPtK-BundesPsychotherapeutenKammer (2014) BPtK-Studie zur stationären Versorgung psychisch kranker Menschen
Sachverständigenrat (2018) Bedarfsgerechte Steuerung der Gesundheitsversorgung. Kurzfassung des Gutachtens 2018
Brieger P (2019) Psychiatrische Versorgung in Deutschland—ein Überblick. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz 62(2):121–127
Deutsche Gesellschaft für Psychiatrie und Psychotherapie, P.u.N.e.V. (2018) DGPPN-Standpunkte für eine zukunftsfähige Psychiatrie [cited 21/12/2021; Available from: https://www.dgppn.de/_Resources/Persistent/11a14679d449d3abc76fdd61fb7ff6c428310f67/DGPPN_Standpunktepapier%20web.pdf
Bower P, Gilbody S (2005) Stepped care in psychological therapies: access, effectiveness and efficiency: narrative literature review. Br J Psychiatry 186(1):11–17
Gustavsson A et al (2011) Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 21(10):718–779
Łaszewska A et al (2020) The excess economic burden of mental disorders: findings from a cross-sectional prevalence survey in Austria. Eur J Health Econ 21(7):1075–1089
Larg A, Moss JR (2011) Cost-of-illness studies: a guide to critical evaluation. Pharmacoeconomics 29(8):653–671
Akobundu E et al (2006) Cost-of-Illness studies: a review of common methods. Pharmacoeconomics 24(9):869–890
Frey S (2014) The economic burden of schizophrenia in Germany: a population-based retrospective cohort study using genetic matching. Eur Psychiatry 29(8):479–489
Dams J et al (2017) Excess costs of social anxiety disorder in Germany. J Affect Disord 213:23–29
Dams J et al (2018) Excess costs of alcohol-dependent patients in German psychiatric care compared with matched non-alcohol-dependent individuals from the general population: a secondary analysis of two datasets. BMJ Open 8(8):e020563
König H et al (2021) The excess costs of depression and the influence of sociodemographic and socioeconomic factors: results from the German Health Interview and Examination Survey for Adults (DEGS). Pharmacoeconomics 39(6):667–680
Lambert M et al (2020) Study protocol for a randomised controlled trial evaluating an evidence-based, stepped and coordinated care service model for mental disorders (RECOVER). BMJ Open 10(5):e036021
Grupp H, König H-H, Konnopka A (2016) Health care utilisation and costs in the general population in Germany. Health Policy 120(2):159–169
First MB et al (1997) Structured clinical interview for DSM-IV® axis ii personality disorders SCID-II. American Psychiatric Pub
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613
Löwe B et al (2004) Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord 81(1):61–66
Altman EG et al (1997) The Altman Self-Rating Mania Scale. Biol Psychiatry 42(10):948–955
Bandelow B (1999) Panic and Agoraphobia Scale (PAS). Hogrefe & Huber Publishers
Connor KM et al (2000) Psychometric properties of the Social Phobia Inventory (SPIN): new self-rating scale. Br J Psychiatry 176(4):379–386
Sosic Z, Gieler U, Stangier U (2008) Screening for social phobia in medical in- and outpatients with the German version of the Social Phobia Inventory (SPIN). J Anxiety Disord 22(5):849–859
Spitzer RL et al (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092–1097
Löwe B et al (2008) Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care 46(3):266–274
Goodman WK et al (1989) The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 46(11):1006–1011
Hand I, Büttner-Westphal H (1991) Die Yale-Brown Obsessive Compulsive Scale (Y-BOCS): Ein halbstrukturiertes Interview zur Beurteilung des Schweregrades von Denk- und Handlungszwängen. Verhaltenstherapie 1(3):223–225
Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP (2013) The PTSD Checklist for DSM-5 (PCL-5)
Krüger-Gottschalk A et al (2017) The German version of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): psychometric properties and diagnostic utility. BMC Psychiatry 17(1):379
Kroenke K, Spitzer RL, Williams JB (2002) The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 64(2):258–266
Löwe B et al (2004) Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord 78(2):131–140
Zimmermann J et al (2014) The structure and correlates of self-reported DSM-5 maladaptive personality traits: findings from two German-speaking samples. J Pers Disord 28(4):518–540
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13(2):261–276
Fairburn C, Cooper Z (1993) The eating disorder examination. In: Fairburn CG, Wilson GT, Schleimer K (eds) Binge eating: nature, assessment, and treatment. Guilford Press, New York
Hilbert A et al (2007) Eating disorder examination-questionnaire. Diagnostica 53(3):144–154
Kessler RC et al (2005) The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med 35(2):245–256
Bräunig P, Shugar G, Krüger S (1996) An investigation of the Self-Report Manic Inventory as a diagnostic and severity scale for mania. Compr Psychiatry 37(1):52–55
Guy W (1976) Clinical Global Impressions, in ECDEU assessment manual for psychopharmacology. US Department of Health, Education and Welfare, Public Health Service, Alcohol, Drug Abuse and Mental Health Administration
Aas IHM (2010) Global Assessment of Functioning (GAF): properties and frontier of current knowledge. Ann Gen Psychiatry 9:20–20
Seidl H et al (2015) [FIMA--questionnaire for health-related resource use in an elderly population: development and pilot study]. Gesundheitswesen (Bundesverband der Ärzte des Öffentlichen Gesundheitsdienstes (Germany)) 77(1):46–52
Grupp H et al (2018) FIMPsy—questionnaire for the assessment of medical and non medical resource utilisation in mental disorders: development and application. Psychiatr Prax 45(2):87–94
Bock JO et al (2015) [Calculation of standardised unit costs from a societal perspective for health economic evaluation]. Gesundheitswesen (Bundesverband der Ärzte des Öffentlichen Gesundheitsdienstes (Germany)) 77(1):53–61
Grupp H, König HH, Konnopka A (2017) [Calculation of Standardised Unit Costs for the Economic Evaluation of Mental Disorders]. Gesundheitswesen (Bundesverband der Ärzte des Öffentlichen Gesundheitsdienstes (Germany)) 79(1):48–57
Schöffski O, von der Schulenburg JMG (2008) Gesundheitsökonomische Evaluationen. Springer, Berlin Heidelberg
Pike J, Grosse SD (2018) Friction cost estimates of productivity costs in cost-of-illness studies in comparison with human capital estimates: a review. Appl Health Econ Health Policy 16(6):765–778
Helgesson M et al (2018) Trajectories of work disability and unemployment among young adults with common mental disorders. BMC Public Health 18(1):1228–1228
Mousteri V et al (2019) Adolescent mental health and unemployment over the lifespan: population evidence from Sweden. Soc Sci Med 222:305–314
Statistisches Bundesamt, Verdienste und Arbeitskosten (2018) Arbeitskosten im Produzierenden Gewerbe und im Dienstleistungsbereich- Ergebnisse für Deutschland—2016. Wiesbaden
Statistisches Bundesamt (2019) Verdienste und Arbeitskosten. Arbeitnehmerverdienste 2019. Wiesbaden
Deutsche Rentenversicherung. Erwerbsminderungsrenten. 2021 28.05.2021] Available from: https://www.deutsche-rentenversicherung.de/DRV/DE/Rente/Allgemeine-Informationen/Rentenarten-und-Leistungen/Erwerbsminderungsrente/erwerbsminderungsrente_node.html
Hainmueller J, Xu Y (2013) Ebalance: a stata package for entropy balancing. J Stat Softw. https://doi.org/10.18637/jss.v054.i07
Hainmueller J (2012) Entropy balancing for causal effects: a multivariate reweighting method to produce balanced samples in observational studies. Polit Anal 20(1):25–46
World Health Organization. Body mass index - BMI. Health Topics. Disease prevention. Nutrition. A healthy lifestyle. 2020 07.05.2020]; Available from: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi
Schulz H et al (2008) Psychotherapeutische Versorgung. Gesundheitsberichterstattung des Bundes. Heft 41
Konnopka A, König H (2020) Economic burden of anxiety disorders: a systematic review and meta-analysis. Pharmacoeconomics 38(1):25–37
König H, König HH, Konnopka A (2019) The excess costs of depression: a systematic review and meta-analysis. Epidemiol Psychiatr Sci 29:e30
Fasseeh A et al (2018) A systematic review of the indirect costs of schizophrenia in Europe. Eur J Public Health 28(6):1043–1049
Ekman M et al (2013) The societal cost of schizophrenia in Sweden. J Ment Health Policy Econ 16(1):13–25
Grupp H, König HH, Konnopka A (2014) Cost measurement of mental disorders in Germany. J Ment Health Policy Econ 17(1):3–8
Hoffmann F, Koller D (2017) Verschiedene Regionen, verschiedene Versichertenpopulationen? Soziodemografische und gesundheitsbezogene Unterschiede zwischen Krankenkassen. Gesundheitswesen (Bundesverband der Ärzte des Öffentlichen Gesundheitsdienstes (Germany)) 79(01):e1–e9
Jäckle A, Roberts C, Lynn P (2006) Telephone versus face-to-face interviewing: mode effects on data quality and likely causes: report on phase II of the ESS-Gallup mixed mode methodology project. ISER Working Paper Series
Pelzer B, Schaffrath S, Vernaleken I (2014) Coping with unemployment: the impact of unemployment on mental health, personality, and social interaction skills. Work 48(2):289–295
Funding
Open Access funding enabled and organized by Projekt DEAL. This research leading to these results received funding from the Innovation Fund of the Federal Joint Committee (G-BA) under Grant Agreement No. 01NVF16018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JG has received research funding from the German Federal Ministry of Education and Research, German Science Foundation, and speaker fees from Lundbeck, Janssen-Cilag, Lilly, Otsuka and Boehringer. ML has received consultant or speaker fees from AstraZeneca, Bristol-Myers Squibb, Lilly Deutschland GmbH, Janssen Cilag GmbH, Lundbeck GmbH, Otsuka Pharma GmbH, Roche Deutschland Holding GmbH, Sanovi Aventis, Trommsdorff GmbH & Co KG. AKW has received consultant or speaker fees from Lilly Deutschland GmbH, Janssen Cilag GmbH, Lundbeck GmbH, Otsuka Pharma GmbH, Roche Deutschland Holding GmbH.
Ethics approval
The RECOVER study has obtained ethics approval from the ethics committee of the Hamburg Medical Association (PV5672) have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The written consent of all participants was obtained prior to the study.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
This study includes only anonymized data. The study participants provided informed consent that anonymized study data will be used for publications.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
König, H., König, HH., Gallinat, J. et al. Excess costs of mental disorders by level of severity. Soc Psychiatry Psychiatr Epidemiol 58, 973–985 (2023). https://doi.org/10.1007/s00127-022-02298-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02298-8