Abstract
Background
Although addition of adjuvant chemotherapy is the current standard, the prognosis of pancreatic cancers still remains poor. The NEPAFOX trial evaluated perioperative treatment with FOLFIRINOX in resectable pancreatic cancer.
Patients and Methods
This multicenter phase II trial randomized patients with resectable or borderline resectable pancreatic cancer without metastases into arm (A,) upfront surgery plus adjuvant gemcitabine, or arm (B,) perioperative FOLFIRINOX. The primary endpoint was overall survival (OS).
Results
Owing to poor accrual, recruitment was prematurely stopped after randomization of 40 of the planned 126 patients (A: 21, B: 19). Overall, approximately three-quarters were classified as primarily resectable (A: 16, B: 15), and the remaining patients were classified as borderline resectable (A: 5, B: 4). Of the 12 evaluable patients, 3 achieved partial response under neoadjuvant FOLFIRINOX. Of the 21 patients in arm A and 19 patients in arm B, 17 and 7 underwent curative surgery, and R0-resection was achieved in 77% and 71%, respectively. Perioperative morbidity occurred in 72% in arm A and 46% in arm B, whereas non-surgical toxicity was comparable in both arms. Median RFS/PFS was almost doubled in arm B (14.1 months) compared with arm A (8.4 months) in the population with surgical resection, whereas median OS was comparable between both arms.
Conclusions
Although the analysis was only descriptive owing to small patient numbers, no safety issues regarding surgical complications were observed in the perioperative FOLFIRINOX arm. Thus, considering the small number of patients, perioperative treatment approach appears feasible and potentially effective in well-selected cohorts of patients. In pancreatic cancer, patient selection before initiation of neoadjuvant therapy appears to be critical.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pancreatic ductal adenocarcinoma (PDAC) is one of the malignant tumors with the highest mortality. The 5-year overall survival for all pancreatic cancers including all stages was approximately 11% in the US population from 2011 to 2017.1 Resection with curative intent followed by adjuvant chemotherapy represents the current standard of care. However, more than 80% of all patients with PDAC are not eligible for curative surgery because of the presence of distant metastasis and/or locally advanced disease at the time of diagnosis.
Despite substantial improvements in pancreatic surgery and effective adjuvant treatment options with more powerful chemotherapy (CTX) regimens over the last years, even tumors with an upfront clearly resectable situation still have an unfavorable prognosis. Furthermore, the overall recurrence rate is as high as 85% and most recurrences occur as systemic liver metastasis early in the course, with a median disease-free survival of only 6.7 months.2 Thus, there may be a need for early implementation of a systemic therapy component.3
Neoadjuvant or perioperative multimodal therapies have significantly improved pathological response as well as overall outcome of resectable gastroesophageal junction and gastric adenocarcinomas.4,5 Immediate systemic therapy has been adopted as a neoadjuvant approach in borderline resectable PDAC on the basis of the findings of several randomized controlled trials (RCTs) demonstrating its survival benefit.6,7,8,9 Nowadays, neoadjuvant approach is accepted in the National Comprehensive Cancer Network guideline in pancreatic borderline resectable cases in which the cancer is not clearly resectable with upfront surgery because the R+ surgery rate is high without upfront therapy. It is reasonable to assume that systemic chemotherapy and/or radiochemotherapy prior to surgery may have a similar impact on the outcome of resectable PDAC.
Neoadjuvant treatment (NAT) strategy also emerged as an option even in resectable PDAC because of its potential benefits, including immediate treatment of undetectable micrometastases. Furthermore, neoadjuvant treatment enables anticancer therapy that is not hampered by postoperative complications, which are the reason nearly half of the patients with PDAC cannot receive adjuvant therapeutic approaches.10 However, NAT may also be associated with a potential loss of eligibility for curative resection owing to tumor growth during therapy. Presurgical attrition occurs in approximately 30% of patients with resectable PDAC, suggesting the possibility of selection bias in studies showing the benefits of NAT.10,11 Since there are still conflicting results on survival gain compared with upfront surgery, the real effectiveness of NAT in resectable PDAC remains unclear.12,13,14 Recently pooled data from three randomized controlled trials of NAT for resectable PDAC suggest that this approach should be accepted as new standard of care.15 Nevertheless, neoadjuvant treatment of PDAC is currently still considered an experimental approach. The current standard of care is surgical resection followed by adjuvant CTX with either gemcitabine or a combination CTX, e.g., gemcitabine and capecitabine.16
Overall, the data provided a strong rationale to evaluate the efficacy and safety of neoadjuvant treatment with FOLFIRINOX (FFX) in patients with resectable PDAC.
Patients and Methods
Study Design and Participants
This was an investigator-initiated multicenter, randomized, unblinded, controlled phase II trial. All versions of the trial protocol were approved by the Ethik-Kommission der Landesärztekammer Hessen ethics committee and subsequently by the respective ethics committees of each of the participating centers. The trial is registered with ClinicalTrials.gov (no. NCT02172976). The trial was conducted in accordance with the Declaration of Helsinki. All patients provided written informed consent to participate in this trial.
Patients with histologically confirmed adenocarcinoma of the pancreas were included. For histological confirmation, a maximum of three attempts was allowed. The tumor had to be radiological confirmed as locally limited, resectable [primarily resectable or borderline situation according to the National Comprehensive Cancer Network (NCCN) classification criteria] without distant metastases. Further, the main inclusion criteria were age ≤ 75 years; Eastern Cooperative Oncology Group (ECOG) performance status ≤ 1; adequate hematological, hepatic, and renal function parameters; normal cardiac ejection fraction; no prior pancreas resection; and no prior cytostatic chemotherapy.
Patients were centrally randomized in a 1:1 ratio to the standard treatment arm (A) with upfront surgery followed by six cycles adjuvant gemcitabine (1000 mg/m2 on days 1, 8, and 15 on a 28-day cycle) or to the experimental arm (B) with perioperative FFX [irinotecan 180 mg/m2, oxaliplatin 85 mg/m2, 5-fluorouracil (5-FU) 400 mg/m2 bolus, 5-FU 2400 mg/m2, and sodium folinate 400 mg/m2] on day 1 on a 14-day cycle for 4–6 cycles pre- as well as post-surgery. In arm B, filgrastim should be applied if necessary on days 5–7 of every cycle. Therapy was terminated prematurely for unacceptable toxicity, disease progression, death, or upon patient request. In arm B, surgery was scheduled 4–6 weeks after the last dose of neoadjuvant FFX. The surgeon was responsible for the selection of the adequate oncological resection technique. Centers with experienced pancreatic surgery departments (or established collaboration with such departments) were selected for this trial and the surgery reports were centrally reviewed by an experienced surgeon (T.O.G.).
Radiological examinations [chest computed tomography (CT) and abdominal CT or magnetic resonance imaging (MRI)] were performed before the start of the study and in arm B after the third preoperative cycle and before surgery to assess operability.
Randomization
Randomization was performed by an interactive web response system (IWRS) on the basis of a sequence generated with permuted blocks and stratified by ECOG performance status (0 vs 1) and resectability (primarily clearly resectable versus borderline resectable). Patients were enrolled by authorized individuals who requested randomization using IWRS integrated in the electronic Case Report Forms (eCRF). Actual assignment to trial groups took place on the server of the independent data management providers (Trium Analysis Online, Munich, Germany) by means of a validated SAS program, which underlies strict access control. The randomization system allocated a unique identification number to every patient and sent a message that included the allocation result to the investigator. The study was open label and no masking was required.
Study Endpoints
The primary endpoint was overall survival (OS), defined as time from randomization until death from any cause. Secondary endpoints included recurrence/progression-free survival (RFS/PFS), defined as time from randomization until disease recurrence/progression under preoperative CTX, until evidence of recurrence (after surgery had been performed), or death from any cause. Secondary endpoints were perioperative morbidity and mortality, R0 resection rate, and feasibility and tolerability of FOLFIRINOX with regard to the use of G-CSF/filgrastim in primary prophylaxis.
Statistical Analysis
The initial sample size calculation was based on the median survival of 22.1 months for patients treated with adjuvant gemcitabine within the CONCO-001 trial2 and the median survival of 18.8 months for patients treated with neoadjuvant gemcitabine.17 Patients with borderline resectable tumors, who were also enrolled in this trial, have a worse survival. Therefore, a median survival of 18 months in the standard adjuvant gemcitabine arm was assumed. Neoadjuvant/adjuvant chemotherapy with FFX was expected to improve median survival with a clinically relevant hazard ratio (HR) of 0.68. Taking into account a dropout rate of 15%, an alpha error of 0.15 (one-sided log-rank test), and a power of 80%, a total of 126 patients at a 1:1 randomization were needed. However, recruitment of the trial was stopped after 40 patients owing to poor accrual.
The intention-to-treat (ITT) population was defined as all patients randomized to participate in the study. The curative surgery population was defined as all patients who are randomized and received radical oncological pancreatic surgery. The curative surgery population was defined by the coordinating investigator on the basis of the surgery reports and database entries.
All parameters were evaluated and reported in an explorative or descriptive manner. The Kaplan–Meier method was used to estimate the distribution of time to event variables. Summaries included the number and percentages of events per treatment group, the median, and 25% and 75% quantiles of survival time as well as the proportion of patients without event at certain timepoints. Event-related data were estimated by the product limit method providing the numbers of events and censored cases, median survival time along with its 95% CI, and compared using the log rank test. Patients without any documentation of events, lost to follow-up, or with early dropout were censored at last observation, i.e., the date of last tumor assessment for progression-free survival and last known survival date for overall survival. Incomplete time-to-event observations were handled as censored measurements and missing data were considered as failure for the primary endpoint.
The analyses were carried out using SAS software.
Results
Between 5 March 2015 and 23 March 2018, 40 patients were randomly assigned to the phase II part of the NEPAFOX trial. Furthermore, 21 patients were assigned to arm A, with direct upfront surgery without preoperative chemotherapy followed by adjuvant gemcitabine CTX (SOC- arm), and 19 patients were assigned to experimental arm B, with neoadjuvant FFX followed by surgery and adjuvant FFX. After inclusion of the 40 patients into the phase II part of the trial, the NEPAFOX trial was prematurely stopped owing to poor accrual.
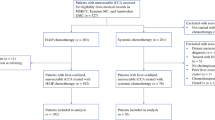
Baseline characteristics, including age, sex, and ECOG performance status, were similar between both arms. Before randomization, 76.2% of the patients in arm A and 78.9% in arm B were classified as primarily resectable, and the remaining patients were classified as borderline resectable. Jaundice was present at baseline in 33.3% (n = 7) of patients in arm A and 42.1% (n = 8) of patients in arm B. Of the seven patients with jaundice in adjuvant gemcitabine arm, four (57.1%) received presurgical stenting, and seven of the eight patients with jaundice in the perioperative FFX arm (87.5%) received biliary stenting (Fig. 1).
The median time from randomization until the start of systemic neoadjuvant therapy in arm B was 11 days (range 2–29 days), indicating a delay of tumor therapy that was most likely caused by interventional procedures to enable patients’ neoadjuvant approach, such as diagnostic histological tumor confirmation or biliary stenting. In arm A, 13 patients (62%) began the adjuvant systemic gemcitabine treatment (62%), with a median of three cycles applied. All 19 patients (100%) randomized to arm B started neoadjuvant FFX chemotherapy, with a median of 6.0 FFX cycles applied (pre- and postoperatively). Of 19 patients who started with FFX, 11 (57.9%) completed the recommended six preoperative cycles. Five patients (26%) started postoperative chemotherapy, with four completing all recommended cycles (21% of total population; Fig. 1) (Table 1).
Overall, 156 and 166 adverse events (AEs) were reported in arm A and arm B, respectively, and the incidence of AEs grade ≥ 3 was higher in arm B (57% versus 84%). However, only two AEs in arm A and one in arm B with grade ≥ 3 were classified as treatment related. The most common AEs with grades 1–2 (> 20%) were diarrhea and fatigue in both arms, fever in arm A, and anorexia, dizziness, and nausea in arm B. The most common AEs with grade ≥ 3 (< 5%) were neutropenia in arm A and abdominal pain, biliary tract infection, diarrhea, GGT increase, and sepsis in arm B (Table 2). One fatal serious adverse event (SAE) that was classified as related to the treatment was reported in arm A (hepatic failure) and two nonrelated fatal SAEs (both sepsis) occurred in arm B.
G-CSF was administered in the first cycle in the perioperative FFX arm in 12 patients (63.1%), with 4 (33%) experiencing a delay in the FFX schedule. Only one of these four patients had a delay in schedule owing to neutropenia (Table S1). Of the remaining seven patients who did not receive upfront G-CSF in cycle 1, three (37%) showed a dose delay, with one of them due to neutropenia. Of 19 patients in the perioperative FFX arm, 2 (10.5%) received iron substitution, each in cycle 2 of the neoadjuvant treatment (Table 3).
According to RECIST 1.1, none of the patients in the perioperative FFX arm achieved complete response after completion of the neoadjuvant treatment. Three patients (15.8%) showed partial response, six patients (31.6%) showed stable disease, and three patients (15.8%) had signs of tumor progression. For seven patients (36.8%), response evaluation according to RECIST was not conducted, and three of these patients showed clinically progressive disease and did not proceed to surgery (Table 4). One patient with progressive disease following RECIST underwent surgery, but only liver metastases were resected. Overall, 18 patients (85.7%) in arm A and 11 patients (57.9%) in arm B proceeded to surgery. Reasons for not conducting surgery were patient’s wish and detection of local irresectability before surgery in arm A, as well as disease progression in arm B (Fig. 1). Of all patients undergoing surgery, 17 patients (94%) in arm A and 7 patients (64%) in arm B received radical tumor surgery, including pancreatic tumor resection and lymph node dissection. R0 resection was achieved in 5 of the 7 (76.5%) patients in arm A and in 13 of the 17 (71.4%) patients in arm B. Perioperative morbidity rate in all patients who underwent any kind of surgery was 72.2% in arm A and 45.5% in arm B. There were no relevant differences within the local and systemic complications between both arms (Table 4).
Within the ITT population, the median OS was increased in arm A compared with arm B [25.68 months (95% CI 11.74, –) versus 10.03 months (95% CI 6.25–27.95)]. The median RFS/PFS was 9.8 months (95% CI 4.44–19.76) in arm A and 6.64 months (95% CI 2.50–11.84) in arm B (HR 0.722; Fig. 2). However, within the population of patients who received curative surgery, median OS was comparable between both arms [arm A: 25.68 months (95% CI 11.74, –); arm B: 22.55 months (95% CI 6.25, –); HR 1.054]. Furthermore, median RFS/PFS was numerically increased in the patients receiving neoadjuvant FFX [arm A: 8.38 months (95% CI 4.27, –), arm B: 14.14 months (95% CI 6.25, –; Fig. 2)].
Discussion
Robust data based on phase III RCTs established the adjuvant therapy approach for pancreatic cancer treatment. These data have been shown to improve survival, but only for patients who are fit enough after surgery. Unfortunately, a subset of patients who undergo upfront surgery do not recover adequately to be able to receive adjuvant treatment. Thus, about 45% of patients scheduled for adjuvant chemotherapy after surgical resection do not receive it owing to poor performance status, postoperative morbidity, or early disease progression.18,19 In addition, the majority of data regarding perioperative tumor therapy show a definite survival benefit of chemotherapy in both the neoadjuvant and adjuvant settings compared with data of no perioperative chemotherapy.
The results of NEPAFOX show a shorter median survival in the perioperative FFX arm compared with the adjuvant gemcitabine standard arm in the intention-to-treat population, presumably because fewer patients received surgery for a variety of reasons. Thus, within the limits of this defined trial population, FFX neoadjuvant treatment was not shown to provide longer survival than upfront surgery followed by adjuvant gemcitabine. However, almost all patients in the standard arm A without neoadjuvant treatment, but only one-third of the patients who received neoadjuvant FFX treatment in arm B, underwent curative surgery. The main reason for not conducting surgery for patients in arm B was progression under neoadjuvant treatment. Among these patients who received curative resection, the use of perioperative FFX compared with adjuvant gemcitabine alone resulted in an almost doubling of RFS/PFS (14.1 months vs 8.4 months) and no difference in OS. The results are in line with previous data showing median disease free-survival ranging between 10 months and 17 months for perioperative chemotherapy in resectable PDA.20,21,22 Thus, the results of the NEPAFOX underlines patient selection for neoadjuvant therapy.
Several trials have been performed to assess neoadjuvant chemotherapy for pancreatic resectable disease. However, most of the early trials were only cohort trials and used older single-agent chemotherapy regimens, plus or minus radiation.23,24,25,26,27,28,29,30,31,32,33 Recent pooled data from three randomized controlled phase II trials, however, suggested that neoadjuvant therapy for resectable pancreatic cancer could be the new standard of care15
During the conduct of the NEPAFOX trial, the results of the PRODIGE 24/CCTG PA.6 phase III trial were published, demonstrating that the modified FFX significantly increased the efficacy in the adjuvant setting compared with gemcitabine monotherapy. Furthermore, the mFFX regimen was superior to gemcitabine monotherapy in all subgroups analyzed, including patients with advanced T3/4 tumors, N+ tumors, and even after R1 resection.34 In addition, the gemcitabine only treatment achieved a 10–15-month longer overall survival compared with previous trials evaluating adjuvant gemcitabine, which was likely owing to the high use of FFX after relapse in the gemcitabine arm.34 The PRODIGE 24/CCTG PA.6 trial was therefore the first, and so far the only, study providing such a benefit in a group with positive surgical margins. However, it must be noted that the median age of 63 years in this trial suggests that the majority of patients included were younger than the average population of patients with PDAC, e.g., 69 years in 600 patients of the QOLIXANE trial.35
In addition, despite the promising results for adjuvant treatment, it is important to note that only about 60% of patients with PDAC receive adjuvant treatment in real-world settings owing to perioperative morbidity, even when the start of adjuvant treatment is delayed up to 3 months postoperatively.36 Therefore, trial populations of adjuvant studies are highly selected patients.
One-quarter of the NEPAFOX population was defined as borderline resectable, and while adjuvant chemotherapy remains the standard approach for primarily resectable pancreatic cancers, borderline resectable or even locally advanced pancreatic cancers are increasingly treated with neoadjuvant chemotherapy.37,38 The intention of neoadjuvant chemotherapy in borderline resectable pancreatic cancer is, on the one hand, to decrease tumor size for an easier resection of the primary tumor and to achieve an R0 resection, and on the other hand, to biologically select patients without tumor progression under upfront systemic therapy who will benefit from subsequent radical tumor surgery. Previous trials have even shown favorable outcomes after a neoadjuvant approach followed by surgery, although post-neoadjuvant imaging suggested a persistent unresectability. This indicates that surgical evaluation will always be an option when surgical intervention is the only possibility to cure a patient and achieve long-term survival.37,39
Despite the promising increase in RFS/PFS in the curative resected population under perioperative FFX treatment, the use of FFX in the neoadjuvant situation is not entirely unproblematic. If the neoadjuvant concept fails, a potent therapy for the then palliative situation has already been exhausted. In addition, one must also be aware that in resectable pancreatic cancers, neoadjuvant therapy could lead to a delay of the required surgery, especially when patients suffer complications from the neoadjuvant systemic therapy. As such, cholestasis could lead to the need of biliary stenting, enabling patients to receive a cytotoxic therapy and provoke a further delay of surgery. According to the current guidelines, surgery of pancreatic cancer can be performed without prior histological confirmation.40,41 However, histological confirmation of the primary tumor with a need of a positive biopsy is required before the start of a systemic therapy, especially neoadjuvant systemic chemotherapy. This often turns out to be not so succinct, because unlike, for example, the relatively simple biopsy of liver metastasis in stage IV disease, biopsy of primary pancreatic metastasis is always required in clear curative situations.42 In up to 25% of cases there is no sufficient material obtainable even after repeated endoscopic-ultrasound-guided fine needle aspiration, and therefore surgery gets delayed without even the option of the planned neoadjuvant chemotherapy treatment being initiated.43 Furthermore, the histological structure of the primary pancreatic cancer with dense stromal character may limit the effectiveness of upfront chemotherapy on the primary cancer.44 Thus, patient selection is critical for neoadjuvant treatment to reduce the risk of neoadjuvant concept fails that would limit remaining treatment options.
Thus, the rationale of a potential benefit owing to early systemic treatment in the form of a neoadjuvant treatment should be weighed against the complications and toxicity of the treatment potentially affecting perioperative morbidity and even mortality. In our trial, no increase in toxicity regarding surgical complications in the neoadjuvant treatment arm compared with the standard arm were observed.
Data Availability
The data underlying this article will be available from the corresponding author upon reasonable request.
References
NIH National Cancer Institute. Surveillance, epidemiology, and end results (SEER) program; 2022. https://seer.cancer.gov/statfacts/html/pancreas.html. Accessed Jan 2023.
Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310(14):1473–81. https://doi.org/10.1001/jama.2013.279201.
Roth MT, Berlin JD. Current concepts in the treatment of resectable pancreatic cancer. Curr Oncol Rep. 2018;20(5):39. https://doi.org/10.1007/s11912-018-0685-y.
Al-Batran S-E, Hofheinz RD, Pauligk C, et al. Histopathological regression after neoadjuvant docetaxel, oxaliplatin, fluorouracil, and leucovorin versus epirubicin, cisplatin, and fluorouracil or capecitabine in patients with resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4-AIO): results from the phase 2 part of a multicentre, open-label, randomised phase 2/3 trial. Lancet Oncol. 2016;17(12):1697–708. https://doi.org/10.1016/s1470-2045(16)30531-9.
Al-Batran S-E, Homann N, Pauligk C, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393(10184):1948–57. https://doi.org/10.1016/s0140-6736(18)32557-1.
Jang JY, Han Y, Lee H, et al. Oncological benefits of neoadjuvant chemoradiation with gemcitabine versus upfront surgery in patients with borderline resectable pancreatic cancer: a prospective, randomized, open-label, multicenter phase 2/3 trial. Ann Surg. 2018;268(2):215–22. https://doi.org/10.1097/sla.0000000000002705.
Katz MHG, Shi Q, Meyers J, et al. Efficacy of preoperative mFOLFIRINOX vs mFOLFIRINOX plus hypofractionated radiotherapy for borderline resectable adenocarcinoma of the pancreas: the A021501 phase 2 randomized clinical trial. JAMA Oncol. 2022;8(9):1263–70. https://doi.org/10.1001/jamaoncol.2022.2319.
van Dam JL, et al. Neoadjuvant therapy or upfront surgery for resectable and borderline resectable pancreatic cancer: a meta-analysis of randomised controlled trials. Eur J Cancer. 2022;160:140–9. https://doi.org/10.1016/j.ejca.2021.10.023.
Versteijne E, Suker M, Groothuis K, et al. Preoperative chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer: results of the Dutch randomized phase III PREOPANC trial. J Clin Oncol. 2020;38(16):1763–73. https://doi.org/10.1200/jco.19.02274.
Wolff RA. Adjuvant or neoadjuvant therapy in the treatment in pancreatic malignancies: where are we? Surg Clin North Am. 2018;98(1):95–111. https://doi.org/10.1016/j.suc.2017.09.009.
Heinrich S. Neoadjuvant therapy for pancreatic ductal adenocarcinoma-real effects or patient selection? Hepatobiliary Surg Nutr. 2018;7(4):289–91. https://doi.org/10.21037/hbsn.2018.03.11.
Gillen S, Schuster T, Meyer Zum Büschenfelde C, Friess H, Kleeff J. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010;7(4):e1000267. https://doi.org/10.1371/journal.pmed.1000267.
Lee YS, Lee J-C, Yang SY, Kim J, Hwang J-H. Neoadjuvant therapy versus upfront surgery in resectable pancreatic cancer according to intention-to-treat and per-protocol analysis: a systematic review and meta-analysis. Sci Rep. 2019;9(1):15662–15662. https://doi.org/10.1038/s41598-019-52167-9.
Xu CP, Xue XJ, Liang N, Xu DG, Liu FJ, Yu XS, Zhang JD. Effect of chemoradiotherapy and neoadjuvant chemoradiotherapy in resectable pancreatic cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2014;140(4):549–59. https://doi.org/10.1007/s00432-013-1572-4.
Birrer DL, Golcher H, Casadei R, et al. Neoadjuvant therapy for resectable pancreatic cancer: a new standard of care pooled data from 3 randomized controlled trials. Ann Surg. 2021;274(5):713–20. https://doi.org/10.1097/sla.0000000000005126.
Neoptolemos JP, Palmer DH, Ghaneh P, et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet. 2017;389(10073):1011–24. https://doi.org/10.1016/s0140-6736(16)32409-6.
Andriulli A, Festa V, Botteri E, et al. Neoadjuvant/preoperative gemcitabine for patients with localized pancreatic cancer: a meta-analysis of prospective studies. Ann Surg Oncol. 2012;19(5):1644–62. https://doi.org/10.1245/s10434-011-2110-8.
Mayo SC, Gilson MM, Herman JM, et al. Management of patients with pancreatic adenocarcinoma: national trends in patient selection, operative management, and use of adjuvant therapy. J Am Coll Surg. 2012;214(1):33–45. https://doi.org/10.1016/j.jamcollsurg.2011.09.022.
Merkow RP, Bilimoria KY, Tomlinson JS, et al. Postoperative complications reduce adjuvant chemotherapy use in resectable pancreatic cancer. Ann Surg. 2014;260(2):372–7. https://doi.org/10.1097/sla.0000000000000378.
Seufferlein T, Uhl W, Kornmann M, et al. Perioperative or only adjuvant gemcitabine plus nab-paclitaxel for resectable pancreatic cancer (NEONAX)—a randomized phase II trial of the AIO pancreatic cancer group. Ann Oncol. 2023;34(1):91–100. https://doi.org/10.1016/j.annonc.2022.09.161.
Sohal DPS, Duong M, Ahmad SA, et al. Efficacy of perioperative chemotherapy for resectable pancreatic adenocarcinoma: a phase 2 randomized clinical trial. JAMA Oncol. 2021;7(3):421–7. https://doi.org/10.1001/jamaoncol.2020.7328.
Tempero MA, Pelzer U, O’Reilly EM, et al. Adjuvant nab-paclitaxel + gemcitabine in resected pancreatic ductal adenocarcinoma: results from a randomized, open-label, phase III trial. J Clin Oncol. 2023;41(11):2007–19. https://doi.org/10.1200/JCO.22.01134.
Evans DB, Varadhachary GR, Crane CH, et al. Preoperative gemcitabine-based chemoradiation for patients with resectable adenocarcinoma of the pancreatic head. J Clin Oncol. 2008;26(21):3496–502. https://doi.org/10.1200/jco.2007.15.8634.
Golcher H, Brunner TB, Witzigmann H, et al. Neoadjuvant chemoradiation therapy with gemcitabine/cisplatin and surgery versus immediate surgery in resectable pancreatic cancer: results of the first prospective randomized phase II trial. Strahlenther Onkol. 2015;191(1):7–16. https://doi.org/10.1007/s00066-014-0737-7.
Grose D, McIntosh D, Jamieson N, et al. The role of induction chemotherapy + chemoradiotherapy in localised pancreatic cancer: initial experience in Scotland. J Gastro Oncol. 2017;8(4):683–95. https://doi.org/10.21037/jgo.2017.04.01.
Heinrich S, Pestalozzi BC, Schäfer M, et al. Prospective phase II trial of neoadjuvant chemotherapy with gemcitabine and cisplatin for resectable adenocarcinoma of the pancreatic head. J Clin Oncol. 2008;26(15):2526–31. https://doi.org/10.1200/jco.2007.15.5556.
Motoi F, Unno M. Neoadjuvant treatment for resectable pancreatic adenocarcinoma: what is the best protocol? Ann Gastroenterol Surg. 2020;4(2):100–8. https://doi.org/10.1002/ags3.12311.
O’Reilly EM, Perelshteyn A, Jarnagin WR, et al. A single-arm, nonrandomized phase II trial of neoadjuvant gemcitabine and oxaliplatin in patients with resectable pancreas adenocarcinoma. Ann Surg. 2014;260(1):142–8. https://doi.org/10.1097/SLA.0000000000000251.
Sahani DV, Kambadakone A, Macari M, Takahashi N, Chari S, Fernandez-del Castillo C. Diagnosis and management of cystic pancreatic lesions. AJR Am J Roentgenol. 2013;200(2):343–54. https://doi.org/10.2214/ajr.12.8862.
Tajima H, Ohta T, Kitagawa H, et al. Pilot study of neoadjuvant chemotherapy with gemcitabine and oral S-1 for resectable pancreatic cancer. Exp Ther Med. 2012;3(5):787–92. https://doi.org/10.3892/etm.2012.482.
Talamonti MS, Small W Jr, Mulcahy MF, et al. A multi-institutional phase II trial of preoperative full-dose gemcitabine and concurrent radiation for patients with potentially resectable pancreatic carcinoma. Ann Surg Oncol. 2006;13(2):150–8. https://doi.org/10.1245/aso.2006.03.039.
Turrini O, Viret F, Moureau-Zabotto L, et al. Neoadjuvant 5 fluorouracil-cisplatin chemoradiation effect on survival in patients with resectable pancreatic head adenocarcinoma: a ten-year single institution experience. Oncology. 2009;76(6):413–9. https://doi.org/10.1159/000215928.
Motoi F, Kosuge T, Ueno H, et al. Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP05). Jpn J Clin Oncol. 2019;49(2):190–4. https://doi.org/10.1093/jjco/hyy190.
Conroy T, Hammel P, Hebbar M, et al. FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med. 2018;379(25):2395–406. https://doi.org/10.1056/NEJMoa1809775.
Al-Batran S-E, Hofheinz R-D, Reichart A, et al. Quality of life and outcome of patients with metastatic pancreatic cancer receiving first-line chemotherapy with nab-paclitaxel and gemcitabine: real-life results from the prospective QOLIXANE trial of the platform for outcome, quality of life and translational research on pancreatic cancer registry. Int J Cancer. 2021;148(6):1478–88. https://doi.org/10.1002/ijc.33336.
Deutsche Krebsgesellschaft. Jahresbericht der zertifizierten Pankreaskarzinomzentren—Kennzahlenauswertung 2018. Available online: www.krebsgesellschaft.de/jahresberichte.html. Accessed Jan 2023.
Ferrone CR, Marchegiani G, Hong TS. Radiological and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann Surg. 2015;261(1):12–7. https://doi.org/10.1097/sla.0000000000000867.
Khorana AA, Mangu PB, Berlin J, et al. Potentially curable pancreatic cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017;35(20):2324–8. https://doi.org/10.1200/jco.2017.72.4948.
Wagner M, Antunes C, Pietrasz D, et al. CT evaluation after neoadjuvant FOLFIRINOX chemotherapy for borderline and locally advanced pancreatic adenocarcinoma. Eur Radiol. 2017;27(7):3104–16. https://doi.org/10.1007/s00330-016-4632-8.
Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. S3-Leitlinie zum exokrinen Pankreaskarzinom. (Version 1.0); 2013.
Seufferlein T. Guidelines and expert consensus in the ZfG. Z Gastroenterol. 2014;52(2):179. https://doi.org/10.1055/s-0033-1356390.
Haeberle L, Esposito I. Pathology of pancreatic cancer. Transl Gastroenterol Hepatol. 2019;4:50. https://doi.org/10.21037/tgh.2019.06.02.
Hewitt MJ, McPhail MJ, Possamai L, Dhar A, Vlavianos P, Monahan KJ. EUS-guided FNA for diagnosis of solid pancreatic neoplasms: a meta-analysis. Gastrointest Endosc. 2012;75(2):319–31. https://doi.org/10.1016/j.gie.2011.08.049.
Verbeke C, Löhr M, Karlsson JS, Del Chiaro M. Pathology reporting of pancreatic cancer following neoadjuvant therapy: challenges and uncertainties. Cancer Treat Rev. 2015;41(1):17–26. https://doi.org/10.1016/j.ctrv.2014.11.002.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was financially supported by Vifor Pharma Deutschland GmbH, medac GmbH (Wedel, Germany), and Pfizer Pharma GmbH (initially Hospira, Berlin, Germany). The funders had no influence on the collection, analysis, interpretation of data, or the design of the study. Moreover, the writing of the manuscript was not influenced by the companies.
Author information
Authors and Affiliations
Contributions
TOG and SEA had the original idea, designed the study, and were responsible for the protocol development. UB and CP were responsible for the project management. UB and ML wrote the manuscript. UB, ML, and TOG performed the literature search and prepared figures and tables. All authors except UB, CP, and ML recruited patients into the study and collected data. All authors contributed to data interpretation and revising the manuscript. TOG and SEA had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Disclosure
Thorsten O. Goetze consults for Amgen, AstraZeneca, Bayer, BMS, Daiichi Sankyo, Foundation One Medicine, Lilly, MCI, MSD, Novartis, Roche, and Boehringer and received honoraria from Amgen, BMS, Lilly, MSD, Novartis, Roche, and GSK. Wolf O. Bechstein received honoraria from Astellas, Charité Berlin, CHIESI, Deutscher Ärzteverlag, Else-Kröner-Stiftung, European Society for Organ Transplantation, Falk Foundation, GORE, MCI, Novartis, Sanofi, Sirtex, and Terumo. Gabriele M. Siegler consults for AstraZeneca, BMS, Janssen-Cilag, Novartis; receives honoraria from Aurikamed, BMS, Deutsche Röntgengesellschaft, Eisai, Janssen-Cilag, Konzept Pharma, Roche; research grants from Novartis and Nutricia; and travel grants from Amgen, Novarti, and Servier. Salah-Eddin Al-Batran is the CEO/funder of Institut für Klinische Krebsforschung IKF; is on the advisory board of BMS, Immutep, Lilly, MacroGenics, and MSD; received research grants from Astra-Zeneca, BMS, Celgene, Eurozyto, Hospira, Immutep, Ipsen, Lilly, Medac, MSD, Roche, Sanofi, and Vifor; and is a speaker for AIO Studien gGmbH, BMS, Lilly, and MCI. Marino Venerito received honoraria for speaker, consultancy, advisory role, and/or research grants from Servier, Roche, BMS, MSD, EISAI, Bayer, Lilly, AstraZeneca, Merck Serono, Sirtex, Ipsen, Nordic Pharma, and Amgen. Ulli Bankstahl, Claudia Pauligk, Maria Loose, and Nils Homann have no conflicts of interest to declare. Possible conflicts of other authors tbn.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goetze, T.O., Reichart, A., Bankstahl, U.S. et al. Adjuvant Gemcitabine Versus Neoadjuvant/Adjuvant FOLFIRINOX in Resectable Pancreatic Cancer: The Randomized Multicenter Phase II NEPAFOX Trial. Ann Surg Oncol 31, 4073–4083 (2024). https://doi.org/10.1245/s10434-024-15011-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-024-15011-7