Abstract
Introduction
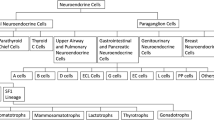
Presacral neuroendocrine neoplasms (PNENs) are rare tumors, with limited data on management and outcomes.
Methods
A retrospective review of institutional medical records was conducted to identify all patients with PNENs between 2008 and 2022. Data collection included demographics, symptoms, imaging, surgical approaches, pathology, complications, and long-term outcomes.
Results
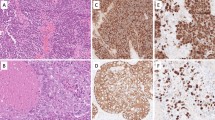
Twelve patients were identified; two-thirds were female, averaging 44.8 years of age, and, for the most part, presenting with back pain, constipation, and abdominal discomfort. Preoperative imaging included computed tomography scans and magnetic resonance images, with somatostatin receptor imaging and biopsies being common. Half of the patients had metastatic disease on presentation. Surgical approach varied, with anterior, posterior, and combined techniques used, often involving muscle transection and coccygectomy. Short-term complications affected one-quarter of patients. Pathologically, PNENs were mainly well-differentiated grade 2 tumors with positive synaptophysin and chromogranin A. Associated anomalies were common, with tail-gut cysts prevalent. Mean tumor diameter was 6.3 cm. Four patients received long-term adjuvant therapy. Disease progression necessitated additional interventions, including surgery and various chemotherapy regimens. Skeletal, liver, thyroid, lung, and pancreatic metastases occurred during follow-up, with no mortality reported. Kaplan–Meier analysis showed a 5-year local recurrence rate of 23.8%, disease progression rate of 14.3%, and de novo metastases rate of 30%.
Conclusion
The study underscores the complex management of PNENs and emphasizes the need for multicenter research to better understand and manage these tumors. It provides valuable insights into surgical outcomes, recurrence rates, and overall survival, guiding future treatment strategies for PNEN patients.



Similar content being viewed by others
References
Ghosh J, Eglinton T, Frizelle FA, Watson AJ. Presacral tumours in adults. Surgeon. 2007;5(1):31–8.
Jao SW, Beart RW Jr, Spencer RJ, Reiman HM, Ilstrup DM. Retrorectal tumors. Mayo Clinic experience, 1960–1979. Dis Colon Rectum. 1985;28(9):644–52.
Hobson KG, Ghaemmaghami V, Roe JP, Goodnight JE, Khatri VP. Tumors of the retrorectal space. Dis Colon Rectum. 2005;48(10):1964–74.
Messick CA, Hull T, Rosselli G, Kiran RP. Lesions originating within the retrorectal space: a diverse group requiring individualized evaluation and surgery. J Gastrointest Surg. 2013;17(12):2143–52.
Spencer RJ, Jackman RJ. Surgical management of precoccygeal cysts. Surg Gynecol Obstet. 1962;115:449–52.
Kelley SR, Dozois EJ. Presacral Tumors. In: SR Steele, TL Hull, N Hyman, JA Maykel, TE Read, CB Whitlow, editors. The ASCRS Textbook of Colon and Rectal Surgery. Cham: Springer International Publishing; 2022. p. 375–96.
Thiis-Evensen E, Boyar Cetinkaya R. Incidence and prevalence of neuroendocrine neoplasms in Norway 1993–2021. J Neuroendocrinol. 2023;35(4):e13264.
Das S, Dasari A. Epidemiology, incidence, and prevalence of neuroendocrine neoplasms: Are there global differences? Curr Oncol Rep. 2021;23(4):43.
Korse CM, Taal BG, van Velthuysen ML, Visser O. Incidence and survival of neuroendocrine tumours in the Netherlands according to histological grade: experience of 2 decades of cancer registry. Eur J Cancer. 2013;49(8):1975–83.
Hallet J, Law CH, Cukier M, Saskin R, Liu N, Singh S. Exploring the rising incidence of neuroendocrine tumors: a population-based analysis of epidemiology, metastatic presentation, and outcomes. Cancer. 2015;121(4):589–97.
White BE, Rous B, Chandrakumaran K, Wong K, Bouvier C, Van Hemelrijck M, et al. Incidence and survival of neuroendocrine neoplasia in England 1995–2018: a retrospective, population-based study. Lancet Reg Health Eur. 2022;23:100510.
Taal BG, Visser O. Epidemiology of neuroendocrine tumours. Neuroendocrinology. 2004;80(Suppl 1):3–7.
Matrood S, Apostolidis L, Schrader J, Krug S, Lahner H, Ramaswamy A, et al. Multicenter analysis of presacral neuroendocrine neoplasms-clinicopathological characterization and treatment outcomes of a rare disease. Front Endocrinol (Lausanne). 2021;12:709256.
Lloyd RV. Practical markers used in the diagnosis of neuroendocrine tumors. Endocr Pathol. 2003;14(4):293–301.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Glasgow SC, Birnbaum EH, Lowney JK, Fleshman JW, Kodner IJ, Mutch DG, et al. Retrorectal tumors: a diagnostic and therapeutic challenge. Dis Colon Rectum. 2005;48(8):1581–7.
Yang G, Dhall D, Yu R, Tuli R, Amersi FF, Friedman ML, et al. The Clinicopathological aspects of primary presacral neuroendocrine neoplasms: one center experience. Pancreas. 2018;47(1):122–9.
Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934–59.
Zhong W, You C, Chen H, Huang S. Primary presacral carcinoid tumor with gluteal muscle metastasis. Neurol India. 2012;60(5):544–5.
Dujardin F, Beaussart P, de Muret A, Rosset P, Waynberger E, Mulleman D, de Pinieux G. Primary neuroendocrine tumor of the sacrum: case report and review of the literature. Skeletal Radiol. 2009;38(8):819–23.
Fiandaca MS, Ross WK, Pearl GS, Bakay RA. Carcinoid tumor in a presacral teratoma associated with an anterior sacral meningocele: case report and review of the literature. Neurosurgery. 1988;22(3):581–8.
Mullaney TG, Lightner AL, Johnston M, Kelley SR, Larson DW, Dozois EJ. A systematic review of minimally invasive surgery for retrorectal tumors. Tech Coloproctol. 2018;22(4):255–63.
Luong TV, Salvagni S, Bordi C. Presacral carcinoid tumour. Review of the literature and report of a clinically malignant case. Dig Liver Dis. 2005;37(4):278–81.
Chatani S, Onaya H, Kato S, Inaba Y. Adenocarcinoma and neuroendocrine tumor arising within presacral teratoma associated with Currarino syndrome: a case report. Indian J Radiol Imaging. 2019;29(3):327–31.
Colombo F, Janous P, Buxton N. Carcinoid transformation of presacral dermoid cyst in patient with currarino syndrome: a case report. Br J Neurosurg. 2019;33(3):285–6.
Coetzee E, Malaka S. Malignant neuroendocrine tumour in an adult female diagnosed with Currarino syndrome. S Afr J Surg. 2019;57(4):44.
Pendlimari R, Leonard D, Dozois EJ. Rare malignant neuroendocrine transformation of a presacral teratoma in patient with Currarino syndrome. Int J Colorectal Dis. 2010;25(11):1383–4.
Correa Bonito A, Maqueda González R, Rodríguez Sánchez A, Bermejo Marcos E, Blanco Terés L, García Septiem J, Martín Pérez E. Presacral neuroendocrine tumour in a patient diagnosed with Currarino’s syndrome. Gastroenterol Hepatol. 2022;45(Suppl 1):62–3.
Scott AT, Tessmann JB, Braun T, Brown B, Breheny PJ, Darbro BW, et al. Presacral neuroendocrine tumors associated with the Currarino syndrome. Am J Med Genet A. 2021;185(5):1582–8.
Liu AJ, Halfdanarson TR, Sonbol MB. Currarino syndrome: a rare condition with potential connection to neuroendocrine tumors. Pancreas. 2020;49(8):1104–8.
Angelini A, Ruggieri P. A new surgical technique (modified Osaka technique) of sacral resection by posterior-only approach: description and preliminary results. Spine (Phila Pa 1976). 2013;38(3):E185–92.
Broccard SP, Colibaseanu DT, Behm KT, Mishra N, Davis P, Maimone KL, et al. Risk of malignancy and outcomes of surgically resected presacral tailgut cysts: a current review of the Mayo Clinic experience. Colorectal Dis. 2022;24(4):422–7.
Del Rivero J, Perez K, Kennedy EB, Mittra ES, Vijayvergia N, Arshad J, et al. Systemic therapy for tumor control in metastatic well-differentiated gastroenteropancreatic neuroendocrine tumors: ASCO guideline. J Clin Oncol. 2023;41(32):5049–67.
Caplin ME, Pavel M, Ćwikła JB, Phan AT, Raderer M, Sedláčková E, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224–33.
Rinke A, Müller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656–63.
Kim MR, Shim HK. Long-term follow-up of a patient with primary presacral neuroendocrine tumor: a case report with literature review. Am J Case Rep. 2019;20:1969–75.
Falkmer UG, Gustafsson T, Wenzel R, Wierup N, Sundler F, Kulkarni H, et al. Malignant presacral ghrelinoma with long-standing hyperghrelinaemia. Ups J Med Sci. 2015;120(4):299–304.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of (177)Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125–35.
Brabander T, van der Zwan WA, Teunissen JJM, Kam BLR, Feelders RA, de Herder WW, et al. Long-term efficacy, survival, and safety of [(177)Lu-DOTA(0), Tyr(3)]octreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors. Clin Cancer Res. 2017;23(16):4617–24.
Ballal S, Yadav MP, Tripathi M, Sahoo RK, Bal C. Survival outcomes in metastatic gastroenteropancreatic neuroendocrine tumor patients receiving concomitant (225)Ac-DOTATATE targeted alpha therapy and capecitabine: a real-world scenario management based long-term outcome study. J Nucl Med. 2022. https://doi.org/10.2967/jnumed.122.264043.
Delpassand ES, Tworowska I, Esfandiari R, Torgue J, Hurt J, Shafie A, Núñez R. Targeted α-emitter therapy with (212)Pb-DOTAMTATE for the treatment of metastatic SSTR-expressing neuroendocrine tumors: first-in-humans dose-escalation clinical trial. J Nucl Med. 2022;63(9):1326–33.
Yao JC, Fazio N, Singh S, Buzzoni R, Carnaghi C, Wolin E, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968–77.
Chan J, Geyer S, Ou FS, Knopp M, Behr S, Zemla T, et al. LBA53 Alliance A021602: Phase III, double-blinded study of cabozantinib versus placebo for advanced neuroendocrine tumors (NET) after progression on prior therapy (CABINET). Ann Oncol. 2023;34:S1292.
Pusceddu S, Prinzi N, Tafuto S, Ibrahim T, Filice A, Brizzi MP, et al. Association of upfront peptide receptor radionuclide therapy with progression-free survival among patients with enteropancreatic neuroendocrine tumors. JAMA Netw Open. 2022;5(2):e220290.
Gudmundsdottir H, Habermann EB, Vierkant RA, Starlinger P, Thiels CA, Warner SG, et al. Survival and symptomatic relief after cytoreductive hepatectomy for neuroendocrine tumor liver metastases: long-term follow-up evaluation of more than 500 patients. Ann Surg Oncol. 2023;30(8):4840–51.
Funding
This research did not receive external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Thorvardur Halfdanarson has received research support from Thermo Fisher Scientific, Advanced Accelerator Applications (a Novartis company), Camurus, Crinetics, and ITM Isotopen Technologien Muenchen. He has also undertaken consultancy/advisory board/steering committee work for Ipsen, TerSera, Advanced Accelerator Applications (a Novartis company), Terumo, ITM Isotopen Technologien Muenchen, Crinetics, Perspective Therapeutics, and Camurus. Tommaso Violante, Brenda Murphy, Davide Ferrari, Rondell P. Graham, Patrick Navin, Amit Merchea, David W. Larson, Eric J. Dozois, and William R. Perry have no conflicts of interest to disclose in relation to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Violante, T., Murphy, B., Ferrari, D. et al. Presacral Neuroendocrine Neoplasms: A Multi-site Review of Surgical Outcomes. Ann Surg Oncol (2024). https://doi.org/10.1245/s10434-024-15328-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1245/s10434-024-15328-3