Abstract
Background
Subjective hearing loss (SHL) refers to an individual’s self-assessment of their hearing loss. The association and underlying mechanisms between SHL and cognitive impairment still necessitate elucidation.
Objectives
To validate potential mechanisms between SHL and cognitive impairment.
Design
Cross-section.
Setting
Shanghai, China.
Participants
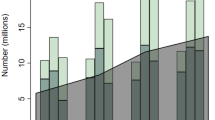
A total of 2369 individuals from communities and the cognitive disorder clinic.
Measurements
All participants were subjected to a comprehensive neuropsychological assessment, encompassing the Hearing Handicap Inventory for the Elderly-Screening Version (HHIE-S). The participants’ brain β-amyloid (Aβ) deposition status, plasma biomarkers associated with Alzheimer’s disease (AD), and cardiovascular risk factors were also collected.
Results
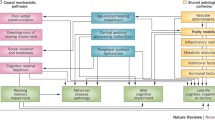
In individuals with a heightened SHL, elevated HHIE-S score was linked to diminished cognitive and daily functioning as well as heightened levels of depressed mood. This correlation was observed in auditory memory performance but not in visual memory. The influence of SHL on cognitive function was mediated by depressed mood. SHL was associated with diabetes and smoking, whereas cognitive function was associated with hyperlipidemia and alcohol consumption. In individuals with positive brain Aβ deposition, SHL demonstrated associations with cognitive function independent of plasma Aβ42/40 ratio, P-tau181, neurofilament light chain, and APOE allele status.
Conclusion
SHL has an independent effect on cognitive impairment. The findings do no provide evidence for the common cause mechanism. Instead, the findings support the presence of a cognitive resource mechanism and an impoverished environment mechanism, along with the potential for a pathological interaction mechanism.

Similar content being viewed by others
Data Availability: The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
GBD 2019 Hearing Loss Collaborators. Hearing loss prevalence and years lived with disability, 1990–2019: findings from the Global Burden of Disease Study 2019. Lancet. 2021;397(10278):996–1009. doi:https://doi.org/10.1016/S0140-6736(21)00516-X
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet. 2020;396(10248):413–446. doi:https://doi.org/10.1016/S0140-6736(20)30367-6
Uchida Y, Sugiura S, Nishita Y, Saji N, Sone M, Ueda H. Age-related hearing loss and cognitive decline — The potential mechanisms linking the two. Auris Nasus Larynx. 2019;46(1):1–9. doi:https://doi.org/10.1016/j.anl.2018.08.010
Golub JS, Brickman AM, Ciarleglio AJ, Schupf N, Luchsinger JA. Association of Subclinical Hearing Loss With Cognitive Performance. JAMA Otolaryngol Head Neck Surg. 2020;146(1):57–67. doi:https://doi.org/10.1001/jamaoto.2019.3375
Griffiths TD, Lad M, Kumar S, et al. How Can Hearing Loss Cause Dementia? Neuron. 2020;108(3):401–412. doi:https://doi.org/10.1016/j.neuron.2020.08.003
Kurata N, Schachern PA, Paparella MM, Cureoglu S. Histopathologic Evaluation of Vascular Findings in the Cochlea in Patients With Presbycusis. JAMA Otolaryngol Head Neck Surg. 2016;142(2):173–178. doi:https://doi.org/10.1001/jamaoto.2015.3163
Omata Y, Tharasegaran S, Lim YM, et al. Expression of amyloid-β in mouse cochlear hair cells causes an early-onset auditory defect in high-frequency sound perception. Aging (Albany NY). 2016;8(3):427–439. doi:https://doi.org/10.18632/aging.100899
Shityakov S, Hayashi K, Störk S, Scheper V, Lenarz T, Förster CY. The Conspicuous Link between Ear, Brain and Heart-Could Neurotrophin-Treatment of Age-Related Hearing Loss Help Prevent Alzheimer’s Disease and Associated Amyloid Cardiomyopathy? Biomolecules. 2021;11(6):900. doi:https://doi.org/10.3390/biom11060900
Förster CY, Shityakov S, Scheper V, Lenarz T. Linking Cerebrovascular Dysfunction to Age-Related Hearing Loss and Alzheimer’s Disease-Are Systemic Approaches for Diagnosis and Therapy Required? Biomolecules. 2022;12(11):1717. doi:https://doi.org/10.3390/biom12111717
Kim JS, Lee HJ, Lee S, et al. Conductive Hearing Loss Aggravates Memory Decline in Alzheimer Model Mice. Front Neurosci. 2020;14:843. doi:https://doi.org/10.3389/fnins.2020.00843
Zheng M, Yan J, Hao W, et al. Worsening hearing was associated with higher β-amyloid and tau burden in age-related hearing loss. Sci Rep. 2022;12(1):10493. doi:https://doi.org/10.1038/s41598-022-14466-6
Golub JS, Sharma RK, Rippon BQ, Brickman AM, Luchsinger JA. The Association Between Early Age-Related Hearing Loss and Brain β-Amyloid. Laryngoscope. 2021;131(3):633–638. doi:https://doi.org/10.1002/lary.28859
de Haan W, Mott K, van Straaten ECW, Scheltens P, Stam CJ. Activity dependent degeneration explains hub vulnerability in Alzheimer’s disease. PLoS Comput Biol. 2012;8(8):e1002582. doi:https://doi.org/10.1371/journal.pcbi.1002582
van Nifterick AM, Gouw AA, van Kesteren RE, Scheltens P, Stam CJ, de Haan W. A multiscale brain network model links Alzheimer’s disease-mediated neuronal hyperactivity to large-scale oscillatory slowing. Alzheimers Res Ther. 2022;14(1):101. doi:https://doi.org/10.1186/s13195-022-01041-4
Ittner LM, Ke YD, Delerue F, et al. Dendritic function of tau mediates amyloid-beta toxicity in Alzheimer’s disease mouse models. Cell. 2010;142(3):387–397. doi:https://doi.org/10.1016/j.cell.2010.06.036
Xu W, Zhang C, Li JQ, et al. Age-related hearing loss accelerates cerebrospinal fluid tau levels and brain atrophy: a longitudinal study. Aging (Albany NY). 2019;11(10):3156–3169. doi:https://doi.org/10.18632/aging.101971
Parker T, Cash DM, Lane C, et al. Pure tone audiometry and cerebral pathology in healthy older adults. J Neurol Neurosurg Psychiatry. 2020;91(2):172–176. doi:https://doi.org/10.1136/jnnp-2019-321897
Sarant JZ, Harris DC, Busby PA, et al. No Influence of Age-Related Hearing Loss on Brain Amyloid-β. J Alzheimers Dis. 2022;85(1):359–367. doi:https://doi.org/10.3233/JAD-215121
Tuwaig M, Savard M, Jutras B, et al. Deficit in Central Auditory Processing as a Biomarker of Pre-Clinical Alzheimer’s Disease. J Alzheimers Dis. 2017;60(4):1589–1600. doi:https://doi.org/10.3233/JAD-170545
Wang HF, Zhang W, Rolls ET, et al. Hearing impairment is associated with cognitive decline, brain atrophy and tau pathology. EBioMedicine. 2022;86:104336. doi:https://doi.org/10.1016/j.ebiom.2022.104336
Armstrong NM, An Y, Doshi J, et al. Association of Midlife Hearing Impairment With Late-Life Temporal Lobe Volume Loss. JAMA Otolaryngol Head Neck Surg. 2019;145(9):794–802. doi:https://doi.org/10.1001/jamaoto.2019.1610
Ray J, Popli G, Fell G. Association of Cognition and Age-Related Hearing Impairment in the English Longitudinal Study of Ageing. JAMA Otolaryngol Head Neck Surg. 2018;144(10):876–882. doi:https://doi.org/10.1001/jamaoto.2018.1656
Lin FR, Albert M. Hearing loss and dementia - who is listening? Aging Ment Health. 2014;18(6):671–673. doi:https://doi.org/10.1080/13607863.2014.915924
Lichtenstein MJ, Bess FH, Logan SA. Validation of screening tools for identifying hearing-impaired elderly in primary care. JAMA. 1988;259(19):2875–2878.
Torre P, Moyer CJ, Haro NR. The accuracy of self-reported hearing loss in older Latino-American adults. Int J Audiol. 2006;45(10):559–562. doi:https://doi.org/10.1080/14992020600860935
Videhult Pierre P, Johnson AC, Fridberger A. Subjective and Clinically Assessed Hearing Loss; A Cross-Sectional Register-Based Study on a Swedish Population Aged 18 through 50 Years. PLoS One. 2015;10(4):e0123290. doi:https://doi.org/10.1371/journal.pone.0123290
Zhao X, Zhou Y, Wei K, et al. Associations of sensory impairment and cognitive function in middle-aged and older Chinese population: The China Health and Retirement Longitudinal Study. J Glob Health. 2021;11:08008. doi:https://doi.org/10.7189/jogh.11.08008
Vaccaro R, Zaccaria D, Colombo M, Abbondanza S, Guaita A. Adverse effect of self-reported hearing disability in elderly Italians: Results from the InveCe.Ab study. Maturitas. 2019;121:35–40. doi:https://doi.org/10.1016/j.maturitas.2018.12.009
Matthews K, Dawes P, Elliot R, Pendleton N, Tampubolon G, Maharani A. Trajectories of self-reported hearing and their associations with cognition: evidence from the United Kingdom and United States of America. Age Ageing. 2023;52(2):afad017. doi:https://doi.org/10.1093/ageing/afad017
Cui L, Huang L, Pan FF, et al. Chinese Preclinical Alzheimer’s Disease Study (C-PAS): Design and Challenge from PET Acceptance. J Prev Alz Dis. Published online 2023. doi:https://doi.org/10.14283/jpad.2023.49
Pan FF, Wang Y, Huang L, Huang Y, Guo QH. Validation of the Chinese version of Addenbrooke’s cognitive examination III for detecting mild cognitive impairment. Aging Ment Health. 2022;26(2):384–391. doi:https://doi.org/10.1080/13607863.2021.1881757
Huang L, Chen KL, Lin BY, et al. Chinese version of Montreal Cognitive Assessment Basic for discrimination among different severities of Alzheimer’s disease. Neuropsychiatr Dis Treat. 2018;14:2133–2140. doi:https://doi.org/10.2147/NDT.S174293
Farias ST, Mungas D, Reed BR, et al. The measurement of everyday cognition (ECog): scale development and psychometric properties. Neuropsychology. 2008;22(4):531–544. doi:https://doi.org/10.1037/0894-4105.22.4.531
Cui L, Zhang Z, Guo Y, Li Y, Xie F, Guo Q. Category Switching Test: A Brief Amyloid-β-Sensitive Assessment Tool for Mild Cognitive Impairment. Assessment. Published online April 20, 2023:10731911231167537. doi:https://doi.org/10.1177/10731911231167537
Zhao Q, Guo Q, Hong Z. Clustering and switching during a semantic verbal fluency test contribute to differential diagnosis of cognitive impairment. Neurosci Bull. 2013;29(1):75–82. doi:https://doi.org/10.1007/s12264-013-1301-7
Knesevich JW, LaBarge E, Edwards D. Predictive value of the Boston Naming Test in mild senile dementia of the Alzheimer type. Psychiatry Res. 1986;19(2):155–161. doi:https://doi.org/10.1016/0165-1781(86)90008-9
Zhao Q, Guo Q, Liang X, et al. Auditory Verbal Learning Test is Superior to Rey-Osterrieth Complex Figure Memory for Predicting Mild Cognitive Impairment to Alzheimer’s Disease. Curr Alzheimer Res. 2015;12(6):520–526. doi:https://doi.org/10.2174/1567205012666150530202729
Benedict RHB, Schretlen D, Groninger L, Dobraski M, Shpritz B. Revision of the Brief Visuospatial Memory Test: Studies of normal performance, reliability, and validity. Psychological Assessment. 1996;8(2):145–153. doi:https://doi.org/10.1037/1040-3590.8.2.145
Zhao Q, Guo Q, Li F, Zhou Y, Wang B, Hong Z. Application of a new variant of the Trail making test. PLoS One. 2013;8(2):e57333. doi:https://doi.org/10.1371/journal.pone.0057333
Chen K, Huang L, Lin B, Zhou Y, Zhao Q, Guo Q. The Number of Items on Each Stroop Test Card Is Unrelated to Its Sensitivity. Neuropsychobiology. 2019;77(1):38–44. doi:https://doi.org/10.1159/000493553
Corruble E, Legrand JM, Zvenigorowski H, Duret C, Guelfi JD. Concordance between self-report and clinician’s assessment of depression. J Psychiatr Res. 1999;33(5):457–465. doi:https://doi.org/10.1016/s0022-3956(99)00011-4
Miebach L, Wolfsgruber S, Polcher A, et al. Which features of subjective cognitive decline are related to amyloid pathology? Findings from the DELCODE study. Alzheimers Res Ther. 2019;11(1):66. doi:https://doi.org/10.1186/s13195-019-0515-y
Li Q, Sun X, Cui L, et al. Alterations in metamemory capacity and neural correlates in a subtype of subjective cognitive decline. Neuroimage Clin. 2022;36:103255. doi:https://doi.org/10.1016/j.nicl.2022.103255
Li Q, Pan FF, Huang Q, Lo CYZ, Xie F, Guo Q. Altered metamemory precedes cognitive impairment in subjective cognitive decline with positive amyloid-beta. Front Aging Neurosci. 2022;14:1046445. doi:https://doi.org/10.3389/fnagi.2022.1046445
Jessen F, Wolfsgruber S, Kleineindam L, et al. Subjective cognitive decline and stage 2 of Alzheimer disease in patients from memory centers. Alzheimers Dement. Published online April 22, 2022. doi:https://doi.org/10.1002/alz.12674
Bondi MW, Edmonds EC, Jak AJ, et al. Neuropsychological criteria for mild cognitive impairment improves diagnostic precision, biomarker associations, and progression rates. J Alzheimers Dis. 2014;42(1):275–289. doi:https://doi.org/10.3233/JAD-140276
McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–269. doi:https://doi.org/10.1016/j.jalz.2011.03.005
Ren S, Li J, Huang L, et al. Brain Functional Alterations and Association with Cognition in People with Preclinical Subjective Cognitive Decline and Objective Subtle Cognitive Difficulties. Neuroscience. 2023;513:137–144. doi:https://doi.org/10.1016/j.neuroscience.2023.01.004
Pan F, Huang Y, Cai X, et al. Integrated algorithm combining plasma biomarkers and cognitive assessments accurately predicts brain β-amyloid pathology. Commun Med. 2023;3(1):65. doi:https://doi.org/10.1038/s43856-023-00295-9
Rosseel Y. lavaan: An R Package for Structural Equation Modeling. J Stat Soft. 2012;48(2). doi:https://doi.org/10.18637/jss.v048.i02
Kim S, Park JM, Han JS, et al. Age-related hearing loss in the Korea National Health and Nutrition Examination Survey. PLoS One. 2020;15(12):e0243001. doi:https://doi.org/10.1371/journal.pone.0243001
Wang D, Zhang H, Ma H, Zhang L, Yang L, Xu L. Hearing threshold levels and hearing loss among people in Zhejiang, China: a population-based cross-sectional study. BMJ Open. 2019;9(4):e027152. doi:https://doi.org/10.1136/bmjopen-2018-027152
Cui L, Zhang Z, Huang L, Li Q, Guo YH, Guo QH. Dual-stage cognitive assessment: a two-stage screening for cognitive impairment in primary care. BMC Psychiatry. 2023;23(1):368. doi:https://doi.org/10.1186/s12888-023-04883-w
Cohen MA, Horowitz TS, Wolfe JM. Auditory recognition memory is inferior to visual recognition memory. Proc Natl Acad Sci U S A. 2009;106(14):6008–6010. doi:https://doi.org/10.1073/pnas.0811884106
Cohen MA, Evans KK, Horowitz TS, Wolfe JM. Auditory and visual memory in musicians and nonmusicians. Psychon Bull Rev. 2011;18(3):586–591. doi:https://doi.org/10.3758/s13423-011-0074-0
Gloede ME, Paulauskas EE, Gregg MK. Experience and information loss in auditory and visual memory. Q J Exp Psychol (Hove). 2017;70(7):1344–1352. doi:https://doi.org/10.1080/17470218.2016.1183686
Schmid C, Büchel C, Rose M. The neural basis of visual dominance in the context of audio-visual object processing. Neuroimage. 2011;55(1):304–311. doi:https://doi.org/10.1016/j.neuroimage.2010.11.051
Tarawneh HY, Jayakody DMP, Sohrabi HR, Martins RN, Mulders WHAM. Understanding the Relationship Between Age-Related Hearing Loss and Alzheimer’s Disease: A Narrative Review. J Alzheimers Dis Rep. 2022;6(1):539–556. doi:https://doi.org/10.3233/ADR-220035
Gagné JP, Besser J, Lemke U. Behavioral Assessment of Listening Effort Using a Dual-Task Paradigm. Trends Hear. 2017;21:2331216516687287. doi:https://doi.org/10.1177/2331216516687287
Ponticorvo S, Manara R, Pfeuffer J, et al. Cortical pattern of reduced perfusion in hearing loss revealed by ASL-MRI. Hum Brain Mapp. 2019;40(8):2475–2487. doi:https://doi.org/10.1002/hbm.24538
Amieva H, Ouvrard C, Meillon C, Rullier L, Dartigues JF. Death, Depression, Disability, and Dementia Associated With Self-reported Hearing Problems: A 25-Year Study. J Gerontol A Biol Sci Med Sci. 2018;73(10):1383–1389. doi:https://doi.org/10.1093/gerona/glx250
Samocha-Bonet D, Wu B, Ryugo DK. Diabetes mellitus and hearing loss: A review. Ageing Res Rev. 2021;71:101423. doi:https://doi.org/10.1016/j.arr.2021.101423
Li P, Pang K, Zhang R, Zhang L, Xie H. Prevalence and risk factors of hearing loss among the middle-aged and older population in China: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. Published online July 13, 2023. doi:https://doi.org/10.1007/s00405-023-08109-3
Cruickshanks KJ, Klein R, Klein BE, Wiley TL, Nondahl DM, Tweed TS. Cigarette smoking and hearing loss: the epidemiology of hearing loss study. JAMA. 1998;279(21):1715–1719. doi:https://doi.org/10.1001/jama.279.21.1715
Zhang M, Qu T, Liu S, et al. Ethylbenzene induces hearing loss by triggering mitochondrial impairments and excess apoptosis in cochlear progenitor cells via suppressing the Wnt/β-catenin signaling. Ecotoxicol Environ Saf. 2023;254:114721. doi:https://doi.org/10.1016/j.ecoenv.2023.114721
Deal JA, Jiang K, Rawlings A, et al. Hearing, β-amyloid deposition and cognitive test performance in Black and White older adults: the ARIC-PET Study. J Gerontol A Biol Sci Med Sci. Published online July 7, 2023:glad159. doi:https://doi.org/10.1093/gerona/glad159
Nadhimi Y, Llano DA. Does hearing loss lead to dementia? A review of the literature. Hear Res. 2021;402:108038. doi:https://doi.org/10.1016/j.heares.2020.108038
Neff RM, Jicha G, Hawk GS, Bush ML, McNulty B. Association of Subjective Hearing Loss and Apolipoprotein E ε4 Allele on Alzheimer’s Disease Neurodegeneration. Otol Neurotol. 2021;42(1):e15–e21. doi:https://doi.org/10.1097/MAO.0000000000002855
Wang R, Reddy PH. Role of Glutamate and NMDA Receptors in Alzheimer’s Disease. J Alzheimers Dis. 2017;57(4):1041–1048. doi:https://doi.org/10.3233/JAD-160763
Beckmann D, Feldmann M, Shchyglo O, Manahan-Vaughan D. Hippocampal Synaptic Plasticity, Spatial Memory, and Neurotransmitter Receptor Expression Are Profoundly Altered by Gradual Loss of Hearing Ability. Cereb Cortex. 2020;30(8):4581–4596. doi:https://doi.org/10.1093/cercor/bhaa061
van’ tHooft JJ, Pelkmans W, Tomassen J, et al. Distinct disease mechanisms may underlie cognitive decline related to hearing loss in different age groups. J Neurol Neurosurg Psychiatry. 2023;94(4):314–320. doi:https://doi.org/10.1136/jnnp-2022-329726
Acknowledgments
This study was funded by the National Natural Science Foundation of China (82171198), Shanghai Municipal Science and Technology Major Project (2018SHZDZX01), Shanghai Municipal Health Commission (202140042), and Guangdong Provincial Key S&T Program (2018B030336001). We would like to thank Jie-Hua Zhu, Xian-Qing Xie, and Yun Yang for their help with neuropsychological tests.
Author information
Authors and Affiliations
Contributions
Author Contributions: LC and QHG contributed to the conception and design of the study; YYT, ZZ, YHG, FX, and QHG contributed to the acquisition and analysis of data; LC and YHG contributed to drafting the text and preparing the figures. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest: The authors declare that they have no conflict of interest.
Ethical standards: The study was reviewed and approved by the Ethics Committee of Shanghai Sixth People’s Hospital (approval number 2019-032). It was performed in accordance with the principles of the Declaration of Helsinki. All participants provided written informed consent to participate in the study.
Additional information
How to cite this article: L. Cui, Y.-Y. Tu, Z. Zhang, et al. Associations and Potential Multiple Mechanisms between Subjective Hearing Loss and Cognitive Impairment. J Prev Alz Dis 2024; https://doi.org/10.14283/jpad.2024.62
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Cui, L., Tu, YY., Zhang, Z. et al. Associations and Potential Multiple Mechanisms between Subjective Hearing Loss and Cognitive Impairment. J Prev Alzheimers Dis (2024). https://doi.org/10.14283/jpad.2024.62
Received:
Accepted:
Published:
DOI: https://doi.org/10.14283/jpad.2024.62