Abstract
Background
For some patients with colorectal liver metastases (CRLMs), surgical resection of all visible disease can lead to long-term survival and even cure. When complete resection is not feasible, microwave ablation (MWA) can help achieve hepatic disease control. As modern 2.45-GHz MWA generators gain popularity, the characteristics of tumors most likely to benefit from this method remain unclear. This study aimed to evaluate local recurrence (LR) rates, patterns of recurrence, and factors contributing to treatment failure after 2.45-GHz MWA of CRLM.
Methods
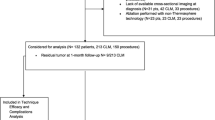
Patients with CRLM who underwent operative 2.45-GHz MWA between 2011 and 2019 were identified in a prospectively maintained single-institution database. Recurrence outcomes were ascertained for each lesion by imaging review. Factors associated with LR were analyzed.
Results
The study enrolled 184 patients bearing 416 ablated tumors. Most of the patients (65.8%) had high clinical risk scores (3–5), and 165 (90%) underwent concurrent liver resection. The median tumor size was 10 mm. After a median follow-up period of 28.8 months, LR was observed in 45 tumors, and the cumulative incidence of LR at 24 months was 10.9% (95% confidence interval [CI], 8.0–14.3%]. In 7%, LR was the first recurrence site, often combined with recurrence elsewhere. The cumulative incidence of LR at 24 months was 6.8% (95% CI 3.8–11.0%) for tumors 10 mm in size or smaller, 12.4% (95% CI 7.8–18.1%) for tumors 11 to 20 mm in size, and 30.2% (95% CI 14.2–48.0%) for tumors larger than 20 mm. In the multivariable analysis, tumors larger than 20 mm with a subcapsular location were significantly associated with increased LR risk.
Conclusions
Treatment of CRLM with 2.45-GHz MWA offers excellent local control at 2 years and is most successful for small tumors deep within the parenchyma.



Similar content being viewed by others
References
Fong Y, Fortner J, Sun RL, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18 (discussion 318–21).
House MG, Ito H, Gönen M, et al. Survival after hepatic resection for metastatic colorectal cancer: trends in outcomes for 1600 patients during two decades at a single institution. J Am Coll Surg. 2010;210(744–52):752–5.
Adam R, Hagopian EJ, Linhares M, et al. A comparison of percutaneous cryosurgery and percutaneous radiofrequency for unresectable hepatic malignancies. Arch Surg. 2002;137:1332–9 (discussion 1340).
Iannitti DA, Martin RC, Simon CJ, et al. Hepatic tumor ablation with clustered microwave antennae: the US phase II trial. HPB Oxford. 2007;9:120–4.
Kingham TP, Karkar AM, D’Angelica MI, et al. Ablation of perivascular hepatic malignant tumors with irreversible electroporation. J Am Coll Surg. 2012;215:379–87.
Leung U, Kuk D, D’Angelica MI, et al. Long-term outcomes following microwave ablation for liver malignancies. Br J Surg. 2015;102:85–91.
Franzese C, Comito T, Clerici E, et al. Liver metastases from colorectal cancer: propensity score-based comparison of stereotactic body radiation therapy vs. microwave ablation. J Cancer Res Clin Oncol. 2018;144:1777–83.
Palma DA, Olson R, Harrow S, et al. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet. 2019;393:2051–8.
Groeschl RT, Pilgrim CH, Hanna EM, et al. Microwave ablation for hepatic malignancies: a multiinstitutional analysis. Ann Surg. 2014;259:1195–200.
Correa-Gallego C, Fong Y, Gonen M, et al. A retrospective comparison of microwave ablation vs. radiofrequency ablation for colorectal cancer hepatic metastases. Ann Surg Oncol. 2014;21:4278–83.
Takahashi H, Kahramangil B, Kose E, et al. A comparison of microwave thermosphere versus radiofrequency thermal ablation in the treatment of colorectal liver metastases. HPB Oxford. 2018;20:1157–62.
Sun Y, Cheng Z, Dong L, et al. Comparison of temperature curve and ablation zone between 915- and 2450-MHz cooled-shaft microwave antenna: results in ex vivo porcine livers. Eur J Radiol. 2012;81:553–7.
Curto S, Taj-Eldin M, Fairchild D, et al. Microwave ablation at 915 MHz vs 2.45 GHz: a theoretical and experimental investigation. Med Phys. 2015;42:6152–61.
Martin RC, Scoggins CR, McMasters KM. Safety and efficacy of microwave ablation of hepatic tumors: a prospective review of a 5-year experience. Ann Surg Oncol. 2010;17:171–8.
Abdalla EK, Vauthey JN, Ellis LM, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg. 2004;239:818–25 (discussion 825–7).
Ardito F, Panettieri E, Vellone M, et al. The impact of R1 resection for colorectal liver metastases on local recurrence and overall survival in the era of modern chemotherapy: an analysis of 1428 resection areas. Surgery. 2019;165:712–20.
Zhou B, Fine J, Latouche A, et al. Competing risks regression for clustered data. Biostatistics. 2012;13:371–83.
Abreu de Carvalho LF, Logghe B, Van Cleven S, et al. Local control of hepatocellular carcinoma and colorectal liver metastases after surgical microwave ablation without concomitant hepatectomy. Langenbecks Arch Surg. 2021;406:2749–57.
Simo KA, Tsirline VB, Sindram D, et al. Microwave ablation using 915-MHz and 2.45-GHz systems: What are the differences? HPB Oxford. 2013;15:991–6.
Acknowledgement
This study was supported by NIH/NCI Cancer Center Support Grant P30CA008748 at Memorial Sloan Kettering Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karagkounis, G., McIntyre, S.M., Wang, T. et al. Rates and Patterns of Recurrence After Microwave Ablation of Colorectal Liver Metastases: A Per Lesion Analysis of 416 Tumors in the Era of 2.45 GHz Generators. Ann Surg Oncol 30, 6571–6578 (2023). https://doi.org/10.1245/s10434-023-13751-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13751-6